Abstract
Purpose
To determine if oocyte denudation and ICSI at 36.5 versus 39 h post HCG and/or Lupron trigger (2.5 h versus 5 h post-oocyte retrieval) influences fertilization and blastulation rates in good prognosis couples
Methods
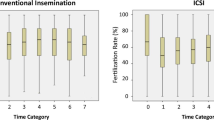
We performed a prospective, randomized controlled trial of 12 patients undergoing IVF with ICSI at an academic fertility center, resulting in 206 MII oocytes analyzed. At time of retrieval, patients with more than 10 oocytes retrieved had their oocytes randomized into two groups—one group for oocyte denudation and ICSI at 36.5 h post HCG and/or Lupron trigger and the other group for these procedures at 39 h post HCG and/or Lupron trigger (2.5 and 5 h after oocyte retrieval). Primary outcomes were fertilization and blastulation rates.
Results
No difference was observed in fertilization rate, total blastulation rate, or day of blastulation based on timing of denudation and ICSI (all p > 0.05). Multiple regression analyses for fertilization and blastulation controlling for age and BMI revealed no difference in fertilization based on time of ICSI (p = 0.38, 0.71, respectively). A conditional logistic regression to account for multiple oocytes derived from each patient also found no difference in fertilization or blastulation based on timing of ICSI, even when controlling for age and BMI (p = 0.47, 0.59, respectively).
Conclusion(s)
In good prognosis couples, we observed no difference in fertilization or blastulation rates based on timing of ICSI within the currently accepted 2- to 6-h window post-retrieval based on a 34-h trigger. The oocyte appears to have a physiological tolerance for fertilization during this window of time, and variability in the timing of ICSI during this window is unlikely to have an impact on cycle outcome.

Similar content being viewed by others
References
Palermo GD, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of a single spermatozoa into an oocyte. Lancet. 1992;340:17–8.
Hodes-Wertz B, Mullin CM, Adler A, Noyes N, Grifo JA, Berkeley AS. Is intracytoplasmic sperm injection overused? J Urol. 2012;187(2):602–6. https://doi.org/10.1016/j.juro.2011.09.151.
Simopolou M, Giannelou P, Bakas P, Gkoles L, Kalampokas T, Pantos K, et al. Making ICSI safer and more effective: a review of the human oocyte and ICSI practice. In Vivo. 2016;30(4):387–400.
Practice Committees of the American Society for Reproductive Medicine and Society for Assisted Reproductive Technology. Intracytoplasmic sperm injection (ICSI) for non-male factor infertility: a committee opinion. Fertil Steril. 2012;98(6):1395–9.
Boulet SL, Mehta A, Kissin DM, Warner L, Kawwas JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313(3):255–63.
Rubino P, Vigano P, Luddi A, Piomboni P. The ICSI procedure from past to future: a systematic review of the more controversial aspects. Hum Reprod Update. 2016;22(2):194–277.
Eppig JJ, Schultz RM, O’Brien M, Chesnel F. Relationship between the developmental programs controlling nuclear and cytoplasmic maturation of mouse oocytes. Dev Biol. 1994;164:1–9.
Sundstrom P, Nilsson BO. Meiotic and cytoplasmic maturation of oocytes collected in stimulated cycles is asynchronous. Hum Reprod. 1988;3:613–9.
Trounson AO, Mohr LR, Wood C, Leeton JF. Effect of delayed insemination on in-vitro fertilization, culture and transfer of human embryos. J Reprod Fertil. 1982;64:285–94.
Khan I, Staessen C, Van de Abbeel E, Camus M, Wisanto A, Smitz J, et al. Time of insemination and its effect on in-vitro-fertilization, cleavage, and pregnancy rates in GnRH agonist/HMG stimulated cycles. Hum Reprod. 1989;4:921–6.
Reinzi L, Ubaldi F, Anniballo R, Cerulo G, Greco E. Preincubation of human oocytes may improve fertilization and embryo quality after intracytoplasmic sperm injection. Hum Reprod. 1998;13:1014–9.
Aletebi F. Denudation and sperm injection interval timing: impact on outcome of intracytoplasmic sperm injection. Int J Women's Health. 2011;3:99–103.
