Abstract
Purpose
There is controversy whether teratospermia is associated with poorer IVF outcomes and if ICSI may overcome this deficit. The debate likely lies in study heterogeneity, poor adjustment for confounders, and inter-observer variation in sperm morphology assessment. Given the current literature, a shift in practice was implemented at our center in February 2017, whereby teratospermia was no longer a criterion for ICSI. We hypothesized that, despite decreasing ICSI rates, we would see no change in ART outcomes.
Methods
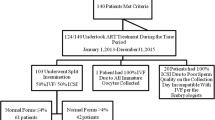
A retrospective study was performed including 1821 couples undergoing IVF/ICSI at a single center from January 2016 to December 2018, divided into cohorts before and after the practice change. The primary outcome of clinical pregnancy and secondary outcomes of fertilization, fertilization failure, good quality blastocyst formation, embryo utilization, positive hCG, and miscarriage rates was compared, adjusting for potential confounders. Subgroup analysis was performed evaluating teratospermia as the only reason for a male factor infertility diagnosis.
Results
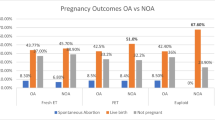
Despite a decrease in ICSI rate of 30.3%, we found no significant difference in clinical intrauterine pregnancy rate, with an adjusted relative risk of 0.93 (0.81, 1.07, P = 0.3008). There were no significant differences in other secondary outcomes after multivariate adjustment. Subgroup analysis for those with male factor infertility due to teratospermia showed no difference in outcomes.
Conclusion
This study concurs with the recent data suggesting that employing ICSI solely for teratospermia is unnecessary. This may allow clinics to decrease ICSI rates without sacrificing success rates, leading to lower cost and risk associated with treatment.

Similar content being viewed by others
References
MacLeod J, Wang Y. Male fertility potential in terms of semen quality: a review of the past, a study of the present. Fertil Steril. 1979;31(2):103–16.
Kruger TF, Menkveld R, Stander FS, Lombard CJ, Van der Merwe JP, van Zyl JA, et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil Steril. 1986;46(6):1118–23.
Grow DR, Oehninger S, Seltman HJ, Toner JP, Swanson RJ, Kruger TF, et al. Sperm morphology as diagnosed by strict criteria: probing the impact of teratospermia on fertilization rate and pregnancy outcome in a large in vitro fertilization population. Fertil Steril. 1994;62(3):559–67.
Guzick DS, Overstreet JW, Factor LP, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001;345:1388–93.
Van der Merwe FH, Kruger TF, Oehninger SC, Lombard CJ. The use of semen parameters to identify the subfertile male in the general population. Gynecol Obstet Investig. 2005;59(2):86–91.
Kruger TF, Haque D, Acosta AA, Pleban P, Swanson RJ, Simmons KF, et al. Correlation between sperm morphology, acrosin, and fertilization in an IVF program. Arch Androl. 1988;20:237–41.
Menkveld R, Stander FSH, Kotze TJVW, Kruger TF, van Zyl JA. The evaluation of morphological characteristics of human spermatozoa according to stricter criteria. Hum Reprod. 1990;5(5):586–92.
Menkveld R, Rhemrev JP, Franken DR, Vermeiden JP, Kruger TF. Acrosomal morphology as a novel criterion for male fertility diagnosis: relation with acrosin activity, morphology (strict criteria), and fertilization in vitro. Fertil Steril. 1996;65(3):637–44.
Coetzee K, Kruger TF, Lombard CJ. Predictive value of normal sperm morphology: a structured literature review. Hum Reprod Update. 1998;4(1):73–82.
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Induction of acrosome reaction in human spermatozoa used for subzonal insemination. Hum Reprod. 1992;7(2):248–54.
Pisarska MD, Casson PR, Cisneros PL, Lamb DJ, Lipshultz LI, Buster JE, et al. Fertilization after standard in vitro fertilization versus intracytoplasmic sperm injection in subfertile males using sibling oocytes. Fertil Steril. 1999;71:627–32.
Plachot M, Belaisch-Allart J, Mayenga JM, Chouraqui A, Tesquier L, Serkine AM. Outcome of conventional IVF and ICSI on sibling oocytes in mild male factor infertility. Hum Reprod. 2002;17:362–9.
