Abstract
Objective
To investigate whether minimal ovarian stimulation (mOS) is as effective as conventional ovarian stimulation (cOS) for older women belonging to different groups according to the Poseidon criteria.
Material and methods
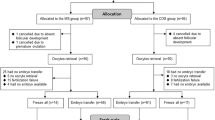
Observational retrospective multicentre cohort including women from Poseidon’s groups 2 and 4 that underwent in vitro fertilization (IVF). We performed a mixed-effects logistic regression model, adding as a random effect the patients and the stimulation cycle considering the dependence of data. Survival curves were employed as a measure of the cumulative live birth rate (CLBR). The primary outcomes were live birth rate per embryo transfer and CLBR per consecutive embryo transfer and oocyte consumed until a live birth was achieved.
Results
A total of 2002 patients underwent 3056 embryo transfers (mOS = 497 and cOS = 2559). The live birth rates per embryo transfer in mOS and cOS showed no significant difference in both Poseidon’s groups. Likewise, the logistic regression showed similar live birth rates between the two protocols in Poseidon’s groups 2 (OR 1.165, 95% CI 0.77–1.77; p = 0.710) and 4 (OR 1.264 95% CI 0.59–2.70; p = 0.387). However, the survival curves showed higher CLBR per oocyte in women that received mOS (Poseidon group 2: p < 0.001 and Poseidon group 4: p = 0.039).
Conclusions
Minimal ovarian stimulation is a good alternative to COS as a first-line treatment for patients belonging to Poseidon’s groups 2 and 4. The number of oocytes needed to achieve a live birth seems inferior in mOS strategy than cOS.




Similar content being viewed by others
Change history
30 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10815-021-02208-y
References
Errazuriz J, Drakopoulos P, Pening D, Racca A, Romito A, De Munck N, et al. Pituitary suppression protocol among Bologna poor responders undergoing ovarian stimulation using corifollitropin alfa: does it play any role? Reprod BioMed Online. 2019;38(6):1010–7.
Vaiarelli A, Cimadomo D, Ubaldi N, Rienzi L, Ubaldi FM. What is new in the management of poor ovarian response in IVF? Curr Opin Obstet Gynecol. 2018 Jun;30(3):155–62.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24.
Papathanasiou A, Searle BJ, King NM, Bhattacharya S. Trends in ‘poor responder’ research: lessons learned from RCTs in assisted conception. Hum Reprod Update. 2016;22(3):306–19.
Boza A, Oguz SY, Misirlioglu S, Yakin K, Urman B. Utilization of the Bologna criteria: a promise unfulfilled? A review of published and unpublished/ongoing trials. Fertil Steril. 2018;109(1):104–109.e2.
Venetis CA. The Bologna criteria for poor ovarian response: the good, the bad and the way forward. Hum Reprod. 2014;29(9):1839–41.
Poseidon Group (Patient-Oriented Strategies Encompassing IndividualizeD Oocyte Number), Alviggi C, Andersen CY, Buehler K, Conforti A, De Placido G, et al. A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil Steril. 2016;105(6):1452–3.
Esteves SC, Roque M, Bedoschi GM, Conforti A, Humaidan P, Alviggi C. Defining low prognosis patients undergoing assisted reproductive technology: POSEIDON criteria-the why. Front Endocrinol (Lausanne). 2018;9:461.
Ubaldi F, Vaiarelli A, D’Anna R, Rienzi L. Management of poor responders in IVF: is there anything new? Biomed Res Int. 2014;2014:352098.
Bastu E, Buyru F, Ozsurmeli M, Demiral I, Dogan M, Yeh J. A randomized, single-blind, prospective trial comparing three different gonadotropin doses with or without addition of letrozole during ovulation stimulation in patients with poor ovarian response. Eur J Obstet Gynecol Reprod Biol. 2016;203:30–4.
Haas J, Zilberberg E, Machtinger R, Kedem A, Hourvitz A, Orvieto R. Do poor-responder patients benefit from increasing the daily gonadotropin dose during controlled ovarian hyperstimulation for IVF? Gynecol Endocrinol. 2015;31(1):79–82.
Nagels HE, Rishworth JR, Siristatidis CS, Kroon B. Androgens (dehydroepiandrosterone or testosterone) for women undergoing assisted reproduction. Cochrane Database Syst Rev. 2015;26(11):CD009749.
