Abstract
Purpose
The purpose of this study was to compare baseline characteristics and ovarian stimulation outcomes between patients presenting for medically indicated vs. elective fertility preservation consultation and to determine the impact of the 2013 ASRM guidelines on oocyte cryopreservation on the patient population presenting for fertility preservation consultation.
Methods
Retrospective cohort study conducted at an academic center. Study population included 332 patients presenting for medically indicated fertility preservation consultation and 210 patients presenting for elective consultation.
Results
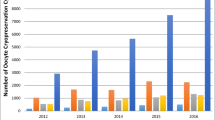
Patients presenting for elective fertility preservation consultation were more likely to be of advanced age, non-Caucasian, highly educated, single, nulligravid, and meet criteria for diminished ovarian reserve (DOR). Additionally, patients presenting electively were more likely to have fertility insurance benefits. A higher percentage of patients with insurance benefits for oocyte cryopreservation proceeded to stimulation. There were no differences in stimulation parameters or number of retrieved oocytes between the groups when adjusted for age. Following release of the ASRM guidelines on oocyte cryopreservation, there was no difference in the percentage of patients in the medical group who proceeded with stimulation; however, a higher percentage of patients presenting electively underwent ovarian stimulation.
Conclusion
Although the populations presenting for medical compared with elective fertility preservation differ at baseline, ovarian stimulation parameters and outcomes are similar when adjusted for age. Insurance benefits for fertility preservation are not comprehensive and impact the decision to proceed with stimulation in all patients. The publication of the ASRM guidelines on oocyte cryopreservation increased utilization of this technology among patients presenting electively; however, they remained at an advanced age and with decreased ovarian reserve parameters.
Similar content being viewed by others
References
Cil AP, Turkgeldi L, Seli E. Oocyte cryopreservation as a preventive measure for age-related fertility loss. Semin Reprod Med. 2015;33(6):429–35. doi:10.1055/s-0035-1567819.
Rudick B, Opper N, Paulson R, Bendikson K, Chung K. The status of oocyte cryopreservation in the United States. Fertil Steril. 2010;94(7):2642–6. doi:10.1016/j.fertnstert.2010.04.079.
Zoll M, Mertes H, Gupta J. Corporate giants provide fertility benefits: have they got it wrong? Eur J Obstet Gynecol Reprod Biol. 2015;195:A1–2. doi:10.1016/j.ejogrb.2015.10.018.
Mertes H, Pennings G. Social egg freezing: for better, not for worse. Reprod BioMed Online. 2011;23(7):824–9. doi:10.1016/j.rbmo.2011.09.010.
Goldman KN, Grifo JA. Elective oocyte cryopreservation for deferred childbearing. Curr Opin Endocrinol Diabetes Obes. 2016;23(6):458–64. doi:10.1097/MED.0000000000000291.
Daniluk JC, Koert E. Childless women’s beliefs and knowledge about oocyte freezing for social and medical reasons. Hum Reprod. 2016;31(10):2313–20. doi:10.1093/humrep/dew189.
Practice Committees of American Society for Reproductive M, Society for Assisted Reproductive T. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99(1):37–43. doi:10.1016/j.fertnstert.2012.09.028.
Ethics ETFo, Law, Dondorp W, de Wert G, Pennings G, Shenfield F, et al. Oocyte cryopreservation for age-related fertility loss. Hum Reprod. 2012;27(5):1231–7. doi:10.1093/humrep/des029.
Johnson LN, Dillon KE, Sammel MD, Efymow BL, Mainigi MA, Dokras A, et al. Response to ovarian stimulation in patients facing gonadotoxic therapy. Reprod BioMed Online. 2013;26(4):337–44. doi:10.1016/j.rbmo.2013.01.003.
Almog B, Azem F, Gordon D, Pauzner D, Amit A, Barkan G, et al. Effects of cancer on ovarian response in controlled ovarian stimulation for fertility preservation. Fertil Steril. 2012;98(4):957–60. doi:10.1016/j.fertnstert.2012.06.007.
