Abstract
Purpose
As the paradigm shifts towards improving cancer survivorship, an important concern for reproductive-aged women diagnosed with cancer is how their disease and its treatment will affect their future fertility. We sought to characterize pregnancy attempts and outcomes in breast cancer patients following chemotherapy.
Methods
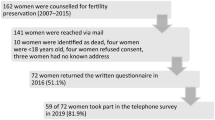
We conducted a prospective cohort study of women diagnosed with breast cancer seen between 2010 and 2019. A questionnaire was administered following cancer treatment with questions regarding oncologic and reproductive history and attempts and method of conception.
Results
Of 181 participants, 46 (25.4%) attempted to conceive following chemotherapy. Thirty-five patients (76.1%) had return of ovarian function. Of those, 34 patients (mean age 32.8 years) first attempted to conceive by intercourse, and 22 (64.7%) became pregnant, resulting in 17 live births. Of the remaining 12 who did not successfully conceive through intercourse, eight went on to try other methods, resulting in five additional pregnancies and one live birth. Twelve patients (mean age 34.6 years) proceeded directly to ART; of those, eight (66.7%) became pregnant, resulting in six live births.
Conclusion
In breast cancer patients with return of ovarian function after chemotherapy, half were able to conceive by intercourse alone. In order to maximize reproductive potential in patients who have return of ovarian function, providers should offer natural conception as a reasonable option prior to the use of cryopreserved tissue. For those who did not attempt to conceive on their own, the use of pre-treatment cryopreserved eggs or embryos had a high likelihood of success.


Similar content being viewed by others
Data availability
We are unable to provide our data due to its identified nature.
References
American Cancer Society. Breast cancer facts & figures (2019-2020). Am Cancer Soc. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breastcancer-facts-and-figures-2019-2020.pdf.2019-2020.pdf2019-2020.pdf.2019-2020.pdf.
Kim HA, Choi J, Park CS, Seong MK, Hong SE, Kim JS, et al. Post-chemotherapy serum anti-Müllerian hormone level predicts ovarian function recovery. Endocr Connect. 2018;7(8):949–56. https://doi.org/10.1530/EC-18-0180.
Yu B, Douglas N, Ferin MJ, Nakhuda GS, Crew K, Lobo RA, et al. Changes in markers of ovarian reserve and endocrine function in young women with breast cancer undergoing adjuvant chemotherapy. Cancer. 2010:NA. https://doi.org/10.1002/cncr.25037.
Henry NL, Xia R, Banerjee M, Gersch C, McConnell D, Giacherio D, et al. Predictors of recovery of ovarian function during aromatase inhibitor therapy. Ann Oncol. 2013;24:2011–6. https://doi.org/10.1093/annonc/mdt149.
Ruddy KJ, O’Neill A, Miller KD, Schneider BP, Baker E, Sparano JA, et al. Biomarker prediction of chemotherapy-related amenorrhea in premenopausal women with breast cancer participating in E5103. Breast Cancer Res Treat. 2014;144:591–7. https://doi.org/10.1007/s10549-014-2891-0.
Letourneau JM, Ebbel EE, Katz PP, Oktay KH, McCulloch CE, Ai WZ, et al. Acute ovarian failure underestimates age-specific reproductive impairment for young women undergoing chemotherapy for cancer. Cancer. 2012;118:1933–9. https://doi.org/10.1002/cncr.26403.
Partridge AH, Ruddy KJ, Gelber S, Schapira L, Abusief M, Meyer M, et al. Ovarian reserve in women who remain premenopausal after chemotherapy for early stage breast cancer. Fertil Steril. 2010;94:638–44. https://doi.org/10.1016/j.fertnstert.2009.03.045.
Silva C, Caramelo O, Almeida-Santos T, Rama ACR. Factors associated with ovarian function recovery after chemotherapy for breast cancer: a systematic review and meta-Analysis. Hum Reprod. 2016;31(12):2737–49. https://doi.org/10.1093/humrep/dew224.
Green DM, Whitton JA, Stovall M, Mertens AC, Donaldson SS, Ruymann FB, et al. Pregnancy outcome of female survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Am J Obstet Gynecol. 2002;187(4):1070–80.
Anderson RA, Brewster DH, Wood R, Nowell S, Fischbacher C, Kelsey TW, et al. The impact of cancer on subsequent chance of pregnancy: a population-based analysis. Hum Reprod. 2018;33(7):1281–90. https://doi.org/10.1093/humrep/dey216.
Van Dorp W, Haupt R, Anderson RA, et al. Reproductive function and outcomes in female survivors of childhood, adolescent, and young adult cancer: a review. J Clin Oncol. 2018;36(21):2169–80. https://doi.org/10.1200/JCO.2017.76.3441.
Lambertini M, Peccatori FA, Demeestere I, Amant F, Wyns C, Stukenborg JB, et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2020;31:1664–78. https://doi.org/10.1016/j.annonc.2020.09.006.
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36(19):1994–2001. https://doi.org/10.1200/JCO.2018.78.1914.
Dabrosin C. An overview of pregnancy and fertility issues in breast cancer patients. Ann Med. 2015;47(8):673–8. https://doi.org/10.3109/07853890.2015.1096953.
Cobo A, García-Velasco J, Domingo J, Pellicer A, Remohí J. Elective and onco-fertility preservation: factors related to IVF outcomes. Hum Reprod. 2018;33(12):1–10. https://doi.org/10.1093/humrep/dey321.
Cobo A, García-Velasco JA, Coello A, Domingo J, Pellicer A, Remohí J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016;105:755–64. https://doi.org/10.1016/j.fertnstert.2015.11.027.
