Abstract
Purpose
The aim of this study was to elucidate whether ovarian tissue is able to withstand a double freezing-thawing procedure.
Methods
Human ovarian cortical biopsies from 4 thawed whole ovaries were divided into 4 experimental subgroups: (a) frozen-thawed non-grafted group, (b) frozen-thawed xenografted group, (c) refrozen-rethawed non-grafted group, and (d) refrozen-rethawed xenografted group. Xenografting was performed using 8 severe combined immunodeficient mice for a total duration of 21 days. The following analyses were conducted: classic hematoxylin and eosin staining, Ki67 immunolabeling, transmission electron microscopy, Masson’s green trichrome, and double CD34 immunostaining.
Results
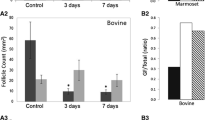
Morphologically normal preantral follicles were detected in all groups. We observed a dramatic decline of more than 65% in early preantral follicle survival rates after grafting of both frozen-thawed (p < 0.0001) and refrozen-rethawed (p < 0.0001) ovarian tissue. However, mean follicle densities remained comparable between the frozen-thawed and refrozen-rethawed non-grafted groups, as well as both grafted groups. Equivalent proportions of proliferating early preantral follicles were identified in frozen-thawed and refrozen-rethawed samples, whether the tissue was grafted or not. Furthermore, we did not observe any significant difference in atretic follicle rates between any of the four groups, and the ultrastructural quality of follicles appeared unaffected by the refreezing procedure. Similar proportions of fibrosis were noted in the frozen-thawed and refrozen-rethawed groups, irrespective of grafting. Finally, no significant differences were witnessed in terms of vascularization.
Conclusion
We were able to demonstrate, for the first time, that refrozen-rethawed ovarian tissue has the same functional characteristics as frozen-thawed ovarian tissue.



Similar content being viewed by others
Data availability
Not applicable.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
Wallace WHB, Anderson RA, Irvine S. Fertility preservation for young patients with cancer: who is at risk and what can be offered? Lancet. 2005;6:209–18.
Meirow D, Biederman H, Anderson RA, Wallace WH. Toxicity of chemotherapy and radiation on female reproduction. Clin Obstet Gynecol. 2010;53:727–39.
Donnez J, Dolmans MM. Fertility preservation in women. N Engl J Med. 2017;377:1657–65.
Hossay C, Dolmans MM. Fertility preservation in women before cancer therapy. Belg J Hematol. 2020;11:44–8.
Donnez J, Dolmans MM. Fertility preservation in women. Nat Rev Endocrinol. 2013;9:735–49.
Wallace WHB, Smith AG, Kelsey TW, Edgar AE, Anderson RA. Fertility preservation for girls and young women with cancer: population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol. 2014;15:1129–36.
Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18:483–91.
Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022–33.
Manavella DD, Cacciottola L, Payen VL, Amorim CA, Donnez J, Dolmans MM. Adipose tissue-derived stem cells boost vascularization in grafted ovarian tissue by growth factor secretion and differentiation into endothelial cell lineages. Mol Hum Reprod. 2019;25:184–93.
Rivas Leonel EC, Lucci CM, Amorim CA. Cryopreservation of human ovarian tissue: a review. Transfus Med Hemother. 2019;46:173–81.
Jeve YB, Gelbaya T, Fatum M. Time to consider ovarian tissue cryopreservation for girls with Turner’s syndrome: an opinion paper. Hum Reprod Open. 2019;2019(3):hoz016.
Peek R, Schleedoorn M, Smeets D, van de Zande G, Groenman F, Braat D, et al. Ovarian follicles of young patients with Turner’s syndrome contain normal oocytes but monosomic 45,X granulosa cells. Hum Reprod. 2019;34:1686–96.
Soares M, Saussoy P, Maskens M, Reul H, Amorim CA, Donnez J, et al. Eliminating malignant cells from cryopreserved ovarian tissue is possible in leukaemia patients. Br J Haematol. 2017;178:231–9.
Dolmans MM, Masciangelo R. Risk of transplanting malignant cells in cryopreserved ovarian tissue. Minerva Ginecol. 2018;70:436–43.
