Abstract
Background
Children born from fresh in vitro fertilization (IVF) cycles are at greater risk of being born smaller and earlier, even when limited to singletons; those born from frozen cycles have an increased risk of large-for-gestational age (LGA) birthweight (z-score ≥1.28). This analysis sought to overcome limitations in other studies by using pairs of siblings, and accounting for prior cycle outcomes, maternal characteristics, and embryo state and stage.
Methods
Pairs of singleton births conceived with IVF and born between 2004 and 2013 were identified from the Society for Assisted Reproductive Technology Clinic Outcome Reporting System database, matched for embryo stage (blastocyst versus non-blastocyst) and infant gender, categorized by embryo state (fresh versus frozen) in 1st and 2nd births (four groups).
Results
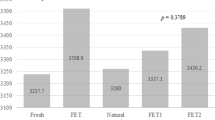
The data included 7795 singleton pairs. Birthweight z-scores were 0.00–0.04 and 0.24–0.26 in 1st and 2nd births in fresh cycles, and 0.25–0.34 and 0.50–0.55 in frozen cycles, respectively. LGA was 9.2–9.8 and 14.2–15.4% in 1st and 2nd births in fresh cycles, and 13.1–15.8 and 20.8–21.0% in 1st and 2nd births in frozen cycles. The risk of LGA was increased in frozen cycles (1st births, adjusted odds ratios (AOR) 1.74, 95% CI 1.45, 2.08; and in 2nd births when the 1st birth was not LGA, AOR 1.70, 95% CI 1.46, 1.98 for fresh/frozen and 1.40, 1.11, 1.78 for frozen/frozen).
Conclusions
Our results with siblings indicate that frozen embryo state is associated with an increased risk for LGA. The implications of these findings for childhood health and risk of obesity are unclear, and warrant further investigation.
Similar content being viewed by others
References
Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012;18:485–503.
Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Söderström-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19:87–104.
Qin J, Liu X, Sheng X, Wang H, Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril. 2016;105:73–85.
Shih W, Rushford DD, Bourne H, Garrett C, McBain JC, Healy DL, et al. Factors affecting low birthweight after assisted reproduction technology: difference between transfer of fresh and cryopreserved embryos suggests an adverse effect of oocyte collection. Hum Reprod. 2008;23:1644–53.
Pelkonen S, Koivunen R, Gissler M, Nuojua-Huttunen S, Suikkari A-M, Hydén-Granskog C, et al. Perinatal outcome of children born after frozen and fresh embryo transfer: the Finnish cohort study 1995–2006. Hum Reprod. 2010;25:914–23.
Henningsen A-KA, Pinborg A, Lidegaard Ø, Vestergaard C, Forman JL, Andersen AN. Perinatal outcome of singleton siblings born after assisted reproductive technology and spontaneous conception: Danish national sibling-cohort study. Fertil Steril. 2011;95:959–63.
Sazonova A, Källen K, Thurin-Kjellberg A, Wennerholm U-B, Bergh C. Obstetric outcome in singletons after in vitro fertilization with cryopreserved/thawed embryos. Hum Reprod. 2012;27:1343–50.
Nakashima A, Araki R, Tani H, Ishihara O, Kuwahara A, Irahara M, et al. Implications of assisted reproductive technologies on term singleton birth weight: an analysis of 25,777 children in the national assisted reproduction registry of Japan. Fertil Steril. 2013;99:450–5.
Wennerholm UB, Henningsen AK, Romundstad LB, Bergh C, Pinborg A, Skjaerven R, et al. Perinatal outcomes of children born after frozen-thawed embryo transfer: a Nordic cohort study from the CoNARTaS group. Hum Reprod. 2013;28:2545–53.
Pinborg A, Henningsen AA, Loft A, Malchau SS, Forman J, Nyboe AA. Large baby syndrome in singletons born after frozen embryo transfer (FET): is it due to maternal factors or the cryotechnique? Hum Reprod. 2014;29:618–27.
Marino JL, Moore VM, Willson KJ, Rumbold A, Whitrow MJ, Giles LC, et al. Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PLoS ONE. 2014;9:e80398. doi:10.1371/journal.pone.0080398.