Tournaye H, Verheyen G, Albano C, Camus M, Van Landuyt L, Devroey P, et al. Intracytoplasmic sperm injection versus in vitro fertilization: a randomized controlled trial and a meta-analysis of the literature. Fertil Steril. 2002;78:1030–7.
Hotaling JM, Smith JF, Rosen M, Muller CH, Walsh TJ. The relationship between isolated teratospermia and clinical pregnancy after in vitro fertilization with or without intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil Steril. 2011;95(3):1141–5.
Keegan BR, Barton S, Sanchez X, Berkeley AS, Krey LC, Grifo J. Isolated teratospermia does not affect in vitro fertilization outcome and is not an indication for intracytoplasmic sperm injection. Fertil Steril. 2007;88:1583–8.
Check JH, Bollendorf A, Wilson C, Summers-Chase D, Horwath D, Yuan W. A retrospective comparison of pregnancy outcome following conventional oocyte insemination vs intracytoplasmic sperm injection for isolated abnormalities in sperm morphology using strict criteria. J Androl. 2007;28(4):607–12.
Rolland M, Le Moal J, Wagner V, Royere D, De Mouzon J. Decline in semen concentration and morphology in a sample of 26609 men close to general population between 1989 and 2005 in France. Hum Reprod. 2013;28(2):462–70.
World Health Organization. Laboratory manual for the examination of human semen and semen-cervical mucus interaction. Singapore: Press Concern; 1980.
World Health Organization. Laboratory manual for the examination of human semen and semen-cervical mucus interaction. Cambridge: Cambridge University Press; 1987.
World Health Organization. Laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge: Cambridge University Press; 1992.
World Health Organization. Laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge: Cambridge University Press; 1999:128.
World Health Organization (WHO). Laboratory manual for the examination and processing of human semen. Geneva: WHO; 2010. p. 271.
Menkveld R. Clinical significance of the low normal sperm morphology value as proposed in the fifth edition of the WHO laboratory manual for the examination and processing of human semen. Asian J Androl. 2010;12:47–58.
Alukal JP, Lamb DJ. Intracytoplasmic sperm injection (ICSI) – what are the risks? Urol Clin North Am. 2008;35(2):277–88.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocyst. In: Jansen R, Mortimer D, editors. Towards reproductive certainty. Carnforth: Parthenon Press; 1999. p. 378–88.
Li Z, Wang AY, Bowman M, Hammarberg K, Farquhar C, Johnson L, et al. ICSI does not increase the cumulative live birth rate in non-male factor infertility. Hum Reprod. 2018;33(7):1322–30.
Schwarze J-E, Jeria R, Crosby J, Villa S, Ortega C, Pommer R. Is there a reason to perform ICSI in the absence of male factor? Lessons from the Latin American registry of ART. Hum Reprod Open. 2017;2.
Hamilton JA, Cissen M, Brandes M, Smeenk JM, de Bruin JP, Kremer JA, et al. Total motile sperm count: a better indicator for the severity of male factor infertility than the WHO sperm classification system. Hum Reprod. 2015;30(5):1110–21.
Centers for Disease Control and Prevention. Assisted reproductive technology fertility clinic success rates report. Atlanta (GA): US Dept of Health and Human Services; 2017. p. 2019.
Funding
This study was funded by the Ottawa Fertility Centre research fund.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Bonnie Woolnough, Jenna Gale, and Elham Sabri. The first draft of the manuscript was written by Bonnie Woolnough, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Doron Shmorgun is a partner with the Ottawa Fertility Centre. Marie-Claude Leveille is an employee of the Ottawa Fertility Centre, and Jenna Gale is an associate physician at the Ottawa Fertility Centre. Bonnie Woolnough has no conflict of interest to declare. Elham Sabri has no conflict of interest to declare.
Ethics approval
This research study was conducted retrospectively from data obtained for clinical purposes for quality assurance. The Ottawa Health Science Network Research Ethics Board found the study to be exempt from requiring ethics review.
Research data repository: Synapse: DOI: https://doi.org/10.7303/syn21535256
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Woolnough, B., Shmorgun, D., Leveille, MC. et al. Does omitting teratospermia as a selection criterion for ICSI change pregnancy rates?. J Assist Reprod Genet 37, 1895–1901 (2020). https://doi.org/10.1007/s10815-020-01827-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01827-1