Abstract
Purpose
We aimed to evaluate the regulation of miR-99a to the biological functions of granulosa cells in polycystic ovary syndrome (PCOS) via targeting IGF-1R.
Methods
We collected aspirated follicular fluid in both patients with and without PCOS. Granulosa cells (GCs) were isolated through Percoll differential centrifugation to detect both miR-99a and IGF-1R expressions. We further transfected COV434 cells with miR-99a mimics to establish a miRNA-99a (miR-99a) overexpression model. We explored the regulation of miR-99a to the proliferation and apoptosis of human GCs via IGF-1R in COV434. The effect of different insulin concentrations on miR-99a expression was also evaluated.
Results
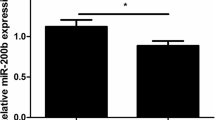
MiR-99a was significantly downregulated while IGF-1R was upregulated in patients with PCOS. MiR-99a can regulate IGF-1R on a post-transcriptional level. After transfection of miR-99a mimics, the proliferation rate was decreased and apoptosis rate was increased significantly in COV434. Exogenous insulin-like growth factor 1 (IGF-1) treatment could reverse the effect of miR-99a. MiR-99a was negatively and dose-dependently regulated by insulin in vitro.
Conclusions
MiR-99a expression was downregulated in patients with PCOS, the degree of which may be closely related to insulin resistance and hyperinsulinemia. MiR-99a could attenuate proliferation and promote apoptosis of human GCs through targeting IGF-1R, which could partly explain the abnormal folliculogenesis in PCOS.







Similar content being viewed by others
References
Dalmay T. MicroRNAs and cancer. J Intern Med. 2008;263(4):366–75. https://doi.org/10.1111/j.1365-2796.2008.01926.x.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–33. https://doi.org/10.1016/j.cell.2009.01.002.
McKenna LB, Schug J, Vourekas A, McKenna JB, Bramswig NC, Friedman JR, et al. MicroRNAs control intestinal epithelial differentiation, architecture, and barrier function. Gastroenterology. 2010;139(5):1654–64, 64 e1. https://doi.org/10.1053/j.gastro.2010.07.040.
Fan C, Lin Y, Mao Y, Huang Z, Liu AY, Ma H, et al. MicroRNA-543 suppresses colorectal cancer growth and metastasis by targeting KRAS, MTA1 and HMGA2. Oncotarget. 2016;7(16):21825–39. https://doi.org/10.18632/oncotarget.7989.
Ge X, Liu X, Lin F, Li P, Liu K, Geng R, et al. MicroRNA-421 regulated by HIF-1alpha promotes metastasis, inhibits apoptosis, and induces cisplatin resistance by targeting E-cadherin and caspase-3 in gastric cancer. Oncotarget. 2016;7(17):24466–82. https://doi.org/10.18632/oncotarget.8228.
Shukla GC, Singh J, Barik S. MicroRNAs: processing, maturation, target recognition and regulatory functions. Mol Cell Pharmacol. 2011;3(3):83–92.
Mei LL, Qiu YT, Huang MB, Wang WJ, Bai J, Shi ZZ. MiR-99a suppresses proliferation, migration and invasion of esophageal squamous cell carcinoma cells through inhibiting the IGF1R signaling pathway. Cancer Biomark. 2017;20:527–37. https://doi.org/10.3233/CBM-170345.
Wang X, Li Y, Qi W, Zhang N, Sun M, Huo Q, et al. MicroRNA-99a inhibits tumor aggressive phenotypes through regulating HOXA1 in breast cancer cells. Oncotarget. 2015;6(32):32737–47. https://doi.org/10.18632/oncotarget.5355.
Xing B, Ren C. Tumor-suppressive miR-99a inhibits cell proliferation via targeting of TNFAIP8 in osteosarcoma cells. Am J Transl Res. 2016;8(2):1082–90.
Maugeri M, Barbagallo D, Barbagallo C, Banelli B, Di Mauro S, Purrello F, et al. Altered expression of miRNAs and methylation of their promoters are correlated in neuroblastoma. Oncotarget. 2016;7(50):83330–41. https://doi.org/10.18632/oncotarget.13090.
Weroha SJ, Haluska P. The insulin-like growth factor system in cancer. Endocrinol Metab Clin N Am. 2012;41(2):335–50, vi. https://doi.org/10.1016/j.ecl.2012.04.014.
Goodarzi MO, Dumesic DA, Chazenbalk G, Azziz R. Polycystic ovary syndrome: etiology, pathogenesis and diagnosis. Nat Rev Endocrinol. 2011;7(4):219–31. https://doi.org/10.1038/nrendo.2010.217.
Moran L, Teede H. Metabolic features of the reproductive phenotypes of polycystic ovary syndrome. Hum Reprod Update. 2009;15(4):477–88. https://doi.org/10.1093/humupd/dmp008.
