Abstract
Purpose
To analyze donor oocyte (DE) data across 6 years for oocyte usage efficiency, trends, and whether changes impacted outcomes.
Methods
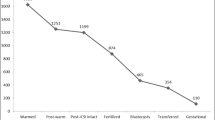
From 2014 to 2019, 323 DE embryo transfers were completed in 200 recipients using oocytes derived of 163 donors. We assessed data for oocytes being freshly retrieved (FRESH-EGG) vs. purchased frozen (FROZEN-EGG); embryos transferred fresh (FRESH-ET) vs. frozen (FROZEN-ET); cycles SHARED (two recipients) vs. SOLE (one recipient); single (SET) vs. double (DET) embryo transfers and usage of PGT-A. Primary outcome was ongoing pregnancy plus live birth (OP/LB) rate.
Results
A total of 229 FRESH-EGG (70%) and 94 FROZEN-EGG (30%) cycles were completed. Overall, the use of FRESH-EGG yielded a higher OP/LB compared to FROZEN-EGG (49% vs. 30%, p = 0.001); within the FRESH-EGG group, OP/LB was similar when comparing FRESH-ET vs. FROZEN-ET (58% vs. 45%, p = 0.07). Within the FRESH-ET group, those using FRESH-EGG had a higher OP/LB than those using FROZEN-EGG (58% vs. 27%, p < 0.001). SHARED vs. SOLE cycles (p = 0.6), donor age (21–32 years; p = 0.4), and age of intended parents (maternal p = 0.3, paternal p = 0.2) did not significantly impact OP/LB. Notably, the use of PGT-A did not improve odds for an OP/LB (p = 0.7).
Conclusion
The use of FRESH-EGG with FRESH-ET without PGT-A remains superior to newer DE treatment combinations. Specifically, the use of FROZEN-EGG and PGT-A did not improve outcomes. Although changing DE practices may enhance experience and affordability, patients and providers must appreciate that choices do not always favorably impact success. Additionally, newly available genetic-ancestry testing may pose longer-term ramifications mandating change in treatment and/or counseling.
Similar content being viewed by others
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable
References
Sauer JL. Competing interests and gamete donation: the case for anonymity. Seton Hall Law Rev. 2009;39(3):919–54.
Centers for Disease Control and Prevention. Assisted Reproductive Technology national summary report. US Dept of Health. 2018
Coates A, Bankowski BJ, Kung A, Griffin DK, Munne S. Differences in pregnancy outcomes in donor egg frozen embryo transfer (Fet) cycles following preimplantation genetic screening (Pgs): a single center retrospective study. J Assist Reprod Genet. 2017;34(1):71–8.
Kushnir VA, Gleicher N. Fresh versus cryopreserved oocyte donation. Curr Opin Endocrinol Diabetes Obes. 2016;23(6):451–7.
Kushnir VA, Darmon SK, Barad DH, Gleicher N. New national outcome data on fresh versus cryopreserved donor oocytes. J Ovarian Res. 2018;11(1):2.
Masbou AK, Friedenthal JB, McCulloh DH, et al. A comparison of pregnancy outcomes in patients undergoing donor egg single embryo transfers with and without preimplantation genetic testing. Reprod Sci. 2019;26(12):1661–5.
Roeca C, Johnson R, Carlson N, Polotsky AJ. Preimplantation genetic testing and chances of a healthy live birth amongst recipients of fresh donor oocytes in the United States. J Assist Reprod Genet. 2020;37(9):2283–92.
Barad DH, Darmon SK, Kushnir VA, Albertini DF, Gleicher N. Impact of preimplantation genetic screening on donor oocyte-recipient cycles in the United States. Am J Obstet Gynecol. 2017;217(5):576.e1–8.
Bracewell-Milnes T, Saso S, Bora S, Ismail AM, al-Memar M, Hamed AH, et al. Investigating psychosocial attitudes, motivations and experiences of oocyte donors, recipients and egg sharers: a systematic review. Hum Reprod Update. 2016;22(4):450–65.
Blakemore JK, Voigt P, Schiffman MR, Lee S, Besser AG, Fino ME. Experiences and psychological outcomes of the oocyte donor: a survey of donors post-donation from one center. J Assist Reprod Genet. 2019;36(10):1999–2005.