Mak SM, Wong WY, Chung HS, Chung PW, Kong GW, Li TC, et al. Effect of mid-follicular phase recombinant LH vs urinary HCG supplementation in poor ovarian responders undergoing IVF-a prospective double-blinded randomized study. Reprod BioMed Online. 2017;34(3):258–66.
Cozzolino M. Growth hormone supplementation in women who are not poor responders. J Assist Reprod Genet. 2021. https://doi.org/10.1007/s10815-021-02166-5.
Cozzolino M, Cecchino GN, Troiano G, Romanelli C. Growth hormone cotreatment for poor responders undergoing in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril 2020;15.
Kamath MS, Maheshwari A, Bhattacharya S, Lor KY, Gibreel A. Oral medications including clomiphene citrate or aromatase inhibitors with gonadotropins for controlled ovarian stimulation in women undergoing in vitro fertilisation. Cochrane Database Syst Rev. 2017;11:CD008528.
Cozzolino M, Franasiak J, Andrisani A, Ambrosini G, Vitagliano A. “Delayed start” gonadotropin-releasing hormone antagonist protocol in Bologna poor-responders: a systematic review and meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2020 Jan;244:154–62.
Tutuncu L, Dundar O. Increasing the stimulation dose of rFHS in unexpected poor responders is not associated with better IVF outcome. Ginekol Pol. 2012 Feb;83(2):111–5.
Youssef MA, van Wely M, Al-Inany H, Madani T, Jahangiri N, Khodabakhshi S, et al. A mild ovarian stimulation strategy in women with poor ovarian reserve undergoing IVF: a multicenter randomized non-inferiority trial. Hum Reprod. 2017;32(1):112–8.
Practice Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm.orgComparison of pregnancy rates for poor responders using IVF with mild ovarian stimulation versus conventional IVF: a guideline. Fertil Steril. 2018;109(6):993–9.
Labarta E, Marin D, Remohi J, Bosch E. Conventional versus minimal ovarian stimulation: an intra-patient comparison of ovarian response in poor-responder women according to Bologna Criteria. Reprod BioMed Online. 2018;37(4):434–41.
Sophonsritsuk A, Choktanasiri W, Weerakiet S, Rojanasakul A. Comparison of outcomes and direct cost between minimal stimulation and conventional protocols on ovarian stimulation in in vitro fertilization. J Obstet Gynaecol Res. 2005;31(5):459–63.
Cozzolino M, Hervas I, Rivera-Egea R, Pellicer A, Garrido N. Do donor spermatozoa improve reproductive outcomes after oocyte donation failure? A retrospective analysis of cumulative live birth rates per donor oocyte consumed. Reprod Biomed Online 2021 Jan 16.
Cruz M, Alama P, Munoz M, Collado D, Blanes C, Solbes E, et al. Economic impact of ovarian stimulation with corifollitropin alfa versus conventional daily gonadotropins in oocyte donors: a randomized study. Reprod BioMed Online. 2017;34(6):605–10.
Nargund G, Fauser BC, Macklon NS, Ombelet W, Nygren K, Frydman R, et al. The ISMAAR proposal on terminology for ovarian stimulation for IVF. Hum Reprod. 2007;22(11):2801–4.
Branigan EF, Estes MA. Minimal stimulation IVF using clomiphene citrate and oral contraceptive pill pretreatment for LH suppression. Fertil Steril. 2000;73(3):587–90.
Teramoto S, Kato O. Minimal ovarian stimulation with clomiphene citrate: a large-scale retrospective study. Reprod BioMed Online. 2007;15(2):134–48.
Klinkert ER, Broekmans FJ, Looman CW, Habbema JD, te Velde ER. Expected poor responders on the basis of an antral follicle count do not benefit from a higher starting dose of gonadotrophins in IVF treatment: a randomized controlled trial. Hum Reprod. 2005;20(3):611–5.
Youssef MA, van Wely M, Mochtar M, Fouda UM, Eldaly A, El Abidin EZ, et al. Low dosing of gonadotropins in in vitro fertilization cycles for women with poor ovarian reserve: systematic review and meta-analysis. Fertil Steril. 2018;109(2):289–301.
Datta AK, Maheshwari A, Felix N, Campbell S, Nargund G. Mild versus conventional ovarian stimulation for IVF in poor responders: a systematic review and meta-analysis. Reprod Biomed Online 2020;14.