Korosec S, Frangez HB, Steblovnik L, Verdenik I, Bokal EV. Independent factors influencing large-for-gestation birth weight in singletons born after in vitro fertilization. J Assist Reprod Genet. 2016;33:9–17.
Mäkinen S, Söderström-Anttila V, Vainio J, Suikkari AM, Tuuri T. Does long in vitro culture promote large for gestational age babies? Hum Reprod. 2013;28:828–34.
Buck Louis GM, Schisterman EF, Dukic VM, Schieve LA. Research hurdles complicating the analysis of infertility treatment and child health. Hum Reprod. 2005;20:12–8.
Declercq E, Luke B, Belanoff C, Cabral H, Diop H, Gopal D, et al. Perinatal outcomes associated with assisted reproductive technology: the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Fertil Steril. 2015;103:888–95.
Stern JE, Luke B, Tobias M, Gopal D, Hornstein MD, Diop H. Adverse pregnancy and birth outcomes by infertility diagnoses with and without ART treatment. Fertil Steril. 2015;103:1438–45.
Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjærven R, Gunnell D, et al. Effects of technology or maternal factors on perinatal outcome after assisted fertilization: a population-based cohort study. Lancet. 2008;372:737–43.
Seggers J, Pontesilli M, Ravelli ACJ, Painter RC, Hadders-Algra M, Heineman MJ, et al. Effects of in vitro fertilization and maternal characteristics on perinatal outcomes: a population-based study using siblings. Fertil Steril. 2016;105:590–8.
Galliano D, Garrido N, Serra-Serra V, Pellicer A. Difference in birth weight of consecutive sibling singletons is not found in oocyte donation when comparing fresh versus frozen embryo replacements. Fertil Steril. 2015;104:1411–8.
Opdahl S, Henningsen AA, Tiitinen A, Bergh C, Pinborg A, Romundstad PR, et al. Risk of hypertensive disorders in pregnancies following assisted reproductive technology: a cohort study from the CoNARTaS group. Hum Reprod. 2015;30:1724–31.
Center for Disease Control and Prevention, American Society for Reproductive Medicine, and Society for Assisted Reproductive Technology. Assisted reproductive technology success rates: national summary and fertility clinic reports. Washington, DC: US Dept. of Health and Human Services; 2012. p. 2014.
Bakketeig LS, Hoffman HJ, Harley EE. The tendency to repeat gestational age and birthweight in successive births. Am J Obstet Gynecol. 1979;135:1086–103.
Talge NM, Mudd LM, Sikorskii A, Basso O. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics. 2014;133:844–53.
Land JA. How should we report on perinatal outcome? Hum Reprod. 2006;21:2638–9.
Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes. 2001;25:1175–82.
Institute of Medicine. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press; 2009.
Luke B, Brown MB, Grainger DA, Stern JE, Klein N, Cedars M. The effect of early fetal losses on singleton assisted-conception pregnancy outcomes. Fertil Steril. 2009;91:2578–85.
de Zegher F, Devlieger H, Eeckels R. Fetal growth: boys before girls. Horm Res. 1999;51:258–9.
de Zegher F, Francois I, Boehmer ALM, Saggese G, Muller J, Hiort O, et al. Androgens and fetal growth. Horm Res. 1998;50:243–4.
Pedersen JF. Ultrasound evidence of sexual difference in fetal size in first trimester. Br Med J. 1980;281:1253.
Zeilmaker GH, Alberda AT, van Gent I, Rijkmans CM, Drogendijk AC. Two pregnancies following transfer of intact frozen-thawed embryos. Fertil Steril. 1984;42:293–6.
Maheshwari A, Bhattacharya S. Elective frozen replacement cycles for all: ready for prime time? Hum Reprod. 2013;28:6–9.
Shapiro BS, Daneshman ST, Garner FC, Aguirre M, Hudson C. Clinical rationale for cryopreservation of entire embryo cohorts in lieu of fresh transfer. Fertil Steril. 2014;102:3–9.
Weinerman R, Mainigi M. Why we should transfer frozen instead of fresh embryos: the translational rationale. Fertil Steril. 2014;102:10–8.
