Abstract
Purpose
To explore the prevalence and clinical features, especially the reproductive function, of 45,X mosaicism patients in northeast China.
Methods
GTG-banding was performed on a series of 2,250 patients from our genetic counseling clinic. Each of these patients underwent a physical examination and was interviewed about their medical history and reproductive problems. Literature on 45,X mosaicism was accessed using PubMed and reviewed.
Results
The prevalence of 45,X mosaicism in northeast China is 0.36 % (8/2250), and the mosaic karyotype of our study accounted for 61.54 % (8/13) of Turner syndrome cases. This is comparable with studies from Asia, Europe, South America and other regions. The affected patients showed genital abnormalities, abnormal pregnancy or infertility.
Conclusion
45,X mosaicism is commonly seen in the genetic counseling clinic. Extensive cytogenetic assessment may improve the detection rate in patients with congenital dysplasia, or history of abnormal pregnancy or infertility. Karyotyping plays a key role in prognosis and assisted reproduction or early surgical treatment.
Similar content being viewed by others
Introduction
Turner’s syndrome (TS) is characterized by a complete or partial absence of one X chromosome. Patients have a range of physical and skeletal features, in which final height and gonadal function are almost always affected. The disorder is thought to be caused by a haploinsufficiency of the escape genes [1] as the X chromosome is enriched for genes expressed in the brain, skeletal muscle, and in sex and reproduction-related tissues [2]. The first documented case of probable TS was amenorrhea in seven adolescent and young adult females with sexual infantilism, short stature, a webbed neck and cubitus valgus [3]. Since then, a number of other karyotype anomalies, such as mosaicisms and structural anomalies of the second X chromosome, have been found in association with TS.
Monosomy X (45,X) represents half of the karyotype spectrum of this syndrome, and the remainder includes structural X chromosome abnormalities or mosaicism for a cell line containing a second sex chromosome [4]. Fewer than 15 % of TS patients appear to have mosaicism with a 46,XY cell population or a Y chromosome rearrangement, 30–50 % are mosaic with a second X or a structurally abnormal X [5], while X/XX and X/XY individuals make up 15.5 % and 9.0 %, respectively, of TS patients [6]. Homer et al. [7] reported the frequency of 45,X/46,XX mosaicism to be 9.6 %, compared with an estimated 3.5 % of 45,X/46,XX in the overall female population by Peschka et al. [8].
Many of the TS cases previously described are characterized by variable phenotypes. Abnormalities in TS include short stature (95–100 %), primary amenorrhea (85 %), infertility (98 %), and characteristic stigmata [9]. In such cases, growth hormone therapy should be started at the age of 2–5, while hormone replacement therapy for the development of normal female sexual characteristics should begin between 12 and 15 years of age and be continued long-term to prevent the development of coronary artery disease and osteoporosis. Affected women also need to undergo genetic counseling prior to conception, followed by prenatal assessment. Moreover, TS patients with a Y or Y-derived chromosome have a 15 % increased risk of developing gonadoblastoma [10].
45,X mosaicism is commonly seen during clinical diagnosis or genetic counseling, and has multiple phenotypes. Ocal et al. [11] reported 11 cases (six females and five males) with ambiguous genitalia and/or delayed puberty with or without short stature. A study in the United States of nine females and seven males aged 15–17 years showed that while all had Müllerian structures (uterus and fallopian tubes), three girls had bilateral streak testes/gonads, nine children (six girls and three boys) had unilateral testes and contralateral streak testes/gonads, and four boys had bilateral testes, with signs of decreased virilization in one but normal male genitalia in the remaining three [12]. About 10–15 % of 45,X/46,XX patients have been reported to menstruate, some have follicles in their ovarian cortical tissue during adolescence, while some patients with a non-mosaic 45,X karyotype have even been reported to become pregnant [13].
Exploring ways to optimize the ovarian potential of TS patients is an area of ongoing interest that includes in vitro fertilization (IVF) and oocyte cryopreservation [14–16]. However, data suggest that even when pregnancy is spontaneously achieved in TS-Mosaic women, there is a marked increase in adverse outcomes. These concerns coupled with the inherently poor ovarian reserve in TS and TS-Mosaic patients have led to the emergence of donor oocyte IVF as a viable treatment option for patients. However, Brezina [17] showed that the rate of maternal X chromosome mosaicism does not affect pregnancy loss rates in TS-Mosaic women undergoing donor oocyte IVF.
