Abstract
With more young breast cancer survivors, a trend toward having children later in life, and improvements in assisted reproductive technology (ART), fertility preserving techniques are of growing importance prior to initiation of gonadotoxic treatments. The American Society for Clinical Oncology (ASCO) updated their Fertility Preservation in Patients with Cancer guidelines in April of 2018. ASCO continues to recognize oocyte and embryo cryopreservation as standard practice for women interested in preserving fertility and sperm cryopreservation as standard practice for men. ASCO has clarified their statement on ovarian suppression during chemotherapy as an option when standard methods are unavailable but should not be used as the sole method of fertility preservation (FP) due to conflicting evidence. ASCO also updated their statement on ovarian tissue cryopreservation, which is still labeled experimental but ASCO acknowledges that it can restore global ovarian function and could be of use in specific patients. The NCCN’s Version 1.2018 Clinical Practice Guidelines® for treatment of breast cancer include fertility counseling as part of their work-up in all types of breast cancer for premenopausal women.The purpose of this review is to explain the indications and evidence for the different methods of FP for young breast cancer patients in accordance with ASCO and NCCN guidelines. The guidance will then be applied to three theoretical clinical cases in order to highlight actual use in clinical practice.
Similar content being viewed by others
References
Breast Cancer Facts & Figures | American Cancer Society. Accessed 19 Jun 2018. Available from: https://www.cancer.org/research/cancer-facts-statistics/breast-cancer-facts-figures.html. 2017–2018.
Female Breast Cancer - Cancer Stat Facts. Accessed 19 Jun 2018. Available from: https://seer.cancer.gov/statfacts/html/breast.html. 2018:Surveillance, Epidemiology, and End Results Program.
NCCN Clinical Practice Guidelines in Oncology. Accessed 16 Jun 2018. Available from: https://www.nccn.org/professionals/physician_gls/default.aspx#detection. Vol 2018. NCCN Version 1.2018 ed: National Comprehensive Cancer Network; 2018.
Fertility Preservation in Patients with Cancer. Accessed 24 Jun 2018. Available from: https://www.asco.org/practice-guidelines/quality-guidelines/guidelines/patient-and-survivor-care#/9661. American Society of Clinical Oncology; 2018.
Goldfarb SB, Kamer SA, Oppong BA, et al. Fertility preservation for the young breast cancer patient. Ann Surg Oncol. 2016;23:1530–6.
Goossens J, Delbaere I, Van Lancker A, Beeckman D, Verhaeghe S, Van Hecke A. Cancer patients' and professional caregivers' needs, preferences and factors associated with receiving and providing fertility-related information: a mixed-methods systematic review. Int J Nurs Stud. 2014;51:300–19.
Peate M, Meiser B, Cheah BC, et al. Making hard choices easier: a prospective, multicentre study to assess the efficacy of a fertility-related decision aid in young women with early-stage breast cancer. Br J Cancer. 2012;106:1053–61.
Letourneau JM, Smith JF, Ebbel EE, et al. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer. 2012;118:4579–88.
Gorman JR, Su HI, Roberts SC, Dominick SA, Malcarne VL. Experiencing reproductive concerns as a female cancer survivor is associated with depression. Cancer. 2015;121:935–42.
Letourneau JM, Ebbel EE, Katz PP, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012;118:1710–7.
Ussher JM, Parton C, Perz J. Need for information, honesty and respect: patient perspectives on health care professionals communication about cancer and fertility. Reprod Health. 2018;15:2.
Kim J, Mersereau JE, Su HI, Whitcomb BW, Malcarne VL, Gorman JR. Young female cancer survivors' use of fertility care after completing cancer treatment. Support Care Cancer. 2016;24:3191–9.
Peate M, Smith SK, Pye V, et al. Assessing the usefulness and acceptability of a low health literacy online decision aid about reproductive choices for younger women with breast cancer: the aLLIAnCE pilot study protocol. Pilot Feasibility Stud. 2017;3:31.