Cardozo ER, Thomson AP, Karmon AE, Dickinson KA, Wright DL, Sabatini ME. Ovarian stimulation and in-vitro fertilization outcomes of cancer patients undergoing fertility preservation compared to age matched controls: a 17-year experience. J Assist Reprod Genet. 2015;32(4):587–96. doi:10.1007/s10815-015-0428-z.
Domingo J, Guillen V, Ayllon Y, Martinez M, Munoz E, Pellicer A, et al. Ovarian response to controlled ovarian hyperstimulation in cancer patients is diminished even before oncological treatment. Fertil Steril. 2012;97(4):930–4. doi:10.1016/j.fertnstert.2012.01.093.
Druckenmiller S, Goldman KN, Labella PA, Fino ME, Bazzocchi A, Noyes N. Successful oocyte cryopreservation in reproductive-aged cancer survivors. Obstet Gynecol. 2016;127(3):474–80. doi:10.1097/AOG.0000000000001248.
Friedler S, Koc O, Gidoni Y, Raziel A, Ron-El R. Ovarian response to stimulation for fertility preservation in women with malignant disease: a systematic review and meta-analysis. Fertil Steril. 2012;97(1):125–33. doi:10.1016/j.fertnstert.2011.10.014.
Knopman JM, Noyes N, Talebian S, Krey LC, Grifo JA, Licciardi F. Women with cancer undergoing ART for fertility preservation: a cohort study of their response to exogenous gonadotropins. Fertil Steril. 2009;91(4 Suppl):1476–8. doi:10.1016/j.fertnstert.2008.07.1727.
Quintero RB, Helmer A, Huang JQ, Westphal LM. Ovarian stimulation for fertility preservation in patients with cancer. Fertil Steril. 2010;93(3):865–8. doi:10.1016/j.fertnstert.2008.10.007.
Baldwin K, Culley L, Hudson N, Mitchell H, Lavery S. Oocyte cryopreservation for social reasons: demographic profile and disposal intentions of UK users. Reprod BioMed Online. 2015;31(2):239–45. doi:10.1016/j.rbmo.2015.04.010.
Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100(5):1343–9. doi:10.1016/j.fertnstert.2013.07.201.
Tsafrir A, Haimov-Kochman R, Margalioth EJ, Eldar-Geva T, Gal M, Bdolah Y, et al. Ovarian stimulation for oocyte cryopreservation for prevention of age-related fertility loss: one in five is a low responder. Gynecol Endocrinol. 2015;31(10):779–82. doi:10.3109/09513590.2015.1062859.
Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016;105(2):459–466 e2. doi:10.1016/j.fertnstert.2015.10.026.
Cobo A, Garcia-Velasco JA, Coello A, Domingo J, Pellicer A, Remohi J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016;105(3):755–764 e8. doi:10.1016/j.fertnstert.2015.11.027.
Garcia-Velasco JA, Domingo J, Cobo A, Martinez M, Carmona L, Pellicer A. Five years’ experience using oocyte vitrification to preserve fertility for medical and nonmedical indications. Fertil Steril. 2013;99(7):1994–9. doi:10.1016/j.fertnstert.2013.02.004.
Chan JL, Johnson LN, Efymow BL, Sammel MD, Gracia CR. Outcomes of ovarian stimulation after treatment with chemotherapy. J Assist Reprod Genet. 2015;32(10):1537–45. doi:10.1007/s10815-015-0575-2.
O'Neill KE, Senapati S, Maina I, Gracia C, Dokras A. GnRH agonist with low-dose hCG (dual trigger) is associated with higher risk of severe ovarian hyperstimulation syndrome compared to GnRH agonist alone. J Assist Reprod Genet. 2016;33(9):1175–84. doi:10.1007/s10815-016-0755-8.