Our study focused on the prevalence of 45,X mosaicism in patients from northeast China. To our knowledge, it is the first to evaluate this together with congenital dysplasia, histories of abnormal pregnancy or infertility and different clinical features on reproduction.
Materials and methods
Patients
Between August 2010 and June 2012, 2,250 TS cases aged between 18 and 39 years with congenital dysplasia and histories of abnormal pregnancy or infertility were collected from our genetic counseling clinic. Each patient underwent a physical examination and was interviewed about their medical histories and reproductive problems.
Semen analysis
Semen samples were obtained after a 5–7 day period of ejaculatory abstinence, and semen analysis was performed according to World Health Organization guidelines [18]. Semen parameters were assessed by using computer-assisted semen analysis (CASA). Each patient underwent semen analysis at least twice before a diagnosis of non-obstructive azoospermia or oligozoospermia was made. Patients with obstructive azoospermia were excluded from this study.
Cytogenetic studies
Cytogenetic studies were performed using G-banding in peripheral blood lymphocytes according to standard techniques [19]. Briefly, peripheral blood lymphocytes were cultured for 72 h in RPMI medium 1640 (GIBCO, Invitrogen, Carlsbad, CA, USA) and fetal bovine serum (Beijing Dingguo Biotechnology, Beijing, China) containing phytohemagglutinin (Shang-hai Yihua Medical Technology Co., Ltd., Shanghai, China), treated with 50 μg/ml colcemid for 1 h, then harvested for analysis. G-banding of metaphase chromosomes was performed by Giemsa staining. At least 20 metaphase cells were analyzed per patient. The procedure was repeated in all cases with abnormal karyotypes. Chromosomal abnormalities were described according to the International System for Human Cytogenetic Nomenclature.
Results
Of the 2,250 patients with congenital dysplasia, abnormal pregnancy history or infertility, 13 cases had 45,X or 45,X mosaicism and eight had 45,X mosaicism, giving a prevalence of 0.36 % (8/2,250) and accounting for 61.54 % (8/13) of TS patients, respectively. Of these eight patients, 37.5 % (3/8) were mosaic with a second X or X trisomy, with no structurally abnormal X chromosome. Five of the eight patients (62.5 %) had mosaicism with a 46,XY cell population or a Y chromosome rearrangement (Table 1).
There were three female cases of 45,X mosaicism; one was amenorrheic, the second had experienced embryonic diapause twice, while the third with 45,X [5]/ 47,XXX [31] /46,XX [14] was receiving IVF treatment. The remaining five male cases with 45,X monoploidy were azoospermic or oligozoospermic (Table 1).
Discussion
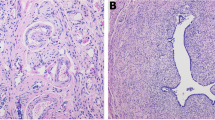
The prevalence of 45,X mosaicism in current TS research differs according to population, but the range is relatively stable. A previous study found a 45,X/46,XX mosaicism frequency of approximately 15 % in TS patients [6], while Kuo [20] reported a 45,X/46,XX mosaicism incidence rate of 25 % in repeated spontaneous abortion patients. In the present study, there were three females with 45,X mosaicism (Table 1), and the prevalence of karyotype 45,X/46,XX or 45,X/47,XXX/46,XX in our study was only slightly lower than in other reported Asian regions (Table 2). Although our prevalence of 45, X/46, XY mosaicism (Fig. 1) was higher than in most other regions, it is comparable with a study by Kannan [6] (Table 2).
It has previously been reported that patients with 6–28 % aneuploidy and 45,X/46,XX mosaicism showed the clinical manifestations of premature ovarian failure or recurrent spontaneous abortions. However, the extent of these symptoms appears to have no adverse effect on the outcomes of IVF or intracytoplasmic sperm injection (ICSI) [7]. Patients with more than 6 % aneuploidy often have an increased body mass index [21], and Oktay et al. [22] reported on one such patient with karyotype 45,X [45 %]/46,XX [55 %], a large proportion of aneuploidy and irregular menstrual periods. The study concluded that controlled ovarian stimulation and oocyte cryopreservation may be an option for fertility preservation in selected adolescents with TS mosaicism and impending ovarian failure.
