Abstract
Purpose
The aim of this study was to evaluate the outcomes of frozen oocytes or embryos cryopreserved after controlled ovarian stimulation (COS) or in vitro maturation (IVM) for female cancer patients who underwent a fertility preservation (FP) prior to gonadotoxic therapy.
Methods
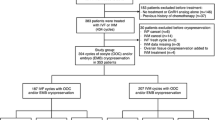
A retrospective cohort study from 2009 to December 2017 was conducted. Among the 667 female cancer patients who underwent oocytes or embryos cryopreservation for FP, 40 (6%) have returned to the fertility clinic between 2011 and 2019 to use their frozen material after being cured. We compared these thaw cycles outcomes according to the techniques used at the time of cryopreservation.
Results
Among the 40 women cancer survivors who used their cryopreserved material, thirty patients have benefited from at least one embryo transfer. Ten patients did not have an embryo transfer since the oocytes did not survive after the thawing process or because no embryo was obtained after fertilization. We related three live births following FP using IVM (two from frozen oocytes and one after embryo cryopreservation). Five live births were obtained when COS was performed at the time of FP (one from frozen oocytes and four after embryo cryopreservation).
Conclusions
Our preliminary results, although they are obtained in a small sample, are encouraging and show that different FP techniques can be used in female cancer patients and lead to live births. IVM is one of the options available that does not delay the start of chemotherapy or if ovarian stimulation using gonadotropins is contraindicated.

Similar content being viewed by others
Data availability
Not applicable
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Binder-Foucard F, Belot A, Delafosse P, Remontet L, Woronoff AS, Bossard N. Estimation nationale de l’incidence et de la mortalité par cancer en France entre 1980 et 2012 : étude à partir des registres des cancers du réseau Francim. Partie 1 - Tumeurs solides [Internet]. Institut de veille sanitaire; 2013 [cited 2020 Sep 26]. Available from: https://hal.archives-ouvertes.fr/hal-02084700
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–87.
Donnez J, Dolmans M-M. Fertility preservation in women. Nat Rev Endocrinol. 2013;9:735–49.
Reh AE, Lu L, Weinerman R, Grifo J, Krey L, Noyes N. Treatment outcomes and quality-of-life assessment in a university-based fertility preservation program: results of a registry of female cancer patients at 2 years. J Assist Reprod Genet. 2011;28:635–41.
Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009;15:587–97.
Gracia CR, Sammel MD, Freeman E, Prewitt M, Carlson C, Ray A, et al. Impact of cancer therapies on ovarian reserve. Fertil Steril. 2012;97:134–140.e1.
Spears N, Lopes F, Stefansdottir A, Rossi V, De Felici M, Anderson RA, et al. Ovarian damage from chemotherapy and current approaches to its protection. Hum Reprod Update. 2019;25(6):673–93.
Dolmans M-M, Lambertini M, Macklon KT, Almeida Santos T, Ruiz-Casado A, Borini A, et al. EUropean REcommendations for female FERtility preservation (EU-REFER): a joint collaboration between oncologists and fertility specialists. Critical Reviews in Oncology/Hematology. 2019;138:233–40.
Ethics Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm.org. Fertility preservation and reproduction in patients facing gonadotoxic therapies: an Ethics Committee opinion. Fertil Steril. 2018;110:380–6.
Alvarez RM, Ramanathan P. Fertility preservation in female oncology patients: the influence of the type of cancer on ovarian stimulation response. Hum Reprod. 2018;33:2051–9.
Creux H, Monnier P, Son W-Y, Buckett W. Thirteen years’ experience in fertility preservation for cancer patients after in vitro fertilization and in vitro maturation treatments. Journal of Assisted Reproduction and Genetics. 2018;35:583–92.
Noyes N, Melzer K, Druckenmiller S, Fino ME, Smith M, Knopman JM. Experiences in fertility preservation: lessons learned to ensure that fertility and reproductive autonomy remain options for cancer survivors. J Assist Reprod Genet. 2013;30:1263–70.
Delattre S, Segers I, Van Moer E, Drakopoulos P, Mateizel I, Enghels L, et al. Combining fertility preservation procedures to spread the eggs across different baskets: a feasibility study. Hum Reprod. 2020;35:2524–36.
Michaan N, Ben-David G, Ben-Yosef D, Almog B, Many A, Pauzner D, et al. Ovarian stimulation and emergency in vitro fertilization for fertility preservation in cancer patients. Eur J Obstet Gynecol Reprod Biol. 2010;149:175–7.