Donnez J, Dolmans MM, Demylle D, Jadoul P, Pirard C, Squifflet J, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364(9443):1405–10.
Bedaiwy MA, Jeremias E, Gurunluoglu R, Hussein MR, Siemianow M, Biscotti C, et al. Restoration of ovarian function after autotransplantation of intact frozen-thawed sheep ovaries with microvascular anastomosis. Fertil Steril. 2003;79(3):594–602.
Imhof M, Bergmeister H, Lipovac M, Rudas M, Hofstetter G, Huber J. Orthotopic microvascular reanastomosis of whole cryopreserved ovine ovaries resulting in pregnancy and live birth. Fertil Steril. 2006;85:1208–15.
Courbière B, Caquant L, Mazoyer C, Franck M, Lornage J, Salle B. Difficulties improving ovarian functional recovery by microvascular transplantation and whole ovary vitrification. Fertil Steril. 2009;91(6):2697–706.
Onions VJ, Webb R, McNeilly AS, Campbell BK. Ovarian endocrine profile and long-term vascular patency following heterotopic autotransplantation of cryopreserved whole ovine ovaries. Hum Reprod. 2009;24(11):2845–55.
Arav A, Gavish Z, Elami A, Natan Y, Revel A, Silber S, et al. Ovarian function 6 years after cryopreservation and transplantation of whole sheep ovaries. Reprod BioMed Online. 2010;20:48–52.
Campbell BK, Hernandez-Medrano J, Onions V, Pincott-Allen C, Aljaser F, Fisher J, et al. Restoration of ovarian function and natural fertility following the cryopreservation and autotransplantation of whole adult sheep ovaries. Hum Reprod. 2014;29(8):1749–63.
Torre A, Vertu-Ciolino D, Mazoyer C, Selva J, Lornage J, Salle B. Safeguarding fertility with whole ovary cryopreservation and microvascular transplantation: higher follicular survival with vitrification than with slow freezing in a ewe model. Transplantation. 2016;100(9):1889–97.
Martinez-Madrid B, Dolmans MM, Van Langendonckt A, Defrere S, Donnez J. Freeze-thawing intact human ovary with its vascular pedicle with a passive cooling device. Fertil Steril. 2004;82:1390–4.
Martinez-Madrid B, Camboni A, Dolmans MM, Nottola S, Van Langendonckt A, Donnez J. Apoptosis and ultrastructural assessment after cryopreservation of whole human ovaries with their vascular pedicle. Fertil Steril. 2007;87:1153–65.
Patrizio P, Bromer J, Johnson J, Martel M, Silber S, Arav A. Cryopreservation of eleven whole human ovaries: histology, immunohistochemistry and technical details. Fertil Steril. 2008;90:S38(O-104).
Leporrier M, Von Theobald P, Roffe JL, Muller G. A new technique to protect ovarian function before pelvic irradiation. Cancer. 1987;60:2201–4.
Hilders CG, Baranski AG, Peters L, Ramkhelawan A, Trimbos JB. Successful human ovarian autotransplantation to the upper arm. Cancer. 2004;101:2771–8.
Mhatre P, Mhatre J, Magotra R. Ovarian transplant: a new frontier. Transplant Proc. 2005;37:1396–8.
Silber SJ, Grudzinskas G, Gosden RG. Successful pregnancy after microsurgical transplantation of an intact ovary. N Engl J Med. 2008;359(24):2617–8.
Westphal JR, Gerritse R, Braat DD, Beerendonk CCM, Peek R. Complete protection against cryodamage of cryopreserved whole bovine and human ovaries using DMSO as a cryoprotectant. J Assist Reprod Genet. 2017;34:1217–29.
Jadoul P, Donnez J, Dolmans MM, Squifflet J, Lengele B, Martinez-Madrid B. Laparoscopic ovariectomy for whole human ovary cryopreservation: technical aspects. Fertil Steril. 2007;87:971–5.
Donnez J, Martinez-Madrid B, Jadoul P, Van Langendonckt A, Demylle D, Dolmans MM. Ovarian tissue cryopreservation and transplantation: a review. Hum Reprod Update. 2006;12:519–35.
