Abstract
Purpose
To evaluate if sperm DNA fragmentation (SDF) in the sample used for intracytoplasmic sperm injection (ICSI) impacts outcomes after euploid blastocyst transfer.
Methods
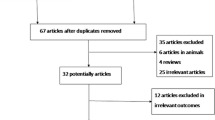
Prospective cohort study of couples undergoing IVF with preimplantation genetic testing for aneuploidy from December 2014–June 2017. Sperm collected on the day of ICSI was analyzed for SDF using the sperm chromatin structure assay (SCSA®). Semen analysis parameters, embryologic outcomes, and clinical outcomes after euploid blastocyst transfer were compared between groups with DNA fragmentation index (DFI) ≤ 15% and DFI > 15% using Mann–Whitney U, t tests, and generalized linear mixed effects models.
Results
Two hundred thirty-four patients were included. One hundred seventy-nine men had DFI ≤ 15% (low DFI group) and 55 men had DFI > 15% group (high DFI group). Total motile sperm and sperm concentration were significantly lower in the group with DFI > 15% vs. DFI ≤ 15%. There was no difference in fertilization (86.3 vs. 84.2%, adjusted OR (95% CI) 0.86 (0.63–1.18)), blastulation (49.5 vs. 48.8%, adjusted OR 1.02 (0.75–1.36)), or euploidy (55.7 vs. 52.1%, adjusted OR 0.96 (0.7–1.31)) between the low and high DFI groups, respectively. Clinical outcomes were similar between low and high DFI groups, including implantation rate (68.8 vs. 79.8%), ongoing pregnancy rate (65.9 vs. 72.6%), and miscarriage rate (4.2 vs. 8.8%), respectively.
Conclusion
Sperm DNA fragmentation on the day of ICSI is not associated with embryologic or clinical outcomes after euploid blastocyst transfer. Increasing levels of SDF are associated with low sperm concentration and total motile sperm count.


Similar content being viewed by others
References
Chandra A, Copen CE, Stephen EH. Infertility and impaired fecundity in the United States, 1982-2010: data from the National Survey of Family Growth. Natl Health Stat Rep. 2013;(67):1–18.
Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod. 1991;6(6):811–6.
Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European Association of Urology guidelines on Male Infertility: the 2012 update. Eur Urol. 2012;62(2):324–32.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. 2009. https://doi.org/10.1056/NEJMoa003005.
Esteves SC. Clinical relevance of routine semen analysis and controversies surrounding the 2010 World Health Organization criteria for semen examination. Int Braz J Urol. 2014;40(4):443–53.
Agarwal A, Allamaneni SS. Sperm DNA damage assessment: a test whose time has come. Fertil Steril. 2005;84(4):850–3.
Sakkas D. denny.sakkas@yale.edu, Division of Reproductive E, Infertility YUSoMNHC, Molecular Biometrics Inc NHC, Juan GA et al. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril. 2010;93(4):1027-36.
Tesarik J, Mendoza C, Greco E. Paternal effects acting during the first cell cycle of human preimplantation development after ICSI. Hum Reprod. 2002;17(1):184–9.
Kumar K, Deka D, Singh A, Mitra DK, Vanitha BR, Dada R. Predictive value of DNA integrity analysis in idiopathic recurrent pregnancy loss following spontaneous conception. J Assist Reprod Genet. 2012;29(9):861–7.
Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril. 2012;98(2):294–301.
Esteves SC, Roque M, Bradley CK, Garrido N. Reproductive outcomes of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with high levels of DNA fragmentation in semen: systematic review and meta-analysis. Fertil Steril. 2017;108(3):456–67.
Bungum M. Sperm DNA integrity assessment: a new tool in diagnosis and treatment of fertility. Obstet Gynecol Int. 2011;2012:531042.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2006;22(1):174–9.
Erenpreiss J, Bungum M, Spano M, Elzanaty S, Orbidans J, Giwercman A. Intra-individual variation in sperm chromatin structure assay parameters in men from infertile couples: clinical implications. Hum Reprod. 2006;21(8):2061–4.
Bronet F, Martínez E, Gaytán M, Liñán A, Cernuda D, Ariza M, et al. Sperm DNA fragmentation index does not correlate with the sperm or embryo aneuploidy rate in recurrent miscarriage or implantation failure patients. Hum Reprod. 2012;27(7):1922–9.
Kaarouch I, Bouamoud N, Louanjli N, Madkour A, Copin H, Benkhalifa M, et al. Impact of sperm genome decay on Day-3 embryo chromosomal abnormalities from advanced-maternal-age patients. Mol Reprod Dev. 2015;82(10):809–19.
González-Marín C, Gosálvez J, Roy R. Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. Int J Mol Sci. 2012;13(11):14026–52.
Al Omrani B, Al Eisa N, Javed M, Al Ghedan M, Al Matrafi H, Al SH. Associations of sperm DNA fragmentation with lifestyle factors and semen parameters of Saudi men and its impact on ICSI outcome. Reprod Biol Endocrinol. 2018;16(1):49.
Belloc S, Benkhalifa M, Cohen-Bacrie M, Dalleac A, Amar E, Zini A. Sperm deoxyribonucleic acid damage in normozoospermic men is related to age and sperm progressive motility. Fertil Steril. 2014;101(6):1588–93.
Oleszczuk K, Giwercman A, Bungum M. Sperm chromatin structure assay in prediction of in vitro fertilization outcome. Andrology. 2016;4(2):290–6.
Lin MH, Kuo-Kuang Lee R, Li SH, Lu CH, Sun FJ, Hwu YM. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90(2):352–9.
Funding
This research was supported by a grant from the Foundation for Embryonic Competence, Basking Ridge, New Jersey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional Review Board (IRB) approval was obtained through Copernicus Group IRB®.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Green, K.A., Patounakis, G., Dougherty, M.P. et al. Sperm DNA fragmentation on the day of fertilization is not associated with embryologic or clinical outcomes after IVF/ICSI. J Assist Reprod Genet 37, 71–76 (2020). https://doi.org/10.1007/s10815-019-01632-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01632-5