Triple X (47,XXX) females occur in approximately 1/1,000 females and have no recognized characteristic phenotype. They do, however, show a significantly elevated mortality with a standardized mortality ratio of 2.5 or an approximately 7-year shortened lifespan [23]. We observed one case of a 39-year-old 45,X [72 %]/47, XXX [28 %] female who twice experienced embryonic diapause in the present study. Other similar cases include a 45,X [90 %]/47,XXX [10 %] patient with secondary amenorrhea, weight loss and streak-like ovaries [24]. However, one 45,X/47,XXX case has reported to achieve two successful pregnancies [25, 26].
One male case of 46,X,dic(Y) [78 %]/45,X [22 %] in the present study was azoospermic, which is comparable with frequencies in a similar Japanese study [27]. In addition, García Benítez et al. [28] reported one female patient with 30 % aneuploidy (46,X, dic(Y) [70 %]/45,X [30 %]) with clinical features of primary amenorrhea and congenital adrenal hyperplasia. Compared with our study, these abnormalities may relate to the proportion of aneuploidy. Another previous study reported three cases of 45,X /47,XYY (one male and two females) with mixed gonadal dysgenesis (MGD) [29].
The prenatal diagnosis of 45,X/46,XY mosaicism occurs in approximately 1.7 per 10,000 prenatal samples. The phenotype ranges from 90 % of normal male fetuses to postnatal features that include a wide spectrum of phenotypes such as hypospadias [30]. Affected males can benefit from assisted reproductive therapies, but prenatal diagnosis plays an important role in preventing the transmission of genetic abnormalities [31, 32]. Kilic et al. [33] reported on three cases with different degrees of 45,X monoploidy, which compares with the three cases in our own study: two with 45,X [60 %]/46,XY [40 %] and 45,X [58 %]/46,XY [42 %] were azoospermic while the third with 45,X [6]/46,XY [26] was oligospermic (Table 2).
Thus, the 45,X mosaicism karyotype has obvious effects on reproduction. As the proportion of aneuploidy is much larger, it may lead to more serious results such as azoospermia and severe oligospermia. However, there is no obvious relationship between the percentage of mosaicism (the number of 45,X cells relative to the total number of cells) and the presence or degree of abnormalities, suggesting that mosaicism is not the only cause of these.
In conclusion, the occurrence of 45,X mosaicism makes it necessary to undertake chromosome karyotype analysis in patients suffering from fertility problems or with obvious abnormal symptoms. Accurate diagnosis can provide information and evidence for assisted reproduction or early surgical treatment.
References
Yang C, Chapman AG, Kelsey AD, Minks J, Cotton AM, Brown CJ. X-chromosome inactivation: molecular mechanisms from the human perspective. Hum Genet. 2011;130(2):175–85.
Vallender EJ, Lahn BT. How mammalian sex chromosomes acquired their peculiar gene content. Bioessays. 2004;26(2):159–69.
Turner HH. A syndrome of infantilism, congenital webbed neck, and cubitus valgus. Endocrinology. 1938;23:566–74.
Portnoï MF, Chantot-Bastaraud S, Christin-Maitre S, Carbonne B, Beaujard MP, Keren B, et al. Familial Turner syndrome with an X;Y translocation mosaicism: implications for genetic counseling, Eur J Med Genet. 2012. [Epub ahead of print].
Wiktor A, Van Dyke DL. FISH analysis helps identify low-level mosaicism in Ullrich-Turner syndrome patients. Genet Med. 2004;6(3):132–5.
Kannan TP, Azman BZ, Ahmad Tarmizi AB, Suhaida MA, Siti Mariam I, Ravindran A, et al. Turner syndrome diagnosed in northeastern Malaysia. Singap Med J. 2008;49(5):400–4.
Homer L, Morel F, Gallon F, Le Martelot MT, Amice V, Kerlan V, et al. Does 45, X/46, XX mosaicism with 6–28 % of aneuploidy affect the outcomes of IVF or ICSI? Eur J Obstet Gynecol Reprod Biol. 2012;163(1):47–51.