Wong KM, Mastenbroek S, Repping S. Cryopreservation of human embryos and its contribution to in vitro fertilization success rates. Fertil Steril. 2014;102:19–26.
Hu X-L, Feng C, Lin X-H, Zhong Z-X, Zhu Y-M, Lv P-P, et al. High maternal serum estradiol environment in the 1st trimester is associated with the increased risk of small-for-gestational-age birth. J Clin Endocrinol Metab. 2014;99:2217–24.
Rallis A, Tremellen K. Controlled ovarian hyper-stimulation during IVF treatment does not increase the risk of preterm delivery compared to the transfer of frozen-thawed embryos in a natural cycle. Aust N Z J Obstet Gynaecol. 2013;53:165–9.
Yeh JS, Steward RG, Dude AM, Shah AA, Goldfarb JM, Muasher SJ. Pregnancy rates in donor oocyte cycles compared to similar autologous in vitro fertilization cycles: an analysis of 26,457 fresh cycles from the Society for Assisted Reproductive Technology. Fertil Steril. 2014;102:399–404.
Wennerholm U-B, Söderström-Anttila V, Bergh C, Aittomäki K, Hazekamp J, Nygren K-G, et al. Children born after cryopreservation of embryos or oocytes: a systematic review of outcome data. Hum Reprod. 2009;24:2158–72.
Roque M, Lattes K, Serra S, Solà I, Geber S, Carreras R, et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril. 2013;99:156–62.
Maheshwari A, Pandey S, Shetty A, Hamilton M, Bhattacharya S. Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen thawed versus fresh embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2012;98:368–77.
Pinborg A, Loft A, Henningsen AKA, Rasmussen S, Nyboe AA. Infant outcome of 957 singletons born after frozen embryo replacement: the Danish National Cohort Study 1995–2006. Fertil Steril. 2010;94:1320–7.
Healy DL, Breheny S, Halliday J, Jaques A, Rushford D, Garrett C, et al. Prevalence and risk factors for obstetric haemorrhage in 6,730 singleton births after assisted reproductive technology in Victoria Australia. Hum Reprod. 2010;25:265–74.
Luke B, Gopal D, Stern JE, Declercq E, Hoang L, Kotelchuck M, et al. Maternal pregnancy and birth complications by fertility status: the Massachusetts outcomes study of assisted reproductive technologies. Fertil Steril. 2015;104:e15.
Belanoff C, Declercq ER, Diop H, Gopal D, Kotelchuck M, Luke B, et al. Severe maternal morbidity and the use of assisted reproductive technology in Massachusetts. Obstet Gynecol. 2016;127:527–34.
Korosec S, Frangez HB, Verdenik I, Kladnik U, Kotar V, Virant-Klun I, Bokal EV. Singleton pregnancy outcomes after in vitro fertilization with fresh or frozen-thawed embryo transfer and incidence of placenta previa. BioMed Res Int. 2014; article ID 431797. Doi.org/10.1155/2014/431797.
Luke B, Stern JE, Kotelchuck M, Declercq E, Anderka M, Diop H. Birth outcomes by infertility treatment: analyses of the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). J Reprod Med. 2016;61:114–27.
Vatten LJ, Skjaerven R. Is pre-eclampsia more than one disease? Br J Obstet Gynaecol. 2004;111:298–302.
Pinborg A, Loft A, Noergaard L, Henningsen AA, Rasmussen S, Nyboe Andersen A. Singletons born after frozen embryo transfer (FET) have an increased risk of being large of gestational age—Danish national controlled cohort study of 15,078 singletons. [abstract] Human Reprod. 2011 (suppl. 1): O-230.
Pinborg A. To transfer fresh or thawed embryos? Seminars Reprod Med. 2012;30:230–5.
Henningsen A-K A, Pinborg A. Birth and perinatal outcomes and complications for babies conceived following ART. Seminars Fetal Neonatal Med. 2014;19:234–8.
Weissmann-Brenner A, Simchen MJ, Zilberberg E, Kalter A, Weisz B, Achiron R, et al. Maternal and neonatal outcomes of large for gestational age pregnancies. Acta Obstet Gynecol Scand. 2012;91:844–9.