Eek D, Paty J, Black P, Celeste Elash CA, Reaney M. A comprehensive disease model of polycystic ovary syndrome (Pcos). Value Health. 2015;18(7):A722. https://doi.org/10.1016/j.jval.2015.09.2739.
Diamanti-Kandarakis E, Piperi C, Spina J, Argyrakopoulou G, Papanastasiou L, Bergiele A, et al. Polycystic ovary syndrome: the influence of environmental and genetic factors. Hormones. 2006;5(1):17–34.
Artimani T, Saidijam M, Aflatoonian R, Amiri I, Ashrafi M, Shabab N, et al. Estrogen and progesterone receptor subtype expression in granulosa cells from women with polycystic ovary syndrome. Gynecol Endocrinol. 2015;31(5):379–83. https://doi.org/10.3109/09513590.2014.1001733.
Stubbs SA, Stark J, Dilworth SM, Franks S, Hardy K. Abnormal preantral folliculogenesis in polycystic ovaries is associated with increased granulosa cell division. J Clin Endocrinol Metab. 2007;92(11):4418–26. https://doi.org/10.1210/jc.2007-0729.
Das M, Djahanbakhch O, Hacihanefioglu B, Saridogan E, Ikram M, Ghali L, et al. Granulosa cell survival and proliferation are altered in polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93(3):881–7. https://doi.org/10.1210/jc.2007-1650.
Chang RJ, Cook-Andersen H. Disordered follicle development. Mol Cell Endocrinol. 2013;373(1–2):51–60. https://doi.org/10.1016/j.mce.2012.07.011.
Yu YS, Sui HS, Han ZB, Li W, Luo MJ, Tan JH. Apoptosis in granulosa cells during follicular atresia: relationship with steroids and insulin-like growth factors. Cell Res. 2004;14(4):341–6. https://doi.org/10.1038/sj.cr.7290234.
Cakir E, Topaloglu O, Colak Bozkurt N, Karbek Bayraktar B, Gungunes A, Sayki Arslan M, et al. Insulin-like growth factor 1, liver enzymes, and insulin resistance in patients with PCOS and hirsutism. Turkish J Med Sci. 2014;44(5):781–6.
Hossain MM, Cao M, Wang Q, Kim JY, Schellander K, Tesfaye D, et al. Altered expression of miRNAs in a dihydrotestosterone-induced rat PCOS model. J Ovarian Res. 2013;6(1):36. https://doi.org/10.1186/1757-2215-6-36.
Roth LW, McCallie B, Alvero R, Schoolcraft WB, Minjarez D, Katz-Jaffe MG. Altered microRNA and gene expression in the follicular fluid of women with polycystic ovary syndrome. J Assist Reprod Genet. 2014;31(3):355–62. https://doi.org/10.1007/s10815-013-0161-4.
Liu S, Zhang X, Shi C, Lin J, Chen G, Wu B, et al. Altered microRNAs expression profiling in cumulus cells from patients with polycystic ovary syndrome. J Transl Med. 2015;13:238. https://doi.org/10.1186/s12967-015-0605-y.
Zhang ZW, Guo RW, Lv JL, Wang XM, Ye JS, Lu NH, et al. MicroRNA-99a inhibits insulin-induced proliferation, migration, dedifferentiation, and rapamycin resistance of vascular smooth muscle cells by inhibiting insulin-like growth factor-1 receptor and mammalian target of rapamycin. Biochem Biophys Res Commun. 2017;486(2):414–22. https://doi.org/10.1016/j.bbrc.2017.03.056.
Tao J, Yang X, Han Z, Lu P, Wang J, Liu X, et al. Serum MicroRNA-99a helps detect acute rejection in renal transplantation. Transplant Proc. 2015;47(6):1683–7. https://doi.org/10.1016/j.transproceed.2015.04.094.
Yang SY, Wang YQ, Gao HM, Wang B, He Q. The clinical value of circulating miR-99a in plasma of patients with acute myocardial infarction. Eur Rev Med Pharmacol Sci. 2016;20(24):5193–7.
Jin Y, Tymen SD, Chen D, Fang ZJ, Zhao Y, Dragas D, et al. MicroRNA-99 family targets AKT/mTOR signaling pathway in dermal wound healing. PLoS One. 2013;8(5):e64434. https://doi.org/10.1371/journal.pone.0064434.
Yao G, Yin M, Lian J, Tian H, Liu L, Li X, et al. MicroRNA-224 is involved in transforming growth factor-beta-mediated mouse granulosa cell proliferation and granulosa cell function by targeting Smad4. Mol Endocrinol. 2010;24(3):540–51. https://doi.org/10.1210/me.2009-0432.
