Abstract
Purposes
Embryo quality is associated with successful implantation and live births. Our retrospective study was carried out to determine whether or not cleavage stage embryo quality affects the miscarriage rate, pregnancy complications and neonatal outcomes of singletons conceived with assisted reproduction technology.
Method
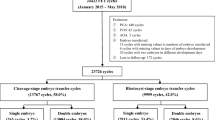
The current study included 11,721 In Vitro Fertilization-Embryo Transfer cycles (IVF-ET) between January 2009 (the date at which electronic medical records were implemented at our center) and March 2013. Only women < 40 years of age undergoing their first fresh embryo transfer cycle using non-donor oocytes were included.
Results
Our study indicated that the transfer of poor-quality embryos resulted in higher miscarriage (19.77 % vs. 13.28 %, p = 0.02) and lower ongoing pregnancy rates (15.33 % vs. 48.06 %, p < 0.001). Logistic regression analysis performed on data derived from 744 cycles culminating in miscarriages versus 4,333 cycles culminating in live births, suggested that embryo quality (p = 0.04) is significantly associated with miscarriage rate after adjusting for other confounding factors. Moreover, there were no differences in the mean birth weight, low birth weight (<2,500 g), very low birth weight (<1,500 g), gestational age, preterm delivery (<37 weeks), very preterm delivery (<32 weeks), congenital malformations, small-for-gestational-age singletons (SGA), and large-for-gestational-age singleton (LGA) rate (p > 0.05). Similarly, pregnancy complications resulting from poor-quality embryos were not different from good-quality embryos (4.04 % vs. 2.57 %, p = 0.33). Finally, logistic regression suggested that embryo quality was not significantly associated with pregnancy complications after adjusting for other confounding factors (p = 0.40).
Conclusions
Our study suggests that transfer of poor-quality embryos did not increase the risk of adverse outcomes; however, the quality of cleavage stage embryos significantly affected the miscarriage rate and ongoing pregnancies.
Similar content being viewed by others
References
Giorgetti C, Terriou P, Auquier P, Hans E, Spach JL, Salzmann J, et al. Embryo score to predict implantation after in-vitro fertilization: based on 957 single embryo transfers. Hum Reprod. 1995;10(9):2427–31.
Ziebe S, Petersen K, Lindenberg S, Andersen AG, Gabrielsen A, Andersen AN. Embryo morphology or cleavage stage: how to select the best embryos for transfer after in-vitro fertilization. Hum Reprod. 1997;12(7):1545–9.
Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, et al. Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod. 1999;14(9):2345–9.
Veleva Z, Orava M, Nuojua-Huttunen S, Tapanainen JS, Martikainen H. Factors affecting the outcome of frozen-thawed embryo transfer. Hum Reprod. 2013;28(9):2425–31. doi:10.1093/humrep/det251.
Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol. 2004;103(3):551–63. doi:10.1097/01.AOG.0000114989.84822.51.
McDonald SD, Han Z, Mulla S, Murphy KE, Beyene J, Ohlsson A. Preterm birth and low birth weight among in vitro fertilization singletons: a systematic review and meta-analyses. Eur J Obstet Gynecol Reprod Biol. 2009;146(2):138–48. doi:10.1016/j.ejogrb.2009.05.035.
McDonald SD, Han Z, Mulla S, Ohlsson A, Beyene J, Murphy KE. Preterm birth and low birth weight among in vitro fertilization twins: a systematic review and meta-analyses. Eur J Obstet Gynecol Reprod Biol. 2010;148(2):105–13. doi:10.1016/j.ejogrb.2009.09.019.
Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012;18(5):485–503. doi:10.1093/humupd/dms018.
Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Soderstrom-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19(2):87–104. doi:10.1093/humupd/dms044.
Kelley-Quon LI, Tseng CH, Janzen C, Shew SB. Congenital malformations associated with assisted reproductive technology: a California statewide analysis. J Pediatr Surg. 2013;48(6):1218–24. doi:10.1016/j.jpedsurg.2013.03.017.
Hansen M, Bower C. The impact of assisted reproductive technologies on intra-uterine growth and birth defects in singletons. Semin Fetal Neonatal Med. 2014;19(4):228–33. doi:10.1016/j.siny.2014.03.002.
El-Chaar D, Yang Q, Gao J, Bottomley J, Leader A, Wen SW, et al. Risk of birth defects increased in pregnancies conceived by assisted human reproduction. Fertil Steril. 2009;92(5):1557–61. doi:10.1016/j.fertnstert.2008.08.080.
Olson CK, Keppler-Noreuil KM, Romitti PA, Budelier WT, Ryan G, Sparks AE, et al. In vitro fertilization is associated with an increase in major birth defects. Fertil Steril. 2005;84(5):1308–15. doi:10.1016/j.fertnstert.2005.03.086.
Birth defects and congenital health risks in children conceived through assisted reproduction technology (ART): a meeting report. J Assist Reprod Genet. 2014;31(8):947–58. doi: 10.1007/s10815-014-0255-7.
Klemetti R, Gissler M, Sevon T, Koivurova S, Ritvanen A, Hemminki E. Children born after assisted fertilization have an increased rate of major congenital anomalies. Fertil Steril. 2005;84(5):1300–7. doi:10.1016/j.fertnstert.2005.03.085.