Peschka B, Leygraaf J, Van der Ven K, Montag M, Schartmann B, Schubert R, et al. Type and frequency of chromosome aberrations in 781 couples undergoing intracytoplasmic sperm injection. Hum Reprod. 1999;14(9):2257–63.
Hovatta O. Pregnancies in women with Turner’s syndrome. Ann Med. 1999;31(2):106–10.
Cools M, Drop SL, Wolffenbuttel KP, Oosterhuis JW, Looijenga LH. Germ cell tumors in the intersex gonad: old paths, new directions,moving frontiers. Endocr Rev. 2006;27(5):468–84.
Ocal G, Berberoğlu M, Sıklar Z, Ruhi HI, Tükün A, Camtosun E, et al. The clinical and genetic heterogeneity of mixed gonadal dysgenes is: does “disorders of sexual development (DSD)”classification based on new Chicago consensus cover all sex chromoso me DSD? Eur J Pediatr. 2012;171(10):1497–502.
Tosson H, Rose SR, Gartner LA. Description of children with 45,X/46,XY karyotype. Eur J Pediatr. 2012;171(3):521–9.
Cools M, Rooman RP, Wauters J, Jacqemyn Y, Du Caju MV. A nonmosaic 45, X karyotype in a mother with Turner’s syndrome and in her daughter. Fertil Steril. 2004;82(4):923–5.
El-Shawarby SA, Sharif F, Conway G, Serhal P, Davies M. Oocyte cryopreservation after controlled ovarian hyperstimulation in mosaic Turner syndrome: another fertility preservation option in a dedicated UK clinic. BJOG. 2010;117(2):234–7.
Lau NM, Huang JY, MacDonald S, Elizur S, Gidoni Y, Holzer H, et al. Feasibility of fertility preservation in young females with Turner syndrome. Reprod Biomed Online. 2009;18(2):290–5.
Balen AH, Harris SE, Chambers EL, Picton HM. Conservation of fertility and oocyte genetics in a young woman with mosaic Turner syndrome. BJOG. 2010;117(2):238–42.
Brezina PR, Christianson MS, Nguyen KHD, Siegel A, Benner AT, Kearns WG. Maternal XX/X chromosome mosaicism in donor oocyte in vitro fertilization (IVF). Middle East Fertil Soc J. 2012;17(2):129–33.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interac-tion. 4th ed. Cambridge: Cambridge University Press; 1999.
Male Infertility Best Practice Policy Committee of the American Urological Association, Practice Committee of the American Society for Reproductive Medicine. Report on optimal evaluation of the infertile male. Fertil Steril. 2006;86:S202–9.
Kuo PL, Guo HR. Mechanism of recurrent spontaneous abortions in women with mosaicism of X-chromosome aneuploidies. Fertil Steril. 2004;82(6):1594–601.
Homer L, Le Martelot MT, Morel F, Amice V, Kerlan V, Collet M, et al. 45, X/46, XX mosaicism below 30 % of aneuploidy: clinical implications in adult women from a re productive medicine unit. Eur J Endocrinol. 2010;162(3):617–23.
Oktay K, Rodriguez-Wallberg KA, Sahin G. Fertility preservation by ovarian stimulation and oocyte cryopreservation in a 14-year-old adolescent with Turner syndrome mosaicism and impending premature ovarian failure. Fertil Steril. 2010;94(2):753.e15–9.
Stochholm K, Juul S, Gravholt CH. Mortality and incidence in women with 47, XXX and variants. Am J Med Genet A. 2010;152A(2):367–72.
Tauchmanovà L, Rossi R, Pulcrano M, Tarantino L, Baldi C, Lombardi G. Turner’s syndrome mosaicism 45X/47XXX: an interesting natural history. J Endocrinol Invest. 2001;24(10):811–5.
Bouchlariotou S, Tsikouras P, Dimitraki M, Athanasiadis A, Papoulidis I, Maroulis G, Liberis A, Liberis V. Turner’s syndrome and pregnancy: has the 45, X/47, XXX mosaicism a different prognosis? Own clinical experience and literature review. J Matern Fetal Neonatal Med. 2011;24(5):668–72.