Banerjee R, Tsiapali E. Occurrence and recall rates of fertility discussions with young breast cancer patients. Support Care Cancer. 2016;24:163–71.
Hill KA, Nadler T, Mandel R, et al. Experience of young women diagnosed with breast cancer who undergo fertility preservation consultation. Clin Breast Cancer. 2012;12:127–32.
Gorman JR, Usita PM, Madlensky L, Pierce JP. Young breast cancer survivors: their perspectives on treatment decisions and fertility concerns. Cancer Nurs. 2011;34:32–40.
Jones G, Hughes J, Mahmoodi N, Smith E, Skull J, Ledger W. What factors hinder the decision-making process for women with cancer and contemplating fertility preservation treatment? Hum Reprod Update. 2017;23:433–57.
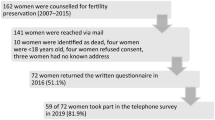
Lambertini M, Anserini P, Fontana V, et al. The PREgnancy and FERtility (PREFER) study: an Italian multicenter prospective cohort study on fertility preservation and pregnancy issues in young breast cancer patients. BMC Cancer. 2017;17:346.
Walter JR, Xu S, Woodruff TK. A call for fertility preservation coverage for breast cancer patients: the cost of consistency. J Natl Cancer Inst 2017;109.
Bann CM, Treiman K, Squiers L, et al. Cancer survivors' use of fertility preservation. J Women's Health (Larchmt). 2015;24:1030–7.
Gonçalves V, Sehovic I, Quinn G. Childbearing attitudes and decisions of young breast cancer survivors: a systematic review. Hum Reprod Update. 2014;20:279–92.
Stensheim H, Cvancarova M, Moller B, Fossa SD. Pregnancy after adolescent and adult cancer: a population-based matched cohort study. Int J Cancer. 2011;129:1225–36.
Gerstl B, Sullivan E, Ives A, Saunders C, Wand H, Anazodo A. Pregnancy outcomes after a breast cancer diagnosis: a systematic review and meta-analysis. Clin Breast Cancer. 2018;18:e79–88.
Murthy RK, Theriault RL, Barnett CM, et al. Outcomes of children exposed in utero to chemotherapy for breast cancer. Breast Cancer Res. 2014;16:500.
Loibl S, Han SN, von Minckwitz G, et al. Treatment of breast cancer during pregnancy: an observational study. Lancet Oncol. 2012;13:887–96.
Hahn KM, Johnson PH, Gordon N, et al. Treatment of pregnant breast cancer patients and outcomes of children exposed to chemotherapy in utero. Cancer. 2006;107:1219–26.
Hartman EK, Eslick GD. The prognosis of women diagnosed with breast cancer before, during and after pregnancy: a meta-analysis. Breast Cancer Res Treat. 2016;160:347–60.
Anderson RA, MRC Centre for Reproductive Health QsMRI, University of Edinburgh, 47 little France crescent, Edinburgh, UK, Brewster DH, et al The impact of cancer on subsequent chance of pregnancy: a population-based analysis. Human Reproduction 2018;33:1281–1290.
Azim HA Jr, Kroman N, Paesmans M, et al. Prognostic impact of pregnancy after breast cancer according to estrogen receptor status: a multicenter retrospective study. J Clin Oncol. 2013;31:73–9.
Llort G, Chirivella I, Morales R, et al. SEOM clinical guidelines in hereditary breast and ovarian cancer. Clin Transl Oncol. 2015;17:956–61.
Wooster R, Weber BL. Breast and ovarian cancer. N Engl J Med. 2003;348:2339–47.
Kuchenbaecker KB, Hopper JL, Barnes DR, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. Jama. 2017;317:2402–16.
Lambertini M, Goldrat O, Toss A, et al. Fertility and pregnancy issues in BRCA-mutated breast cancer patients. Cancer Treat Rev. 2017;59:61–70.
Shapira M, Raanani H, Feldman B, et al. BRCA mutation carriers show normal ovarian response in in vitro fertilization cycles. Fertil Steril. 2015;104:1162–7.