Dolmans MM, Jadoul P, Gilliaux S, Amorim CA, Luyckx V, Squifflet J, et al. A review of 15 years of ovarian tissue bank activities. J Assist Reprod Genet. 2013;30:305–14.
Nisolle M, Casanas-Roux F, Qu J, Motta P, Donnez J. Histologic and ultrastructural evaluation of fresh and frozen-thawed human ovarian xenografts in nude mice. Fertil Steril. 2000;74:122–9.
Anderson RA, McLaughlin M, Wallace WHB, Albertini DF, Telfer EE. The immature human ovary shows loss of abnormal follicles and increasing follicle developmental competence through childhood and adolescence. Hum Reprod. 2014;29:97–106.
Lass A, Silye R, Abrams DC, Krausz T, Hovatta O, Margara R, et al. Follicular density in ovarian biopsy of infertile women: a novel method to assess ovarian reserve. Hum Reprod. 1997;12:1028–31.
Gougeon A. Regulation of ovarian follicular development in primates: facts and hypotheses. Endocr Rev. 1996;17:121–55.
Luyckx V, Scalercio S, Jadoul P, Amorim CA, Soares M, Donnez J, et al. Evaluation of cryopreserved ovarian tissue from prepubertal patients after long-term xenografting and exogenous stimulation. Fertil Steril. 2013;100:1350–7.
Nottola SA, Camboni A, Van Langendonckt A, Demylle D, Macchiarelli G, Dolmans MM, et al. Cryopreservation and xenotransplantation of human ovarian tissue: an ultrastructural study. Fertil Steril. 2008;90:23–32.
Soares M, Sahrari K, Chiti MC, Amorim CA, Ambroise J, Donnez J, et al. The best source of isolated stromal cells for the artificial ovary: medulla or cortex, cryopreserved or fresh? Hum Reprod. 2015;30:1589–98.
Qu J, Godin PA, Nisolle M, Donnez J. Distribution and epidermal growth factor receptor expression of primordial follicles in human ovarian tissue before and after cryopreservation. Hum Reprod. 2000;15:302–10.
Schmidt KL, Byskov AG, Andersen NA, Muller J, Andersen CY. Density and distribution of primordial follicles in single pieces of cortex from 21 patients and in individual pieces of cortex from three entire human ovaries. Hum Reprod. 2003;18:1158–64.
Gook DA, Edgar DH, Borg J, Archer J, McBain JC. Diagnostic assessment of the developmental potential of human cryopreserved ovarian tissue from multiple patients using xenografting. Hum Reprod. 2005;20:72–8.
Dolmans MM, Martinez-Madrid B, Gadisseux E, Guiot Y, Yuan WY, Torre A, et al. Short-term transplantation of isolated human ovarian follicles and cortical tissue into nude mice. Reprod. 2007;134:253–62.
Gavish Z, Peer G, Roness H, Cohen Y, Meirow D. Follicle activation and ‘burn-out’ contribute to post-transplantation follicle loss in ovarian tissue grafts: the effect of graft thickness. Hum Reprod. 2014;29:989–96.
Gavish Z, Spector I, Peer G, Schlatt S, Wistuba J, Roness H, et al. Follicle activation is a significant and immediate cause of follicle loss after ovarian tissue transplantation. J Assist Reprod Genet. 2018;35:61–9.
Masciangelo R, Hossay C, Donnez J, Dolmans MM. Does the Akt pathway play a role in follicle activation after grafting of human ovarian tissue? Reprod BioMed Online. 2019;39:196–8.
Van den Broecke R, Liu J, Handyside A, Van der Elst JC, Krausz T, Dhont M, et al. Follicular growth in fresh and cryopreserved human ovarian cortical grafts transplanted to immunodeficient mice. Eur J Obstet Gynecol Reprod Biol. 2001;97:193–201.
Van Eyck AS, Jordan BF, Gallez B, Heilier JF, Van Langendonckt A, Donnez J. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. Fertil Steril. 2009;92:374–81.
Camboni A, Martinez-Madrid B, Dolmans MM, Amorim CA, Nottola SA, Donnez J, et al. Preservation of fertility in young cancer patients: contribution of transmission electron microscopy. Reprod BioMed Online. 2008;17:136–50.