Wennerholm UB, Soderstrom-Anttila V, Bergh C, Aittomaki K, Hazekamp J, Nygren KG, et al. Children born after cryopreservation of embryos or oocytes: a systematic review of outcome data. Hum Reprod. 2009;24(9):2158–72. doi:10.1093/humrep/dep125.
Pelkonen S, Koivunen R, Gissler M, Nuojua-Huttunen S, Suikkari AM, Hyden-Granskog C, et al. Perinatal outcome of children born after frozen and fresh embryo transfer: the Finnish cohort study 1995–2006. Hum Reprod. 2010;25(4):914–23. doi:10.1093/humrep/dep477.
Pinborg A, Henningsen AA, Loft A, Malchau SS, Forman J, Andersen AN. Large baby syndrome in singletons born after frozen embryo transfer (FET): is it due to maternal factors or the cryotechnique? Hum Reprod. 2014;29(3):618–27. doi:10.1093/humrep/det440.
Ebner T, Yaman C, Moser M, Sommergruber M, Polz W, Tews G. Embryo fragmentation in vitro and its impact on treatment and pregnancy outcome. Fertil Steril. 2001;76(2):281–5.
Oron G, Son WY, Buckett W, Tulandi T, Holzer H. The association between embryo quality and perinatal outcome of singletons born after single embryo transfers: a pilot study. Hum Reprod. 2014. doi:10.1093/humrep/deu079.
Dumoulin JC, Land JA, Van Montfoort AP, Nelissen EC, Coonen E, Derhaag JG, et al. Effect of in vitro culture of human embryos on birthweight of newborns. Hum Reprod. 2010;25(3):605–12. doi:10.1093/humrep/dep456.
Nelissen EC, Van Montfoort AP, Coonen E, Derhaag JG, Geraedts JP, Smits LJ, et al. Further evidence that culture media affect perinatal outcome: findings after transfer of fresh and cryopreserved embryos. Hum Reprod. 2012;27(7):1966–76. doi:10.1093/humrep/des145.
Zhu J, Li M, Chen L, Liu P, Qiao J. The protein source in embryo culture media influences birthweight: a comparative study between G1 v5 and G1-PLUS v5. Hum Reprod. 2014. doi:10.1093/humrep/deu103.
Roos N, Kieler H, Sahlin L, Ekman-Ordeberg G, Falconer H, Stephansson O. Risk of adverse pregnancy outcomes in women with polycystic ovary syndrome: population based cohort study. BMJ. 2011;343:d6309. doi:10.1136/bmj.d6309.
Fridstrom M, Nisell H, Sjoblom P, Hillensjo T. Are women with polycystic ovary syndrome at an increased risk of pregnancy-induced hypertension and/or preeclampsia? Hypertens Pregnancy. 1999;18(1):73–80.
Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update. 2006;12(6):673–83. doi:10.1093/humupd/dml036.
Romundstad LB, Romundstad PR, Sunde A, von During V, Skjaerven R, Gunnell D, et al. Effects of technology or maternal factors on perinatal outcome after assisted fertilisation: a population-based cohort study. Lancet. 2008;372(9640):737–43. doi:10.1016/S0140-6736(08)61041-7.
Henningsen AK, Pinborg A, Lidegaard O, Vestergaard C, Forman JL, Andersen AN. Perinatal outcome of singleton siblings born after assisted reproductive technology and spontaneous conception: Danish national sibling-cohort study. Fertil Steril. 2011;95(3):959–63. doi:10.1016/j.fertnstert.2010.07.1075.
Balaban B, Urman B, Sertac A, Alatas C, Aksoy S, Mercan R. Blastocyst quality affects the success of blastocyst-stage embryo transfer. Fertil Steril. 2000;74(2):282–7.
Richter KS, Harris DC, Daneshmand ST, Shapiro BS. Quantitative grading of a human blastocyst: optimal inner cell mass size and shape. Fertil Steril. 2001;76(6):1157–67.
Ahlstrom A, Westin C, Reismer E, Wikland M, Hardarson T. Trophectoderm morphology: an important parameter for predicting live birth after single blastocyst transfer. Hum Reprod. 2011;26(12):3289–96. doi:10.1093/humrep/der325.
Hill MJ, Richter KS, Heitmann RJ, Graham JR, Tucker MJ, DeCherney AH, et al. Trophectoderm grade predicts outcomes of single-blastocyst transfers. Fertil Steril. 2013;99(5):1283–9 e1. doi:10.1016/j.fertnstert.2012.12.003.
Honnma H, Baba T, Sasaki M, Hashiba Y, Ohno H, Fukunaga T, et al. Trophectoderm morphology significantly affects the rates of ongoing pregnancy and miscarriage in frozen-thawed single-blastocyst transfer cycle in vitro fertilization. Fertil Steril. 2012;98(2):361–7. doi:10.1016/j.fertnstert.2012.05.014.
Acknowledgments
This study was funded by the National Natural Science Foundation of China for Young Scholars (81300483).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical statement
All human studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule The current study describes association between cleavage stage embryo quality and miscarriage based on 11721 IVF-ET cycles. However, embryo quality is not associated with obstetric and perinatal outcomes, transfer of poor-quality embryos is not responsible for a higher percentage of congenital malformations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Zhu, J., Lian, Y., Li, M. et al. Does IVF cleavage stage embryo quality affect pregnancy complications and neonatal outcomes in singleton gestations after double embryo transfers?. J Assist Reprod Genet 31, 1635–1641 (2014). https://doi.org/10.1007/s10815-014-0351-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-014-0351-8