Porcu E, Venturoli S, Damiano G, Ciotti PM, Notarangelo L, Paradisi R, et al. Healthy twins delivered after oocyte cryopreservation and bilateral ovariectomy for ovarian cancer. Reprod BioMed Online. 2008;17(2):265–7. https://doi.org/10.1016/S1472-6483(10)60204-0.
Hartman EK, Eslick GD. The prognosis of women diagnosed with breast cancer before, during and after pregnancy: a meta-analysis. Breast Cancer Res Treat. 2016;160(2):347–60. https://doi.org/10.1007/s10549-016-3989-3.
Iqbal J, Amir E, Rochon PA, Giannakeas V, Sun P, Narod SA. Association of the timing of pregnancy with survival in women with breast cancer. JAMA Oncol. 2017;3(5):659–65. https://doi.org/10.1001/jamaoncol.2017.0248.
Lambertini M, Martel S, Campbell C, Guillaume S, Hilbers FS, Schuehly U, et al. Pregnancies during and after trastuzumab and/or lapatinib in patients with human epidermal growth factor receptor 2–positive early breast cancer: analysis from the NeoALTTO (BIG 1-06) and ALTTO (BIG 2-06) trials. Cancer. 2019;125(2):307–16. https://doi.org/10.1002/cncr.31784.
Lambertini M, Ameye L, Hamy AS, Zingarello A, Poorvu PD, Carrasco E, et al. Pregnancy after breast cancer in patients with germline BRCA mutations. J Clin Oncol. 2020;38:3012–23. https://doi.org/10.1200/JCO.19.02399.
Broekmans FJM, De Ziegler D, Howles CM, Gougeon A, Trew G, Olivennes F. The antral follicle count: practical recommendations for better standardization. Fertil Steril. 2010;3:1044–51. https://doi.org/10.1016/j.fertnstert.2009.04.040.
Poorvu PD, Gelber SI, Zheng Y, Ruddy KJ, Tamimi RM, Peppercorn J, et al. Pregnancy after breast cancer: results from a prospective cohort of young women with breast cancer. Cancer. 2020. https://doi.org/10.1002/cncr.33342.
Lambertini M, Di Maio M, Pagani O, et al. The BCY3/BCC 2017 survey on physicians’ knowledge, attitudes and practice towards fertility and pregnancy-related issues in young breast cancer patients. Breast. 2018;42:41–9. https://doi.org/10.1016/j.breast.2018.08.099.
Lambertini M, Kroman N, Ameye L, Cordoba O, Pinto A, Benedetti G, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst. 2018;110(4):426–9. https://doi.org/10.1093/jnci/djx206.
Pagani O, Ruggeri M, Manunta S, Saunders C, Peccatori F, Cardoso F, et al. Pregnancy after breast cancer: are young patients willing to participate in clinical studies? Breast. 2015;24(3):201–7. https://doi.org/10.1016/j.breast.2015.01.005.
Anderson C, Engel SM, Mersereau JE, Black KZ, Wood WA, Anders CK, et al. Birth outcomes among adolescent and young adult cancer survivors. JAMA Oncol. 2017;3:1078–84. https://doi.org/10.1001/jamaoncol.2017.0029.
Dalberg K, Eriksson J, Holmberg L. Birth outcome in women with previously treated breast cancer-a population-based cohort study from Sweden. PLoS Med. 2006;3:e336. https://doi.org/10.1371/journal.pmed.0030336.
Marklund A, Nasiell J, Berger AS, Fagerberg A, Rodriguez-Wallberg KA. Pregnancy achieved using donor eggs in cancer survivors with treatment-induced ovarian failure: obstetric and perinatal outcome. J Women's Health. 2018;27:939–45. https://doi.org/10.1089/jwh.2017.6703.
Kranick JA, Schaefer C, Rowell S, Desai M, Petrek JA, Hiatt RA, et al. Is pregnancy after breast cancer safe? Breast J. 2010. https://doi.org/10.1111/j.1524-4741.2010.00939.x.
Azim HA, Kroman N, Paesmans M, et al. Prognostic impact of pregnancy after breast cancer according to estrogen receptor status: a multicenter retrospective study. J Clin Oncol. 2013;31:73–9. https://doi.org/10.1200/JCO.2012.44.2285.
Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KA, et al. Adjuvant endocrine therapy for women with hormone receptor–positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2019;37:423–38. https://doi.org/10.1200/JCO.18.01160.
Acknowledgements
We would like to make a special thanks to our nurses and care coordinators who provided patient education and fertility preservation coordination.
Code availability
Code may be made available upon request.
Funding
This study was supported by departmental research funding within the University of California, San Francisco Department of Obstetrics, Gynecology, and Reproductive Sciences. Additionally, this project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number TL1 TR001871.
Author information
Authors and Affiliations
Contributions
M.K.A. and K.W.’s roles included data collection, data analysis, and manuscript writing; N.S. and J.M.L.’s roles included study design and data collection; R.S.’s role included manuscript writing; E.M.L., M.I.C., and M.R.’s roles included study design and manuscript writing.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of California, San Francisco (UCSF) Committee on Human Research and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
As part of the consent process, all participants gave written consent to use de-identified information for research purposes and publications.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abel, M.K., Wald, K., Sinha, N. et al. Conception after chemotherapy: post-chemotherapy method of conception and pregnancy outcomes in breast cancer patients. J Assist Reprod Genet 38, 1755–1765 (2021). https://doi.org/10.1007/s10815-021-02133-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02133-0