Practice Committee of the American Society for Reproductive Medicine. Electronic address Aao, Practice Committee of the American Society for Reproductive M. Prevention and treatment of moderate and severe ovarian hyperstimulation syndrome: a guideline. Fertil Steril. 2016;106(7):1634–47. doi:10.1016/j.fertnstert.2016.08.048.
Baldwin K, Culley L, Hudson N, Mitchell H. Reproductive technology and the life course: current debates and research in social egg freezing. Hum Fertil (Camb). 2014;17(3):170–9. doi:10.3109/14647273.2014.939723.
Kim J, Deal AM, Balthazar U, Kondapalli LA, Gracia C, Mersereau JE. Fertility preservation consultation for women with cancer: are we helping patients make high-quality decisions? Reprod BioMed Online. 2013;27(1):96–103. doi:10.1016/j.rbmo.2013.03.004.
Hill KA, Nadler T, Mandel R, Burlein-Hall S, Librach C, Glass K, et al. Experience of young women diagnosed with breast cancer who undergo fertility preservation consultation. Clin Breast Cancer. 2012;12(2):127–32. doi:10.1016/j.clbc.2012.01.002.
Yee S, Abrol K, McDonald M, Tonelli M, Liu KE. Addressing oncofertility needs: views of female cancer patients in fertility preservation. J Psychosoc Oncol. 2012;30(3):331–46. doi:10.1080/07347332.2012.664257.
Tan SQ, Tan AW, Lau MS, Tan HH, Nadarajah S. Social oocyte freezing: a survey among Singaporean female medical students. J Obstet Gynaecol Res. 2014;40(5):1345–52. doi:10.1111/jog.12347.
Mertes H. Does company-sponsored egg freezing promote or confine women’s reproductive autonomy? J Assist Reprod Genet. 2015;32(8):1205–9. doi:10.1007/s10815-015-0500-8.
Linkeviciute A, Peccatori FA, Sanchini V, Boniolo G. Oocyte cryopreservation beyond cancer: tools for ethical reflection. J Assist Reprod Genet. 2015;32(8):1211–20. doi:10.1007/s10815-015-0524-0.
Bavan B, Porzig E, Baker VL. An assessment of female university students’ attitudes toward screening technologies for ovarian reserve. Fertil Steril. 2011;96(5):1195–9. doi:10.1016/j.fertnstert.2011.08.018.
Birch Petersen K, Hvidman HW, Sylvest R, Pinborg A, Larsen EC, Macklon KT, et al. Family intentions and personal considerations on postponing childbearing in childless cohabiting and single women aged 35-43 seeking fertility assessment and counselling. Hum Reprod. 2015;30(11):2563–74. doi:10.1093/humrep/dev237.
Yu L, Peterson B, Inhorn MC, Boehm JK, Patrizio P. Knowledge, attitudes, and intentions toward fertility awareness and oocyte cryopreservation among obstetrics and gynecology resident physicians. Hum Reprod. 2016;31(2):403–11. doi:10.1093/humrep/dev308.
Stoop D, Maes E, Polyzos NP, Verheyen G, Tournaye H, Nekkebroeck J. Does oocyte banking for anticipated gamete exhaustion influence future relational and reproductive choices? A follow-up of bankers and non-bankers. Hum Reprod. 2015;30(2):338–44. doi:10.1093/humrep/deu317.
Friedman D. Perk up: Facebook and apple now pay for women to freeze eggs. http://www.nbcnews.com/news/us-news/perk-facebook-apple-now-pay-women-freeze-eggs-n225011. 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Institutional Review Board at the University of Pennsylvania (IRB #819938). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Funding sources
NIH T32 HD040135 (SBS), 5K12HD065257-07 (SBS), and 5K12HD001265-14 (SS)
Electronic supplementary material
Supplemental Table 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Schon, S.B., Shapiro, M., Gracia, C. et al. Medical and elective fertility preservation: impact of removal of the experimental label from oocyte cryopreservation. J Assist Reprod Genet 34, 1207–1215 (2017). https://doi.org/10.1007/s10815-017-0968-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-0968-5