Abstract
Purpose
The negative correlation between fecundity and age in women has been extensively documented although data on reproductive performance in very young women is sparse. The objective of this study was to determine whether age ≤25 years has an impact on reproductive outcome in women undergoing IVF-ET.
Methods
IVF outcome in 85 infertility patients aged 19–25 years was compared to that in 69 infertility patients aged 30–35 years. Primary outcomes included fertilization rates and embryo quality. Secondary outcomes were clinical pregnancy and miscarriage rates.
Results
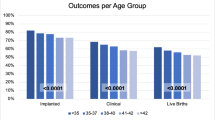
The young patients (≤25 years) demonstrated a lower fertilization rate, and reduced number of top quality embryos. Although clinical pregnancy, and implantation rates were similar to their older counterparts (30–35 years), the young women had a significantly higher miscarriage rate.
Conclusion
Our results demonstrating poorer reproductive performance in very young patients were surprising and need further investigation.

Similar content being viewed by others
References
Bentov Y, Esfandiari N, Burstein E, Casper RF. The use of mitochondrial nutrients to improve the outcome of infertility treatment in older patients. Fertil Steril. 2010;93(1):272–5.
Munné S, Sandalinas M, Magli C, Gianaroli L, Cohen J, Warburton D. Increased rate of aneuploid embryos in young women with previous aneuploid conceptions. Prenat Diagn. 2004;24(8):638–43.
Fragouli E, Escalona A, Gutiérrez-Mateo C, Tormasi S, Alfarawati S, Sepulveda S, et al. Comparative genomic hybridization of oocytes and first polar bodies from young donors. Reprod Biomed Online. 2009;19(2):228–37.
Rodríguez-González M, Serra V, Garcia-Velasco JA, Pellicer A, Remohí J. The “vanishing embryo” phenomenon in an oocyte donation programme. Hum Reprod. 2002;17(3):798–802.
World Health Organization. WHO laboratory manual for the examination of human sperm and semen-cervical mucus interaction. 4th ed. New York: Cambridge University Press; 1999.
Casper RF, Meriano JS, Jarvi KA, Cowan L, Lucato ML. The hypo-osmotic swelling test for selection of viable sperm for intracytoplasmic sperm injection in men with complete asthenozoospermia. Fertil Steril. 1996;65(5):972–6.
Jurisicova A, Varmuza S, Casper RF. Programmed cell death and human embryo fragmentation. Mol Hum Reprod. 1996;2:93–8.
Ziebe S, Lundin K, Loft A, Bergh C. Nyboe Andersen A, Selleskog U, et al. FISH analysis for chromosomes 13, 16, 18, 21, 22, X and Y in all blastomeres of IVF pre-embryos from 144 randomly selected donated human oocytes and impact on pre-embryo morphology. Hum Reprod. 2003;18:2575–81.
Wilding M, Di Matteo L, Dale B. The maternal age effect: a hypothesis based on oxidative phosphorylation. Zygote. 2005;13(4):317–23.
Bartmann AK, Romão GS, Ramos Eda S, Ferriani RA. Why do older women have poor implantation rates? A possible role of the mitochondria. J Assist Reprod Genet. 2004;21(3):79–83.
Simón C, Cano F, Valbueña D, Remohí J, Pellicer A. Clinical evidence for a detrimental effect on uterine receptivity of high serum oestradiol concentrations in high and normal responder patients. Hum Reprod. 1995;10:2432–7.
Valbuena D, Martin J, de Pablo JL, Remohí J, Pellicer A, Simón C. Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76:962–8.
Chun SY, Hsueh AJ. Paracrine mechanisms of ovarian follicle apoptosis. J Reprod Immunol. 1998;39(1–2):63–75.
Nelson JR, Feinman M, Wilcox J, Batzofin J. Preimplantation genetic diagnosis in embryos created from oocyte donation. Fertil Steril 2001 pp. S76 ASRM abstract.
Munné S, Ary J, Zouves C, Escudero T, Barnes F, Cinioglu C, et al. Wide range of chromosome abnormalities in the embryos of young egg donors. Reprod Biomed Online. 2006;12(3):340–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Our results demonstrated that very young women had poorer reproductive performance compared to patients in their early thirties.
Rights and permissions
About this article
Cite this article
Nazemian, Z., Esfandiari, N., Javed, M. et al. The effect of age on in vitro fertilization outcome: is too young possible?. J Assist Reprod Genet 28, 101–106 (2011). https://doi.org/10.1007/s10815-010-9499-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-010-9499-z