Lei L, Jin S, Gonzalez G, Behringer RR, Woodruff TK. The regulatory role of Dicer in folliculogenesis in mice. Mol Cell Endocrinol. 2010;315(1–2):63–73. https://doi.org/10.1016/j.mce.2009.09.021.
Hong X, Luense LJ, McGinnis LK, Nothnick WB, Christenson LK. Dicer1 is essential for female fertility and normal development of the female reproductive system. Endocrinology. 2008;149(12):6207–12. https://doi.org/10.1210/en.2008-0294.
Ding CF, Chen WQ, Zhu YT, Bo YL, Hu HM, Zheng RH. Circulating microRNAs in patients with polycystic ovary syndrome. Hum Fertil. 2015;18(1):22–9. https://doi.org/10.3109/14647273.2014.956811.
Kota J, Chivukula RR, O'Donnell KA, Wentzel EA, Montgomery CL, Hwang HW, et al. Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell. 2009;137(6):1005–17. https://doi.org/10.1016/j.cell.2009.04.021.
Teixeira Filho FL, Baracat EC, Lee TH, Suh CS, Matsui M, Chang RJ, et al. Aberrant expression of growth differentiation factor-9 in oocytes of women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87(3):1337–44. https://doi.org/10.1210/jcem.87.3.8316.
Li D, Liu X, Lin L, Hou J, Li N, Wang C, et al. MicroRNA-99a inhibits hepatocellular carcinoma growth and correlates with prognosis of patients with hepatocellular carcinoma. J Biol Chem. 2011;286(42):36677–85. https://doi.org/10.1074/jbc.M111.270561.
Brahmkhatri VP, Prasanna C, Atreya HS. Insulin-like growth factor system in cancer: novel targeted therapies. Biomed Res Int. 2015;2015:538019–24. https://doi.org/10.1155/2015/538019.
Stubbs SA, Webber LJ, Stark J, Rice S, Margara R, Lavery S, et al. Role of insulin-like growth factors in initiation of follicle growth in normal and polycystic human ovaries. J Clin Endocrinol Metab. 2013;98(8):3298–305. https://doi.org/10.1210/jc.2013-1378.
Louhio H, Hovatta O, Sjoberg J, Tuuri T. The effects of insulin, and insulin-like growth factors I and II on human ovarian follicles in long-term culture. Mol Hum Reprod. 2000;6(8):694–8.
Premoli AC, Santana LF, Ferriani RA, Moura MD, De Sa MF, Reis RM. Growth hormone secretion and insulin-like growth factor-1 are related to hyperandrogenism in nonobese patients with polycystic ovary syndrome. Fertil Steril. 2005;83(6):1852–5. https://doi.org/10.1016/j.fertnstert.2004.10.057.
Velazquez MA, Hermann D, Kues WA, Niemann H. Increased apoptosis in bovine blastocysts exposed to high levels of IGF1 is not associated with downregulation of the IGF1 receptor. Reproduction. 2011;141(1):91–103. https://doi.org/10.1530/REP-10-0336.
Luo L, Wang Q, Chen M, Yuan G, Wang Z, Zhou C. IGF-1 and IGFBP-1 in peripheral blood and decidua of early miscarriages with euploid embryos: comparison between women with and without PCOS. Gynecol Endocrinol. 2016;32(7):538–42. https://doi.org/10.3109/09513590.2016.1138459.
Homburg R, Pariente C, Lunenfeld B, Jacobs HS. The role of insulin-like growth factor-1 (IGF-1) and IGF binding protein-1 (IGFBP-1) in the pathogenesis of polycystic ovary syndrome. Hum Reprod. 1992;7(10):1379–83.
Thierry van Dessel HJ, Lee PD, Faessen G, Fauser BC, Giudice LC. Elevated serum levels of free insulin-like growth factor I in polycystic ovary syndrome. J Clin Endocrinol Metab. 1999;84(9):3030–5. https://doi.org/10.1210/jcem.84.9.5941.
Li W, Wang J, Chen QD, Qian X, Li Q, Yin Y, et al. Insulin promotes glucose consumption via regulation of miR-99a/mTOR/PKM2 pathway. PLoS One. 2013;8(6):e64924. https://doi.org/10.1371/journal.pone.0064924.
Cai G, Ma X, Chen B, Huang Y, Liu S, Yang H, et al. MicroRNA-145 negatively regulates cell proliferation through targeting IRS1 in isolated ovarian granulosa cells from patients with polycystic ovary syndrome. Reprod Sci. 2016;24(6):902–10. https://doi.org/10.1177/1933719116673197.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No. 81401268).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Geng, Y., Sui, C., Xun, Y. et al. MiRNA-99a can regulate proliferation and apoptosis of human granulosa cells via targeting IGF-1R in polycystic ovary syndrome. J Assist Reprod Genet 36, 211–221 (2019). https://doi.org/10.1007/s10815-018-1335-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1335-x