Abstract
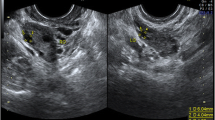
We report the pregnancy and live birth achieved after in vitro maturation (IVM) of oocytes and PGT-A in a 23-year-old patient suffering from ovarian gonadotropin resistance. A woman with resistant ovary syndrome (ROS) had secondary amenorrhea, high FSH levels (25.34 mIU/mL) and LH (29.6 mIU/mL), low estradiol levels (15.2 pg/mL), and high serum AMH levels (38.0 ng/mL), associated with an increased antral follicle count (AFC) of 45. Without gonadotropin priming and HCG trigger, ultrasound-guided transvaginal oocyte retrieval was performed. Aspiration of antral-stage follicles allowed the retrieval of 15 immature oocytes. After oocyte collection, immature oocytes were cultured in the IVM medium. Following IVM, six of them reached metaphase II stage. Resultant matured oocytes were fertilized by intracytoplasmic sperm injection (ICSI). Embryos obtained were cultured to the blastocyst stage. On day 5, three embryos reached blastocyst stage. Trophectoderm biopsy and PGT-A were performed on two better quality embryos on day 5 after fertilization. Two biopsied embryos were reported to be euploid. PGT-A was performed utilizing next-generation sequencing (NGS\MPS). One embryo was transferred in an artificial thaw cycle and resulted in a viable intrauterine pregnancy and live birth. Our experience indicates that there is no requirement for gonadotropin stimulation and use of b-hCG trigger prior to IVM in patients with ROS. The results suggest that oocytes obtained with IVM in patients with ROS are capable of meiotic and mitotic division, fertilization, and generation of euploid embryos. IVM appears to be a valuable approach in patients with ROS, allowing them to have genetically connected offspring.

Similar content being viewed by others
References
Jones GS, De Moraes-Ruehsen M. A new syndrome of amenorrhea in association with hypergonadotropism and apparently normal ovarian follicular apparatus. Am J Obstet Gynecol. 1969;104(4):597–600.
Jequiez AM. Conception in the resistant ovary syndrome occurring during hormone replacement therapy: a report of two cases. Aust N Z J Obstet Gynecol. 1990;30:176–8.
Galvão A, Segers I, Smitz J, Tournaye H, De Vos M. In vitro maturation (IVM) of oocytes in patients with resistant ovary syndrome and in patients with repeated deficient oocyte maturation. J Assist Reprod Genet. 2018;35(12):2161–71. https://doi.org/10.1007/s10815-018-1317-z.
Huhtaniemi I, Alevizaki M. Gonadotropin resistance. Best Pract Res Clin Endocrinol Metab. 2006;20:561–76. https://doi.org/10.1016/j.beem.2006.09.003.
Khor S, Lyu Q, Kuang Y, Lu X. Novel FSHR variants causing female resistant ovary syndrome. Mol Genet Genomic Med. 2019;8(2):e1082. https://doi.org/10.1002/mgg3.1082.
Huhtaniemi IT, Themmen AP. Mutations in human gonadotropin and gonadotropin-receptor genes. Endocrine. 2005;26:207–17. https://doi.org/10.1385/ENDO:26:3:207.
Themmen APN, Huhtaniemi IT. Mutations of gonadotropins and gonadotropin receptors: elucidating the physiology and pathophysiology of pituitary-gonadal function. Endocr Rev. 2000;21:551–83. https://doi.org/10.1210/edrv.21.5.0409.
Conway GS, Conway E, Walker C, Hoppner W, Gromoll J, Simoni M. Mutation screening and isoform prevalence of the follicle stimulating hormone receptor gene in women with premature ovarian failure, resistant ovary syndrome and polycystic ovary syndrome. Clin Endocrinol. 1999;51:97–9. https://doi.org/10.1046/j.1365-2265.1999.00745.x.
Aittomaki K, Lucena JL, Pakarinen P, Sistonen P, Tapanainen J, Gromoll J, et al. Mutation in the follicle-stimulating hormone receptor gene causes hereditary hypergonadotropic ovarian failure. Cell. 1995;82:959–68. https://doi.org/10.1016/0092-8674(95)90275-9.
Haller-Kikkatalo K, Salumets A, Uibo R. Review on autoimmune reactions in female infertility: antibodies to follicle stimulating hormone. Clin Dev Immunol. 2012;2012:762541. https://doi.org/10.1155/2012/762541.
Rogenhofer N, Pavlik R, Jeschke U, Wypior G, Ochsenkühn R, Thaler CJ. Effective ovarian stimulation in a patient with resistant ovary syndrome and antigonadotropin antibodies. Am J Reprod Immunol. 2015;73:185–91. https://doi.org/10.1111/aji.12306.
Meyer WR, Lavy G, DeCherney AH, Visintin I, Economy K, Luborsky JL. Evidence of gonadal and gonadotropin antibodies in women with a suboptimal ovarian response to exogenous gonadotropin. Obstet Gynecol. 1990;75:795–9.