Alves C, Silva SF. Spontaneous procreation in Turner syndrome: report of two pregnancies in the same patient. Syst Biol Reprod Med. 2012;58(2):113–5.
Yoshida A, Nakahori Y, Kuroki Y, Motoyama M, Araki Y, Miura K, Shirai M. Dicentric Y chromosome in an azoospermic male. Mol Hum Reprod. 1997;3(8):709–12.
García Benítez Y, Muñoz-Boyero AC, Santos Reyero M, Alonso-Cerezo MC. Sexual development disorder in a patient 45,X/46,X,DIC(Y). Endocrinol Nutr. 2012;59(4):268–70.
Farrugia MK, Sebire NJ, Achermann JC, Eisawi A, Duffy PG, Mushtaq I. Clinical and gonadal features and early surgical management of 45,X/46,XY and 45,X/47,XYY chromosomal mosaicism presenting with genital anomalies. J Pediatr Urol. 2012. [Epub ahead of print].
Barone C, Bartoloni G, Cataliotti A, Indaco L, Pappalardo E, Barrano B, et al. Prenatal diagnosis of 45, X/46, XY mosaicism with cleft lip and epispadias. Arch Gynecol Obstet. 2011;284(2):509–11.
Franceschini G, D’Alba P, Costantini M, Magistrelli A, Belli P, Mulè A, Coco C, et al. Synchronous bilateral breast carcinoma in a 50-year-old man with 45, X/46, XY mosaic karyotype: report of a case. Surg Today. 2006;36(1):71–5.
Preusser S, Diener PA, l’Allemand-Jander D, Schmid S, Leippold T, Brändle M, et al. Scrotal hysterectomy in a male patient with mixed gonadal dysgenesis 46,XY(75%)/45,X(25%). Urology. 2007;70(6):1223.e7–9.
Kilic S, Yukse B, Tasdemir N, Dogan M, Ozdemir E, Yesilyurt A, et al. Assisted reproductive treatment applications in men with normal phenotype but 45, X/46, XYmosaic karyotype: clinical and genetic perspectives. Taiwan J Obstet Gynecol. 2010;49(2):199–202.
Abir R, Fisch B, Nahum R, Orvieto R, Nitke S, Ben Rafael Z. Turner’s syndrome and fertility: current status and possible putative prospects. Hum Reprod Update. 2001;7(6):603–10.
Chang GY, Dong ZY, Wang W, Xiao Y, Chen FS, Ni JH, et al. Association of 45, X/46, XY mosaicism with disorders of sex development: the clinical analysis of 5 cases. Zhonghua Er Ke Za Zhi. 2011;49(6):451–4.
Brambila-Tapia AJ, Rivera H, García-Castillo H, Domínguez-Quezada MG, Dávalos-Rodríguez IP. 47,XXX/45,X/46,XX mosaicism in a patient with Turner phenotype and spontaneous puberal development. Fertil Steril. 2009;92(5):1747.e5–7.
ALvarez-Nava F, Soto M, Sánchez MA, Fernández E, Lanes R. Molecular analysis in Turner syndrome. J Pediatr. 2003;142(3):336–40.
Marzuki NS, Anggaratri HW, Suciati LP, Ambarwati DD, Paramayuda C, Kartapradja H, et al. Diversity of sex chromosome abnormalities in a cohort of 95 Indonesian patients with monosomy X. Mol Cytogenet. 2011;4:23.
Akgul M, Ozkinay F, Ercal D, Cogulu O, Dogan O, Altay B, et al. Cytogenetic abnormalitie s in 179 cases with male infertility in Western Region of Turkey: report and review. J Assist Reprod Genet. 2009;26(2–3):119–22.
Acknowledgments
We would like to thank the staff of the andrology and genetics laboratory for their excellent work. This work was supported by funds from the National Population and Family Planning Commission of China (No. 2011-GJKJS-07).
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Evaluated the prevalence and clinical features, especially reproductive function of 45,X mosaicism patients in Northeast of China.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Liu, XY., Zhang, HG., Chen, S. et al. 45,X mosaicism in northeast China: a clinical report and review of the literature. J Assist Reprod Genet 30, 407–412 (2013). https://doi.org/10.1007/s10815-012-9927-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-012-9927-3