Hassan HA. Cumulus cell contribution to cytoplasmic maturation and oocyte development competence in vitro. J Assit Reprod Genet. 2001;18:539–43.
Ho JY, Chen MJ, Yi YC, Guu HF, Ho ES. The effect of pre-incubation period of oocytes on nuclear maturity, fertilization rate, embryo quality and pregnancy outcome in IVF and ICSI. J Assist Reprod Genet. 2003;20:348–62.
Isiklar A, Mercan R, Balaban B, Alatas C, Aksoy S, Urman B. Impact of oocyte pre-incubation time on fertilization, embryo quality and pregnancy rate after intracytoplasmic sperm injection. Reprod BioMed Online. 2004;8:682–6.
Patrat C, Kaffel A, Delaroche L, Guibert J, Jounnet P, Epelboin S, et al. Optimal timing for oocyte denudation and intracytoplasmic sperm injection. Obstet Gynecol Int. 2012;2012:403531.
Van de Velde H, De Vos A, Joris H, Nagy ZP, Van Steirteghem AC. Effect of timing of oocyte denudation and micro-injection on survival, fertilization, and embryo quality after intracytoplasmic sperm injection. Hum Reprod. 1998;13:3160–4.
Andrews MM, Fishel SB, Rowe PH, Bery JA, Lisi F, Rinaldi L. Analysis of intracytoplasmic sperm injection procedures related to delayed insemination and ejaculated, epididymal and testicular spermatozoa. Reprod BioMed Online. 2001;2:89–97.
Falcone P, Gambera L, Pisoni M, Lofiego V, De Leo V, Mencaglia L, et al. Correlation between oocyte preincubation time and pregnancy rate after intracytoplasmic sperm injection. Gynecol Endocrinol. 2008;24:295–9.
Mizuno S, Ishikawa Y, Matsumoto H, Sato M, Ida M, Fukada A, et al. The timing of culumus cell removal for intracytoplasmic sperm injection influences the capability of embryonic development. Reprod Med Bio. 2018;18(1):111–7.
Pereira N, Neri QV, Lekovich JP, Palermo GD, Rosenwaks Z. The role of in-vivo and in-vitro maturation time on ooplasmic dysmaturity. Reprod BioMed Online. 2016;32(4):401–6.
Garor R, Shufaro Y, Kotler N, Shefer D, Krasilnikov N, Ben-Haroush A, et al. Prolonging oocyte in vitro culture and handling time does not compensate for a shorter interval from human chorionic gonadotropin administration to oocyte pickup. Fertil Steril. 2015;103:72–5.
Eichenlaub-Ritter U, Chandley AC, Gosden RG. Alterations to the microtubular cytoskeleton and increased disorder of chromosome alignment in spontaneously ovulated mouse oocytes aged in vivo: an immunofluorescence study. Chromosoma. 1986;94:337–45.
Eichenlaub-Ritter U, Stahl A, Luciani JM. The microtubular cytoskeleton and chromosomes of unfertilized human oocytes aged in vitro. Hum Genet. 1988;80:259–64.
Segers I, Adriaenssens T, Coucke W, Cortvrindt R, Smitz J. Timing of nuclear maturation and postovulatory aging in oocytes of in vitro-grown mouse follicles with or without oil overlay. Biol Reprod. 2008;78:859–68.
Kilani S, Cooke S, Chapman M. Time course of meiotic spindle development in MII oocytes. Zygote. 2011 Feb;19(1):55–62.
Cohen Y, Malcov M, Schwartz T, Mey-Raz N, Carmon A, Cohen T, et al. Sindle imaging: a new marker for optimal timing of ICSI? Hum Reprod. 2004;19(3):649–54.
Lee SH, Lee JH, Park YS, Yang KM, Lim CK. Comparison of clinical outcomes between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) in IVF-ICSI split insemination cycles. Clin Exp Reprod Med. 2017;44:96–104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
All procedures performed in this study were in accordance with the ethical standards of the institution (Keck School of Medicine of the University of Southern California Institutional Review Board).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smith, M.B., Ho, J.R., Cortessis, V. et al. What is the optimal timing of intracytoplasmic sperm injection (ICSI) after EGG retrieval? A randomized controlled trial. J Assist Reprod Genet 38, 2151–2156 (2021). https://doi.org/10.1007/s10815-021-02216-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02216-y