Cardozo ER, Thomson AP, Karmon AE, Dickinson KA, Wright DL, Sabatini ME. Ovarian stimulation and in-vitro fertilization outcomes of cancer patients undergoing fertility preservation compared to age matched controls: a 17-year experience. J Assist Reprod Genet. 2015;32:587–96.
Oktay K, Turan V, Bedoschi G, Pacheco FS, Moy F. Fertility preservation success subsequent to concurrent aromatase inhibitor treatment and ovarian stimulation in women with breast cancer. Journal of Clinical Oncology. 2015;33:2424–9.
Robertson AD, Missmer SA, Ginsburg ES. Embryo yield after in vitro fertilization in women undergoing embryo banking for fertility preservation before chemotherapy. Fertil Steril. 2011;95:588–91.
Sabatini ME, Wolkovich AM, Macklin EA, Wright DL, Souter I, Toth TL. Pronuclear embryo cryopreservation experience: outcomes for reducing the risk of ovarian hyperstimulation syndrome and for fertility preservation in cancer patients. J Assist Reprod Genet. 2011;28:279–84.
Johnson LNC, Dillon KE, Sammel MD, Efymow BL, Mainigi MA, Dokras A, et al. Response to ovarian stimulation in patients facing gonadotoxic therapy. Reprod Biomed Online. 2013;26:337–44.
Courbiere B, Decanter C, Bringer-Deutsch S, Rives N, Mirallié S, Pech JC, et al. Emergency IVF for embryo freezing to preserve female fertility: a French multicentre cohort study. Human Reproduction. 2013;28:2381–8.
Dolmans MM, Hollanders de Ouderaen S, Demylle D, Pirard C. Utilization rates and results of long-term embryo cryopreservation before gonadotoxic treatment. Journal of Assisted Reproduction and Genetics. 2015;32:1233–7.
Prasath EB, Chan MLH, Wong WHW, Lim CJW, Tharmalingam MD, Hendricks M, et al. First pregnancy and live birth resulting from cryopreserved embryos obtained from in vitro matured oocytes after oophorectomy in an ovarian cancer patient. Hum Reprod. 2014;29:276–8.
Uzelac PS, Delaney AA, Christensen GL, Bohler HCL, Nakajima ST. Live birth following in vitro maturation of oocytes retrieved from extracorporeal ovarian tissue aspiration and embryo cryopreservation for 5 years. Fertil Steril. 2015;104:1258–60.
Segers I, Bardhi E, Mateizel I, Van Moer E, Schots R, Verheyen G, et al. Live births following fertility preservation using in-vitro maturation of ovarian tissue oocytes. Hum Reprod. 2020;35:2026–36.
Rodrigues P, Marques M, Pimentel S, Rato M, Carvalho P, Correia SC, et al. Oncofertility case report: live birth 10 years after oocyte in vitro maturation and zygote cryopreservation. J Assist Reprod Genet. 2020;37:3089–94.
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500–10.
Yasmin E, Balachandren N, Davies MC, Jones GL, Lane S, Mathur R, et al. Fertility preservation for medical reasons in girls and women: British fertility society policy and practice guideline. Hum Fertil (Camb). 2018;21:3–26.
Cobo A, García-Velasco J, Domingo J, Pellicer A, Remohí J. Elective and onco-fertility preservation: factors related to IVF outcomes. Hum Reprod. 2018;33:2222–31.
Garcia-Velasco JA, Domingo J, Cobo A, Martínez M, Carmona L, Pellicer A. Five years’ experience using oocyte vitrification to preserve fertility for medical and nonmedical indications. Fertil Steril. 2013;99:1994–9.
Martinez M, Rabadan S, Domingo J, Cobo A, Pellicer A, Garcia-Velasco JA. Obstetric outcome after oocyte vitrification and warming for fertility preservation in women with cancer. Reprod Biomed Online. 2014;29:722–8.
Diaz-Garcia C, Domingo J, Garcia-Velasco JA, Herraiz S, Mirabet V, Iniesta I, et al. Oocyte vitrification versus ovarian cortex transplantation in fertility preservation for adult women undergoing gonadotoxic treatments: a prospective cohort study. Fertil Steril. 2018;109:478–485.e2.