Familiari G, Caggiati A, Nottola SA, Ermini M, Di Benedetto MR, Motta PM. Ultrastructure of human ovarian primordial follicles after combination chemotherapy for Hodgkin’s disease. Hum Reprod. 1993;8:2080–7.
de Bruin JP, Dorland M, Spek ER, Posthuma G, van Haaften M, Looman CWN, et al. Ultrastructure of the resting ovarian follicle pool in healthy young women. Biol Reprod. 2002;66:1151–60.
Ohkado A, Hachida M, Furukawa H, Lu H, Hanayama N, Hoshi H, et al. Should the aortic valve homograft be recryopreserved? Ann Thorac Surg. 1998;65:1083–6.
Dath C, Van Eyck AS, Dolmans MM, Romeu L, Delle Vigne L, Donnez J, et al. Xenotransplantation of human ovarian tissue to nude mice: comparison between four grafting sites. Hum Reprod. 2010;25:1734–43.
Israely T, Dafni H, Nevo N, Tsafriri A, Neeman M. Angiogenesis in ectopic ovarian xenotransplantation: multiparameter characterization of the neovasculature by dynamic contrast-enhanced MRI. Magn Reson Med. 2004;52:741–50.
Van Eyck AS, Bouzin C, Feron O, Romeu L, Van Langendonckt A, Donnez J, et al. Both host and graft vessels contribute to revascularization of xenografted human ovarian tissue in murine model. Fertil Steril. 2010;93:1676–85.
Manavella DD, Cacciottola L, Pomme S, Desmet CM, Jordan BF, Donnez J, et al. Two-step transplantation with adipose tissue-derived stem cells increases follicle survival by enhancing vascularization in xenografted frozen-thawed human ovarian tissue. Hum Reprod. 2018;33:1107–16.
Cacciottola L, Manavella DD, Amorim CA, Donnez J, Dolmans MM. In vivo characterization of metabolic activity and oxidative stress in grafted human ovarian tissue using microdialysis. Fertil Steril. 2018;110:534–44.
Roness H, Meirow D. Fertility preservation: follicle reserve loss in ovarian tissue transplantation. Reprod. 2019;158:F35–44.
Acknowledgments
The authors thank Mira Hryniuk for reviewing the English language of the article and Dolores Gonzalez, Olivier Van Kerk, Sarah Storder, and Alberte Lefèvre for their technical assistance. The authors also extend their thanks to Guillaume Courtoy for his assistance with Visiopharm® software.
Funding
This study was supported by grants from the Fonds National de la Recherche Scientifique de Belgique (Télévie grant 7.4602.18F awarded to C.H., F.R.S.-FNRS/FRIA FC29657 awarded to L.C., Télévie grant 7.4590.16 to R.M., 5/4/150/5 grant to M.M.D., EOS grant 30443682 and FNRS-PDR Convention T.0077.14), the Fonds Spéciaux de Recherche, the Foundation Against Cancer (grant 2018-042 awarded to A.C.), and donations from the Ferrero family and Philippe de Spoelberch.
Author information
Authors and Affiliations
Contributions
C.H.: Conception and design of the study, experimental procedures, analysis of results, statistical analysis, and article preparation. A.C.: Experimental procedures, analysis of results, and discussion contribution. L.C.: Experimental procedures and analysis of results and discussion contribution. T.Y.T.N.: Experimental procedures. R.M.: Experimental procedures and analysis of results. J.D.: Data evaluation, discussion contribution, and article revision. M.M.D.: Conception of the study, data evaluation, discussion contribution, and article revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval
The Institutional Review Board of the Université Catholique de Louvain (reference 2012/23MAR/125) approved the use of human ovarian tissue for this study after obtaining written informed consent from all subjects. Animal welfare guidelines were followed, and the protocol was approved by the Committee on Animal Research of the Université Catholique de Louvain (reference 2018/UCL/MD/40).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hossay, C., Camboni, A., Cacciottola, L. et al. Can frozen-thawed human ovary withstand refreezing-rethawing in the form of cortical strips?. J Assist Reprod Genet 37, 3077–3087 (2020). https://doi.org/10.1007/s10815-020-01960-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01960-x