Key Statistics for Breast Cancer in Men. Accessed 13 Jul 2018. Available. from: https://www.cancer.org/cancer/breast-cancer-in-men/about/key-statistics.html. Vol 2018: Am Cancer Soc; 2018.
Ferzoco RM, Ruddy KJ. The epidemiology of male breast cancer. Curr Oncol Rep. 2016;18:1.
Cardoso F, Bartlett JMS, Slaets L, et al. Characterization of male breast cancer: results of the EORTC 10085/TBCRC/BIG/NABCG international male breast cancer program. Ann Oncol. 2018;29:405–17.
Eiser C, Arden-Close E, Morris K, Pacey AA. The legacy of sperm banking: how fertility monitoring and disposal of sperm are linked with views of cancer treatment. Hum Reprod. 2011;26:2791–8.
Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2016;24:2917–31. https://doi.org/10.1200/JCO.2006.06.5888.
Abusief ME, Missmer SA, Ginsburg ES, Weeks JC, Partridge AH. The effects of paclitaxel, dose density, and trastuzumab on treatment-related amenorrhea in premenopausal women with breast cancer. Cancer. 2010;116:791–8.
Ruddy KJ, Guo H, Barry W, et al. Chemotherapy-related amenorrhea after adjuvant paclitaxel-trastuzumab (APT trial). Breast Cancer Res Treat. 2015;151:589–96.
Shandley LM, Spencer JB, Fothergill A, et al. Impact of tamoxifen therapy on fertility in breast cancer survivors. Fertil Steril. 2017;107:243–252.e245.
Blumenfeld Z. Chemotherapy and fertility. Best Pract Res Clin Obstet Gynaecol. 2012;26:379–90.
Sonigo C, Beau I, Grynberg M, Binart N. AMH prevents primordial ovarian follicle loss and fertility alteration in cyclophosphamide-treated mice. FASEB J. 2019;33:1278–87.
Zhou L, Xie Y, Li S, et al. Rapamycin prevents cyclophosphamide-induced over-activation of primordial follicle pool through PI3K/Akt/mTOR signaling pathway in vivo. J Ovarian Res. 2017;10:56.
Goldman KNCD, Arju R, Duncan FE, Keefe DL, Grifo JA, Schneider RJ. mTORC1/2 inhibition preserves ovarian function and fertility during genotoxic chemotherapy. Proc Natl Acad Sci U S A. 2017.
Bines J, Oleske DM, Cobleigh MA. Ovarian function in premenopausal women treated with adjuvant chemotherapy for breast cancer. J Clin Oncol. 1996;14:1718–29.
Zha QB, Tang JH, Li XJ, et al. Prognostic value of chemotherapy-induced amenorrhea in breast cancer: a meta-analysis. Asian Pac J Cancer Prev. 2015;16:5939–44.
Zhou Q, Yin W, Du Y, Shen Z, Lu J. Prognostic impact of chemotherapy-induced amenorrhea on premenopausal breast cancer: a meta-analysis of the literature. Menopause. 2015;22:1091–7.
Zavos A, Valachis A. Risk of chemotherapy-induced amenorrhea in patients with breast cancer: a systematic review and meta-analysis. Acta Oncol. 2016;55:664–70.
Barnabei A, Strigari L, Marchetti P, et al. Predicting ovarian activity in women affected by early breast cancer: a meta-analysis-based nomogram. Oncologist. 2015;20:1111–8.
Anderson RA, Rosendahl M, Kelsey TW, Cameron DA. Pretreatment anti-Müllerian hormone predicts for loss of ovarian function after chemotherapy for early breast cancer. Eur J Cancer. 2013;49:3404–11.
Benedict C, Thom B, Teplinsky E, Carleton J, Kelvin JF. Family-building after breast cancer: considering the effect on adherence to adjuvant endocrine therapy. Clin Breast Cancer. 2017;17:165–70.
