Abstract
Purpose
To identify factors predictive of having supernumerary embryos in a fresh IVF cycle and create a prediction model for clinical counseling.
Methods
We utilized a multivariable Poisson regression to identify predictive factors and then entered these into a logistic regression model, calculating a risk index for each significant variable. The final model was tested using a receiver operating characteristic curve.
Results
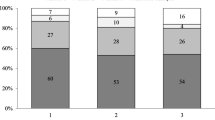
A total of 60,616 fresh transfer cycles were reported to the Society for Assisted Reproductive Technology in 2014. Of these, 47.17% produced supernumerary embryos. A multivariate Poisson regression identified factors predictive of having supernumerary embryos, with age and AMH being the most predictive. Clinical prediction models were developed with acceptable and excellent discrimination. 23.5% of our cohort did not achieve a live birth following their fresh transfer and had excess embryos cryopreserved for future attempts.
Conclusion
Our study suggests that in a minority of fresh IVF cycles in the USA, the fresh transfer is not successful, and there are excess embryos cryopreserved for future use. The likelihood of excess embryos beyond those that would be transferred can be predicted with satisfactory precision prior to initiation of the cycle and with improved precision after fresh embryo transfer. Providing patients with a realistic estimate of their chances of having excess embryos at an initial IVF consult especially those with suspected poor prognosis can be beneficial in determining whether to proceed with multiple embryo banking cycles as opposed to proceeding with a fresh transfer, and whether to opt for an enhanced embryo selection technique such as preimplantation genetic testing for aneuploidy (PGT-A).



Similar content being viewed by others
References
Domar AD, Rooney K, Hacker MR, Sakkas D, Dodge LE. Burden of care is the primary reason why insured women terminate in vitro fertilization treatment. Fertil Steril. 2018;109(6):1121–6.
Ethics Committee of the American Society for Reproductive Medicine. Electronic address, a.a.o. and M. Ethics Committee of the American Society for Reproductive, Fertility treatment when the prognosis is very poor or futile: an Ethics Committee opinion. Fertil Steril. 2019;111(4):659–63.
Maheshwari A, McLernon D, Bhattacharya S. Cumulative live birth rate: time for a consensus? Hum Reprod. 2015;30(12):2703–7.
Gorodeckaja J, et al. High implantation and clinical pregnancy rates with single vitrified-warmed blastocyst transfer and optional aneuploidy testing for all patients. Hum Fertil (Camb). 2019:1–12.
Maxwell SM, Grifo JA. Should every embryo undergo preimplantation genetic testing for aneuploidy? A review of the modern approach to in vitro fertilization. Best Pract Res Clin Obstet Gynaecol. 2018;53:38–47.
Neal SA, Morin SJ, Franasiak JM, Goodman LR, Juneau CR, Forman EJ, et al. Preimplantation genetic testing for aneuploidy is cost-effective, shortens treatment time, and reduces the risk of failed embryo transfer and clinical miscarriage. Fertil Steril. 2018;110(5):896–904.
Lee HL, McCulloh D, Hodes-Wertz B, Adler A, McCaffrey C, Grifo JA. In vitro fertilization with preimplantation genetic screening improves implantation and live birth in women age 40 through 43. J Assist Reprod Genet. 2015;32(3):435–44.
Munne S, et al. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112(6):1071–9 e7.
Scott RT Jr, et al. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100(3):697–703.
Ozgur K, Berkkanoglu M, Bulut H, Yoruk GDA, Candurmaz NN, Coetzee K. Single best euploid versus single best unknown-ploidy blastocyst frozen embryo transfers: a randomized controlled trial. J Assist Reprod Genet. 2019;36(4):629–36.
Drakopoulos P, Blockeel C, Stoop D, Camus M, de Vos M, Tournaye H, et al. Conventional ovarian stimulation and single embryo transfer for IVF/ICSI. How many oocytes do we need to maximize cumulative live birth rates after utilization of all fresh and frozen embryos? Hum Reprod. 2016;31(2):370–6.
Sullivan LM, Massaro JM, D'Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med. 2004;23(10):1631–60.
Hosmer DW, Lemeshow S. Wiley series in probability and statistics Texts and references section. In: Applied logistic regression. 2nd ed. New York: Wiley; 2000. p. xii. 373 pages.
Harrell, F.E., Regression modeling strategies : with applications to linear models, logistic regression, and survival analysis.
Practice Committee of the American Society for Reproductive Medicine. Electronic address, A.a.o. and T. Practice Committee of the Society for Assisted Reproductive. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901–3.
McLernon DJ, et al. Predicting the chances of a live birth after one or more complete cycles of in vitro fertilisation: population based study of linked cycle data from 113 873 women. BMJ. 2016;355:i5735.
van Loendersloot LL, et al. Individualized decision-making in IVF: calculating the chances of pregnancy. Hum Reprod. 2013;28(11):2972–80.
Nelson SM, Fleming R, Gaudoin M, Choi B, Santo-Domingo K, Yao M. Antimullerian hormone levels and antral follicle count as prognostic indicators in a personalized prediction model of live birth. Fertil Steril. 2015;104(2):325–32.
Weissman A, Shoham G, Shoham Z, Fishel S, Leong M, Yaron Y. Preimplantation genetic screening: results of a worldwide web-based survey. Reprod BioMed Online. 2017;35(6):693–700.
Rubio C, Bellver J, Rodrigo L, Castillón G, Guillén A, Vidal C, et al. In vitro fertilization with preimplantation genetic diagnosis for aneuploidies in advanced maternal age: a randomized, controlled study. Fertil Steril. 2017;107(5):1122–9.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100(1):100–7 e1.
Yang YS, et al. Preimplantation genetic screening of blastocysts by multiplex qPCR followed by fresh embryo transfer: validation and verification. Mol Cytogenet. 2015;8:49.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101(3):656–63 e1.
Sunderam S, et al. Assisted reproductive technology surveillance - United States, 2015. MMWR Surveill Summ. 2018;67(3):1–28.
Somigliana E, Busnelli A, Paffoni A, Vigano P, Riccaboni A, Rubio C, et al. Cost-effectiveness of preimplantation genetic testing for aneuploidies. Fertil Steril. 2019;111(6):1169–76.
Dawson AA, Diedrich K, Felberbaum RE. Why do couples refuse or discontinue ART? Arch Gynecol Obstet. 2005;273(1):3–11.
Goldfarb J, Austin C, Lisbona H, Loret de Mola R, Peskin B, Stewart S. Factors influencing patients’ decision not to repeat IVF. J Assist Reprod Genet. 1997;14(7):381–4.
Acknowledgments
SART wishes to thank all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of our members, this research would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
ementary material
ESM 1
(DOCX 19 kb)
Electronic suppl
Electronic suppl
Rights and permissions
About this article
Cite this article
Ibrahim, Y., Stoddard, G. & Johnstone, E. A clinical counseling tool predicting supernumerary embryos after a fresh IVF cycle. J Assist Reprod Genet 37, 1137–1145 (2020). https://doi.org/10.1007/s10815-020-01731-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01731-8