Lazer T, Dar S, Shlush E, Al Kudmani BS, Quach K, Sojecki A, et al. Comparison of IVF outcomes between minimal stimulation and high-dose stimulation for patients with poor ovarian reserve. Int J Reprod Med. 2014;2014:581451.
Mansour R, Aboulghar M, Serour GI, Al-Inany HG, Fahmy I, Amin Y. The use of clomiphene citrate/human menopausal gonadotrophins in conjunction with GnRH antagonist in an IVF/ICSI program is not a cost effective protocol. Acta Obstet Gynecol Scand. 2003;82(1):48–52.
Mohsen IA, El Din RE. Minimal stimulation protocol using letrozole versus microdose flare up GnRH agonist protocol in women with poor ovarian response undergoing ICSI. Gynecol Endocrinol. 2013;29(2):105–8.
Yoo JH, Cha SH, Park CW, Kim JY, Yang KM, Song IO, et al. Comparison of mild ovarian stimulation with conventional ovarian stimulation in poor responders. Clin Exp Reprod Med. 2011;38(3):159–63.
Revelli A, Chiado A, Dalmasso P, Stabile V, Evangelista F, Basso G, et al. “Mild” vs. “long” protocol for controlled ovarian hyperstimulation in patients with expected poor ovarian responsiveness undergoing in vitro fertilization (IVF): a large prospective randomized trial. J Assist Reprod Genet. 2014;31(7):809–15.
Pilehvari S, ShahrokhTehraninejad E, Hosseinrashidi B, Keikhah F, Haghollahi F, Aziminekoo E. Comparison pregnancy outcomes between minimal stimulation protocol and conventional GnRH antagonist protocols in poor ovarian responders. J Family Reprod Health. 2016;10(1):35–42.
Peluso C, Oliveira R, Laporta GZ, Christofolini DM, Fonseca FLA, Lagana AS, et al. Are ovarian reserve tests reliable in predicting ovarian response? Results from a prospective, cross-sectional, single-center analysis. Gynecol Endocrinol. 2020;2:1–9.
Di Paola R, Garzon S, Giuliani S, Lagana AS, Noventa M, Parissone F, et al. Are we choosing the correct FSH starting dose during controlled ovarian stimulation for intrauterine insemination cycles? Potential application of a nomogram based on woman’s age and markers of ovarian reserve. Arch Gynecol Obstet. 2018;298(5):1029–35.
Ragni G, Levi-Setti PE, Fadini R, Brigante C, Scarduelli C, Alagna F, et al. Clomiphene citrate versus high doses of gonadotropins for in vitro fertilisation in women with compromised ovarian reserve: a randomised controlled non-inferiority trial. Reprod Biol Endocrinol. 2012;10 114-7827-10-114.
van Tilborg TC, Torrance HL, Oudshoorn SC, Eijkemans MJC, Koks CAM, Verhoeve HR, et al. Individualized versus standard FSH dosing in women starting IVF/ICSI: an RCT. Part 1: the predicted poor responder. Hum Reprod. 2017 Dec 1;32(12):2496–505.
Acknowledgements
We would like to thank the Clinical Directors of the participating IVI centers for their contribution to the data of the database analyzed. We would also like to thank Victor Lozoya Garcia for the support in the statistical analysis.
Funding
This study was funded by IVIRMA global. No additional external funding was received for this study.
Author information
Authors and Affiliations
Contributions
MC: study design, data analysis, interpretation, and manuscript writing. GNC: manuscript writing, interpretation, critical review, and final manuscript approval. EB and JAGV: critical review and final manuscript approval. NG: statistical analysis, critical review, and final manuscript approval.
Corresponding author
Ethics declarations
Ethics approval
The study received ethical approval on 30 November 2018 by IVI Ethic Committee with the number 1810-FIVI-083-MC.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Images of figures 2 and 3 were inverted.
Rights and permissions
About this article
Cite this article
Cozzolino, M., Cecchino, G.N., Bosch, E. et al. Minimal ovarian stimulation is an alternative to conventional protocols for older women according to Poseidon’s stratification: a retrospective multicenter cohort study. J Assist Reprod Genet 38, 1799–1807 (2021). https://doi.org/10.1007/s10815-021-02185-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02185-2