Rosenberg SM, Gelber S, Gelber RD, et al. Oncology physicians' perspectives on practices and barriers to fertility preservation and the feasibility of a prospective study of pregnancy after breast cancer. J Adolesc Young Adult Oncol. 2017;6:429–34.
Pascual J, Turner NC. Targeting the PI3-kinase pathway in triple negative breast cancer. Ann Oncol. 2019;30:1051–60.
Marcu LG, Santos A, Bezak E. Risk of second primary cancer after breast cancer treatment. Eur J Cancer Care (Engl). 2014;23:51–64.
Huang JY, Chian RC, Gilbert L, et al. Retrieval of immature oocytes from unstimulated ovaries followed by in vitro maturation and vitrification: a novel strategy of fertility preservation for breast cancer patients. Am J Surg. 2010;200:177–83.
Grynberg M, Poulain M, le Parco S, Sifer C, Fanchin R, Frydman N. Similar in vitro maturation rates of oocytes retrieved during the follicular or luteal phase offer flexible options for urgent fertility preservation in breast cancer patients. Hum Reprod. 2016;31:623–9.
Danis RB, Pereira N, Elias RT. Random start ovarian stimulation for oocyte or embryo cryopreservation in women desiring fertility preservation prior to gonadotoxic cancer therapy. Curr Pharm Biotechnol. 2017;18:609–13.
Nangia AK, Krieg SA, Kim SS. Clinical guidelines for sperm cryopreservation in cancer patients. Fertil Steril. 2013;100:1203–9.
van Casteren NJ, van Santbrink EJ, van Inzen W, Romijn JC, Dohle GR. Use rate and assisted reproduction technologies outcome of cryopreserved semen from 629 cancer patients. Fertil Steril. 2008;90:2245–50.
Olatunbosun OA, Zhu L. The role of sperm banking in fertility preservation. Clin Exp Obstet Gynecol. 2012;39:283–7.
2015 Assisted Reproductive Technology National Summary Report Figures | 2013 ART Report | Division of Reproductive Health | CDC. Accessed 24 Jun 2018. Available. from: https://www.cdc.gov/art/reports/2015/national-summary-figures.html.: Centers for Disease Control and Prevention; 2017
Roque M, Valle M, Guimaraes F, Sampaio M, Geber S. Freeze-all cycle for all normal responders? J Assist Reprod Genet. 2017;34:179–85.
Cold S, During M, Ewertz M, Knoop A, Moller S. Does timing of adjuvant chemotherapy influence the prognosis after early breast cancer? Results of the Danish breast cancer cooperative group (DBCG). Br J Cancer. 2005;93:627–32.
Jara Sanchez C, Ruiz A, Martin M, et al. Influence of timing of initiation of adjuvant chemotherapy over survival in breast cancer: a negative outcome study by the Spanish breast cancer research group (GEICAM). Breast Cancer Res Treat. 2007;101:215–23.
Lohrisch C, Paltiel C, Gelmon K, et al. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006;24:4888–94.
Baynosa J, Westphal LM, Madrigrano A, Wapnir I. Timing of breast cancer treatments with oocyte retrieval and embryo cryopreservation. J Am Coll Surg. 2009;209:603–7.
Turan V, Bedoschi G, Moy F, Oktay K. Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril. 2013;100:1681–1685.e1681.
Wald K, Cakmak H, Mok-Lin E, Cedars M, Rosen M, Letourneau J. Back-to-back random-start ovarian stimulation prior to chemotherapy to maximize oocyte yield. J Assist Reprod Genet. 2019.
Dahhan T, Balkenende E, van Wely M, Linn S, Goddijn M. Tamoxifen or letrozole versus standard methods for women with estrogen-receptor positive breast cancer undergoing oocyte or embryo cryopreservation in assisted reproduction. Cochrane Database Syst Rev. 2013:Cd010240.
Oktay K, Buyuk E, Rodriguez-Wallberg KA, Sahin G. In vitro maturation improves oocyte or embryo cryopreservation outcome in breast cancer patients undergoing ovarian stimulation for fertility preservation. Reprod BioMed Online. 2010;20:634–8.