Tucker EJ, Grover SR, Bachelot A, Touraine P, Sinclair AH. Premature ovarian insufficiency: new perspectives on genetic cause and phenotypic spectrum. Endocr Rev. 2016;37(6):609–35. https://doi.org/10.1210/er.2016-1047.
De Vos M, Smitz J, Thompson JG, Gilchrist RB. The definition of IVM is clear - variations need defining. Hum Reprod. 2016;31:2411–5. https://doi.org/10.1093/humrep/dew208.
Grynberg M, Peltoketo H, Christin-Maître S, Poulain M, Bouchard P, Fanchin R. First birth achieved after in vitro maturation of oocytes from a woman endowed with multiple antral follicles unresponsive to follicle-stimulating hormone. J Clin Endocrinol Metab. 2013;98:4493–8. https://doi.org/10.1210/jc.2013-1967.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocyst. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: infertility and genetics beyond. Carnforth: Parthenon Press; 1999. p. 378–88.
Li Y, Pan P, Yuan P, Qiu Q, Yang D. Successful live birth in a woman with resistant ovary syndrome following in vitro maturation of oocytes. J Ovarian Res. 2016;9:1–6. https://doi.org/10.1186/s13048-016-0263-6.
Flageole C, Toufaily C, Bernard DJ, Ates S, Blais V, Chénier S, et al. Successful in vitro maturation of oocytes in a woman with gonadotropin-resistant ovary syndrome associated with a novel combination of FSH receptor gene variants: a case report. J Assist Reprod Genet. 2019;36(3):425–32. https://doi.org/10.1007/s10815-018-1394-z.
Practice Committees of the American Society for Reproductive. M, the Society for Assisted Reproductive T. In vitro maturation: a committee opinion. Fertil Steril. 2013;99:663–6.
Hyman JH, Sokal-Arnon T, Son WY, Tan SL, Dahan MH. Live birth of twins after performing early hCG administration as a modification of natural cycle in vitro fertilization, in a women with decreased ovarian reserve. Arch Gynecol Obstet. 2015;291:219–22. https://doi.org/10.1007/s00404-014-3371-9.
Son WY, Chung JT, Dahan M, Reinblatt S, Tan SL, Holzer H. Comparison of fertilization and embryonic development in sibling in vivo matured oocytes retrieved from different sizes follicles from in vitro maturation cycles. J Assist Reprod Genet. 2011;28:539–44. https://doi.org/10.1007/s10815-010-9527-z.
Son WY, Chung JT, Herrero B, Dean N, Demirtas E, Holzer H, et al. Selection of the optimal day for oocyte retrieval based on the diameter of the dominant follicle in hCG-primed in vitro maturation cycles. Hum Reprod. 2008;23:2680–5. https://doi.org/10.1093/humrep/den332.
Klenov VE, Boulet SL, Mejia RB, et al. Live birth and multiple birth rates in US in vitro fertilization treatment using donor oocytes: a comparison of single-embryo transfer and double-embryo transfer. J Assist Reprod Genet. 2018;35(9):1657–64. https://doi.org/10.1007/s10815-018-1243-0.
Spits C, Guzman L, Mertzanidou A, Jacobs K, Ortega-Hrepich C, Gilchrist RB, et al. Chromosome constitution of human embryos generated after in vitro maturation including 3-isobutyl-1-methylxanthine in the oocyte collection medium. Hum Reprod. 2015;30(3):653–63. https://doi.org/10.1093/humrep/deu329.
Mostinckx L, Segers I, Belva F, Buyl R, Santos-Ribeiro S, Blockeel C, et al. Obstetric and neonatal outcome of assisted reproductive technology (ART) in patients with polycystic ovaries (PCO): in vitro maturation (IVM) of oocytes versus controlled ovarian stimulation. Hum Reprod. 2019;34:1595–607. https://doi.org/10.1093/humrep/dez086.
Belva F, Roelants M, Vermaning S, Desmyttere S, De Schepper J, Bonduelle M, et al. Growth and other health outcomes of 2-year-old singletons born after IVM versus controlled ovarian stimulation in mothers with polycystic ovary syndrome. Hum Reprod Open. 2020;10(1):hoz043. https://doi.org/10.1093/hropen/hoz043.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Kornilov Nikolai, Pavlova Marina, and Yakovlev Pavel. The first draft of the manuscript was written by Yakovlev Pavel and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical approval is required. Informed consent was obtained from participant included in the study.
Consent for publication
The participant has consented to the submission of the case report to the journal.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kornilov, N.V., Pavlova, M.N. & Yakovlev, P.P. The live birth in a woman with resistant ovary syndrome after in vitro oocyte maturation and preimplantation genetic testing for aneuploidy. J Assist Reprod Genet 38, 1303–1309 (2021). https://doi.org/10.1007/s10815-021-02085-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02085-5