Insogna IG, Lanes A, Lee MS, Ginsburg ES, Fox JH. Association of fresh embryo transfers compared with cryopreserved-thawed embryo transfers with live birth rate among women undergoing assisted reproduction using freshly retrieved donor oocytes. JAMA. 2021;325(2):156–63.
Roque M, Haahr T, Geber S, Esteves SC, Humaidan P. Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: a systematic review and meta-analysis of reproductive outcomes. Hum Reprod Update. 2019;25(1):2–14.
Wei D, Liu J-Y, Sun Y, Shi Y, Zhang B, Liu JQ, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019;393(10178):1310–8.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril. 2011;96(2):344–8.
Glujovsky D, Dominguez M, Fiszbajn G, Papier S, Lavolpe M, Sueldo C. A shared egg donor program: which is the minimum number of oocytes to be allocated? J Assist Reprod Genet. 2011;28(3):263–7.
Mullin CM, Fino ME, Talebian S, Keegan D, Grifo JA, Licciardi F. Comparison of pregnancy outcomes in anonymous shared versus exclusive donor oocyte in vitro fertilization cycles. Fertil Steril. 2010;93(2):574–8.
Kolibianakis EM, Tournaye H, Osmanagaoglu K, Camus M, van Waesberghe L, van Steirteghem A, et al. Outcome for donors and recipients in two egg-sharing policies. Fertil Steril. 2003;79(1):69–73.
Doyle N, Gainty M, Eubanks A, Doyle J, Hayes H, Tucker M, et al. Donor oocyte recipients do not benefit from preimplantation genetic testing for aneuploidy to improve pregnancy outcomes. Hum Reprod. 2020;35(11):2548–55.
Noyes N, Hampton BS, Berkeley A, Licciardi F, Grifo J, Krey L. Factors useful in predicting the success of oocyte donation: a 3-year retrospective analysis. Fertil Steril. 2001;76(1):92–7.
Yeh JS, Steward RG, Dude AM, Shah AA, Goldfarb JM, Muasher SJ. Pregnancy outcomes decline in recipients over age 44: an analysis of 27,959 fresh donor oocyte in vitro fertilization cycles from the Society for Assisted Reproductive Technology. Fertil Steril. 2014;101(5):1331–6.
Sagi-Dain L, Sagi S, Dirnfeld M. Effect of paternal age on reproductive outcomes in oocyte donation model: a systematic review. Fertil Steril. 2015;104(4):857–865.e1.
McCarter K, Setton R, Chung A, An A, Rosenwaks Z, Spandorfer S. Is increasing paternal age negatively associated with donor oocyte recipient success? A paired analysis using sibling oocytes. Fertil Steril. Published online April 26, 2021.
Practice Committee of the Society for Assisted Reproductive Technology. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901–3.
Klenov VE, Boulet SL, Mejia RB, Kissin DM, Munch E, Mancuso A, et al. Live birth and multiple birth rates in US in vitro fertilization treatment using donor oocytes: a comparison of single-embryo transfer and double-embryo transfer. J Assist Reprod Genet. 2018;35(9):1657–64.
Berntsen S, Larsen EC, la Cour FN, Pinborg A. Pregnancy outcomes following oocyte donation. Best Pract Res Clin Obstet Gynaecol. 2021;70:81–91.
Keegan DA, Krey LC, Chang H-C, Noyes N. Increased risk of pregnancy-induced hypertension in young recipients of donated oocytes. Fertil Steril. 2007;87(4):776–81.
Practice Committee of the American Society for Reproductive Medicine. Repetitive oocyte donation: a committee opinion. Fertil Steril. 2020;113(6):1150–3.
Rotshenker-Olshinka K, Dahan MH. Fertility care in the era of commercial direct-to-consumer home DNA kits: issues to ponder. J Assist Reprod Genet. 2020;37(3):689–92.
Author information
Authors and Affiliations
Contributions
NN and AP designed the study. AP collected and reviewed the data. AP, NN, and MR analyzed the data. AP, SB, MR, and NN were major contributors writing the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
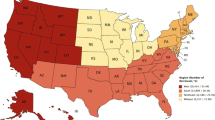
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peyser, A., Brownridge, S., Rausch, M. et al. The evolving landscape of donor egg treatment: success, women’s choice, and anonymity. J Assist Reprod Genet 38, 2327–2332 (2021). https://doi.org/10.1007/s10815-021-02262-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02262-6