Richani D, Gilchrist RB. The epidermal growth factor network: role in oocyte growth, maturation and developmental competence. Hum Reprod Update. 2018;24:1–14.
Guzel Y, Bildik G, Oktem O. Sphingosine-1-phosphate protects human ovarian follicles from apoptosis in vitro. Eur J Obstet Gynecol Reprod Biol. 2018;222:19–24.
Moria A, Das M, Shehata F, Holzer H, Son WY, Tulandi T. Ovarian reserve and oocyte maturity in women with malignancy undergoing in vitro maturation treatment. Fertil Steril. 2011;95:1621–3.
Salama M, Woodruff TK. New advances in ovarian autotransplantation to restore fertility in cancer patients. Cancer Metastasis Rev. 2015;34:807–22.
Gook DA, Edgar DH. Cryopreservation of female reproductive potential. Best Pract Res Clin Obstet Gynaecol. 2019;55:23–36.
Gellert SE, Pors SE, Kristensen SG, Bay-Bjorn AM, Ernst E, Yding AC. Transplantation of frozen-thawed ovarian tissue: an update on worldwide activity published in peer-reviewed papers and on the Danish cohort. J Assist Reprod Genet. 2018;35:561–70.
Dolmans MM, Marotta ML, Pirard C, Donnez J, Donnez O. Ovarian tissue cryopreservation followed by controlled ovarian stimulation and pick-up of mature oocytes does not impair the number or quality of retrieved oocytes. J Ovarian Res. 2014;7:80.
Hourvitz A, Yerushalmi GM, Maman E, et al. Combination of ovarian tissue harvesting and immature oocyte collection for fertility preservation increases preservation yield. Reprod BioMed Online. 2015;31:497–505.
Oktay K, Turan V. Failure of ovarian suppression with gonadotropin-releasing hormone analogs to preserve fertility: an assessment based on the quality of evidence. JAMA Oncol. 2016;2:74–5.
Lambertini M, Ceppi M, Poggio F, et al. Ovarian suppression using luteinizing hormone-releasing hormone agonists during chemotherapy to preserve ovarian function and fertility of breast cancer patients: a meta-analysis of randomized studies. Ann Oncol. 2015;26:2408–19.
Elgindy E, Sibai H, Abdelghani A, Mostafa M. Protecting ovaries during chemotherapy through gonad suppression: a systematic review and meta-analysis. Obstet Gynecol. 2015;126:187–95.
Dating, Sex, And reproduction. Accessed 13 Jul 2018. Available. from: https://www.cancer.net/navigating-cancer-care/dating-sex-and-reproduction. Navigating Cancer Care. Vol 2018: Proc Am Soc Clin Oncol; 2012.
Cancer and Fertility. Accessed 13 Jul 2018. Available. from: https://www.nccn.org/patients/resources/life_with_cancer/fertility.aspx. Life with Cancer. Vol 2018: National Comprehensive Cancer Network; 2018.
Society for Assisted Reproductive Technology: Find A Clinic. Accessed 21 Jul 2018. Available. from: https://www.sart.org/clinic-pages/find-a-clinic/. Vol 2018: ReprodMed; 2018.
Acknowledgements
We would like to thank Bernie Amaro for his assistance and comments that greatly improved this manuscript. Mr. Amaro is a research assistant for the Department of Obstetrics and Gynecology at the University of Florida College of Medicine in Gainesville, FL, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest. This research did not receive any specific grant sponsorship from funding agencies in the public, commercial, or not-for-profit sectors. The findings of this project were included in a poster presentation at the UF College of Medicine Celebration of Research on February 19, 2019.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hampe, M.E., Rhoton-Vlasak, A.S. Fertility preservation in breast cancer with case-based examples for guidance. J Assist Reprod Genet 37, 717–729 (2020). https://doi.org/10.1007/s10815-019-01665-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01665-w