Specchia C, Baggiani A, Immediata V, Ronchetti C, Cesana A, Smeraldi A, et al. Oocyte cryopreservation in oncological patients: eighteen years experience of a tertiary care referral center. Front Endocrinol (Lausanne). 2019;10:600.
Sonigo C, Grynberg M. In vitro oocyte maturation for female fertility preservation. Gynecol Obstet Fertil. 2014;42:657–60.
Chian R-C, Cao Y-X. In vitro maturation of immature human oocytes for clinical application. Methods Mol Biol. 2014;1154:271–88.
Son W-Y, Henderson S, Cohen Y, Dahan M, Buckett W. Immature oocyte for fertility preservation. Front Endocrinol (Lausanne). 2019;10:464.
Grynberg M, Mayeur Le Bras A, Hesters L, Gallot V, Frydman N. First birth achieved after fertility preservation using vitrification of in vitro matured oocytes in a woman with breast cancer. Ann Oncol. 2020;31:541–2.
Cakmak H, Katz A, Cedars MI, Rosen MP. Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. 2013;100:1673–80.
Son W-Y, Chung J-T, Chian R-C, Herrero B, Demirtas E, Elizur S, et al. A 38 h interval between hCG priming and oocyte retrieval increases in vivo and in vitro oocyte maturation rate in programmed IVM cycles. Hum Reprod. 2008;23:2010–6.
Chian RC, Buckett WM, Tulandi T, Tan SL. Prospective randomized study of human chorionic gonadotrophin priming before immature oocyte retrieval from unstimulated women with polycystic ovarian syndrome. Hum Reprod. 2000;15:165–70.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83.
Bizet P, Saias-Magnan J, Jouve E, Grillo JM, Karsenty G, Metzler-Guillemain C, et al. Sperm cryopreservation before cancer treatment: a 15-year monocentric experience. Reprod Biomed Online. 2012;24:321–30.
Botchan A, Karpol S, Lehavi O, Paz G, Kleiman SE, Yogev L, et al. Preservation of sperm of cancer patients: extent of use and pregnancy outcome in a tertiary infertility center. Asian J Androl. 2013;15:382–6.
Le Du A, Kadoch IJ, Bourcigaux N, Doumerc S, Bourrier M-C, Chevalier N, et al. In vitro oocyte maturation for the treatment of infertility associated with polycystic ovarian syndrome: the French experience. Hum Reprod. 2005;20:420–4.
Grynberg M, Poulain M, le Parco S, Sifer C, Fanchin R, Frydman N. Similar in vitro maturation rates of oocytes retrieved during the follicular or luteal phase offer flexible options for urgent fertility preservation in breast cancer patients. Hum Reprod. 2016;31:623–9.
Sonigo C, Simon C, Boubaya M, Benoit A, Sifer C, Sermondade N, et al. What threshold values of antral follicle count and serum AMH levels should be considered for oocyte cryopreservation after in vitro maturation? Hum Reprod. 2016;31:1493–500.
Rienzi L, Gracia C, Maggiulli R, LaBarbera AR, Kaser DJ, Ubaldi FM, et al. Oocyte, embryo and blastocyst cryopreservation in ART: systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum Reprod Update. 2017;23:139–55.
Kirchhoff AC, Yi J, Wright J, Warner EL, Smith KR. Marriage and divorce among young adult cancer survivors. Journal of Cancer Survivorship. 2012;6:441–50.
Acknowledgements
With regard to their commitment to patient care, the authors would like to thank all the members of the reproductive medicine center of the Antoine Béclère Hospital and are grateful to couples–patients who consent to the use of their medical data. They also thank Doctor Astrid Finet De Bantel (native English speaker, Mathilde Clinic, Rouen, France) and Doctor Emine Hamza (native English speaker, Antoine Beclere Hospital, Clamart, France) for copyediting assistance.
Code availability
Not applicable
Author information
Authors and Affiliations
Contributions
All authors have been involved in the conception and design, or acquisition of data, or analysis and interpretation of data. A.M., V.P.,V.W., L.H., V.G., and A.B. drafted the manuscript. M.G., C.S., and N.F. revised the article for important intellectual content. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Mayeur, A., Puy, V., Windal, V. et al. Live birth rate after use of cryopreserved oocytes or embryos at the time of cancer diagnosis in female survivors: a retrospective study of ten years of experience. J Assist Reprod Genet 38, 1767–1775 (2021). https://doi.org/10.1007/s10815-021-02168-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02168-3