Eyzaguirre F, Bancalari R, Romàn R, Silva R, Youlton R, Urquidi C, et al. Prevalence of components of the metabolic syndrome according to birthweight among overweight and obese children and adolescents. J Pediatr Endocrinol Metab. 2012;25:51–6.
Parsons TJ, Power C, Logan S, Summerbell CD. Childhood predictors of adult obesity: a systematic review. Int J Obes. 1999;23(Supplement 8):S1–107.
Eriksson J, Forsén T, Tuomilehto J, Osmond C, Barker D. Size at birth, childhood growth and obesity in adult. Int J Obes. 2001;25:735–40.
Giapros V, Evagelidou E, Challa A, Kiortrios D, Drougia A, Andronikou S. Serum adiponectin and leptin levels and insulin resistance in children born large for gestational age are affected by the degree of overweight. Clin Endocrinol. 2007;66:353–9.
Moore GS, Kneitel AW, Walker CK, Gilbert WM, Xing G. Autism risk in small- and large-for-gestational-age infants. Am J Obstet Gynecol. 2012;206:314.e1–9.
O’Neill KA, Murphy MFG, Bunch KJ, Puumala SE, Carozza SE, Chow EJ, et al. Infant birthweight and risk of childhood cancer: International population-based case control studies of 40,000 cases. Int J Epidemiol. 2015;44:153–68.
Olivennes F, Schneider Z, Remy V, Blanchet V, Kerbrat V, Fanchin R, et al. Perinatal outcome and follow-up of 82 children aged 1–9 years old conceived from cryopreserved embryos. Hum Reprod. 1996;11:1665–8.
Wennerholm UB, Albertsson-Wikland K, Bergh C, Hamberger L, Niklasson A, Nilsson L, et al. Postnatal growth and health in children born after cryopreservation as embryos. Lancet. 1998;351:1085–90.
Nakajo Y, Fukunaga N, Fuchinoue K, Yagi A, Chiba S, Takeda M, et al. Physical and mental development of children after in vitro fertilization and embryo transfer. Reprod Med Biol. 2004;3:63–7.
Green MP, Mouat F, Miles HL, Pleasants AB, Henderson HV, Hofman PL, et al. The phenotype of an IVF child is associated with peri-conception measures of follicular characteristics and embryo quality. Hum Reprod. 2014;29:2583–91.
Romundstad LB, Romundstad PR, Sunde A, von Düring V, Vatten LJ. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Hum Reprod. 2006;21:2353–8.
Grace KS, Sinclair KD. Assisted reproductive technology, epigenetics, and long-term health: a developmental time bomb still ticking. Semin Reprod Med. 2009;27:409–16.
Shufaro Y, Laufer N. Epigenetic concerns in assisted reproduction: update and critical review of the current literature. Fertil Steril. 2013;99:605–6.
Kopeika J, Thornhill A, Khalaf Y. The effect of cryopreservation on the genome of gametes and embryos: principles of cryobiology and critical appraisal of the evidence. Hum Reprod Update. 2015;21:209–27.
Authors’ roles
BL and MBB contributed to the conception and design of the study, drafted the manuscript, and revised it. MBB performed the statistical analyses. BL, JE, and EW linked IVF cycles in the SART CORS database. All the authors contributed to the interpretation of the data and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Committees for the Protection of Human Subjects at the Dartmouth College, Michigan State University, and University of Michigan.
Conflict of interest
BL is a research consultant to the Society for Assisted Reproductive Technology (SART). EW is under contract with SART to maintain the SART CORS database. MBB, JES, JPT, and CCC have no conflicts to declare.
Additional information
Capsule Frozen embryo state is associated with an increased risk for LGA; the implications of these findings for childhood health and obesity risk are unclear.
Rights and permissions
About this article
Cite this article
Luke, B., Brown, M.B., Wantman, E. et al. Increased risk of large-for-gestational age birthweight in singleton siblings conceived with in vitro fertilization in frozen versus fresh cycles. J Assist Reprod Genet 34, 191–200 (2017). https://doi.org/10.1007/s10815-016-0850-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0850-x