Abstract
Therapeutic riding (THR) and HeartMath (HM) mindfulness-based interventions have promise for reducing stress in adolescents with autism spectrum disorder. In three 10-week periods, this study compared THR, HM, and control on salivary cortisol, self-reported stress, parent-reported social responsiveness, and heart-rate variability. This crossover design included 27 participants (12–21 years) randomly assigned to order of intervention. Findings suggest that HM and THR manualized protocols are equally beneficial in decreasing cortisol levels immediately following a session, but HM sessions had more impact on heart-rate variability. There was no significant effect on follow-up cortisol levels within a week after either intervention, but THR had more impact on decreasing some self-reported stressors.
Similar content being viewed by others
Introduction
The need for non-pharmacological interventions for adolescents with autism spectrum disorders (ASD) has grown. In 2014, in the United States, the prevalence rate of ASD was 1 in 59 eight-year old children (Baio et al., 2018). As this group reaches adolescence, just like any developing adolescent, they have the need for autonomy, competence, and belonging for successful transition (Deci & Ryan, 2012; Roeser & Zelazo, 2012). Moreover, youth on the autism spectrum have higher rates of stress and social anxiety, especially in the context of mainstream school settings (Bennett et al., 2018; Hebron & Humphrey, 2014; Kreiser & White, 2014; Lai et al., 2019; Spain et al., 2019; Zainal & Magiati, 2019). In addition to the hallmarks of ASD in DSM-5, consisting of persistent deficits in communication/social interaction and restricted, repetitive behaviors (American Psychiatric Association, 2013), approximately 70% of individuals with ASD have one mental health co-morbidity impacting their quality of life (Kuhlthau et al., 2017; White et al., 2009). Van Steensel et al., (2011) found that 36.6% of autistic children under 18 have a co-morbid anxiety disorder which includes phobia (29.8%), obsessive–compulsive disorder (17.4%) and social anxiety (16.6%). Adolescents with ASD report more solitary than social activities and difficulty forming and maintaining relationships (Hilton et al., 2008; Mazefsky et al., 2013; Orsmond & Kuo, 2011; Seltzer et al., 2004). Evidence exists that social stress levels and fear of negative evaluation in social settings, especially in the transition to adulthood, are related to social interaction patterns (Capriola et al., 2017; Corbett & Simon, 2014; Maddox & White, 2015; Picci & Scherf, 2015; Pickard et al., 2017; Taylor & Seltzer, 2012; White et al., 2014). Unfortunately, social anxiety in adolescents with ASD can impede adolescent developmental tasks, adaptive behaviors, and independent function in adult life (e.g. forming love relationships, and employment) (McGeowen et al., 2013; Picci & Scherf, 2015; Taylor & Seltzer, 2012). Finding evidence of an effective way, without medication, to address stress in young adults with ASD, will have implications for overall wellness and quality of life (Hong et al., 2016; Shattuck et al., 2007).
Stress and Autism
Stress refers to body’s reaction in response to events, including activation of primary stress systems, such as the hypothalamic-pituitary-adrenocortical (HPA) axis (Porges, 2018). Both the social context and the perception of the stressor are important in the way neurological and physiological aspects of social contact influences stress for people with ASD (Bishop-Fitzpatrick et al., 2017; Corbett et al., 2019). When individuals perceive external demands exceeding his/her resources, coping with stress requires both cognitive and behavioral actions to meet the demands (Lazarus & Folkman, 1984). When compared to typical peers in the community, adults with ASD have significantly higher perceived stress and stressful life events (Bishop-Fitzpatrick et al., 2017; Bitsika & Sharpley, 2015) and poorer ability to cope with stress in everyday life (Hirvikoski & Blomqvist, 2015; Tomarken et al., 2015). In fact, the higher the individual’s autism spectrum quotient (AQ) score, the more subjective stress/distress in everyday life (Hirviskoski & Blomqvist, 2015). For youth with ASD who are transitioning into adulthood, elevated stress levels may translate into: (1) lack of emotional regulation, sleep disturbances (Goldman et al., 2017), and poor subjective quality of life and life adjustment (Bishop-Fitzpatrick et al., 2017; Hong et al., 2016); (2) interference with learning capability in school (Stahmer & Aarons, 2009); (3) and diminished ability to complete activities of daily living (Muris et al., 1998). Anxiety relates to the anticipation and apprehension related to interaction with the environment (Corbett & Simon, 2014). While anxiety is a separate construct from perceived and objective stress, stress and anxiety are related (Corbett & Simon, 2014; Lanni et al., 2012; White et al., 2009). Prolonged repetition of stress, especially during adolescent transition, may create poor regulation of the HPA axis and difficulty with emotional regulation (Corbett & Simon, 2014). Potential interventions that decrease stress, promote resilience, and support positive transition may improve treatment for people with ASD (Bishop-Fitzpatrick et al., 2017; Corbett & Simon, 2014).
Cortisol and Autism
Cortisol is used as a reliable indicator of physiological arousal (Taylor & Corbett, 2014). Salivary “free” cortisol is an effective and valid way to assess transient changes in the activity of the HPA axis (Hertz et al., 2015; Shirtcliff et al., 2012). Both perceived and actual threat, such as a new event, lack of predictability, no control over events, and an evaluation of social threat, can activate the HPA axis (Dickerson & Kemeny, 2004; Spolskay et al., 2000) and release cortisol, a hormone, from the adrenal cortices (Fung, 2016; Herman & Cullinan, 1997). High levels of salivary cortisol have been linked to distress, negative affect, lack of cognitive flexibility, and social anxiety in youth (Gordis et al., 2006; Plessow et al., 2011; Thayer et al., 1996).
Typically, cortisol peaks early in the morning with rapid increase after rising, known as the cortisol awakening response increase (CARi) (Chida & Steptoe, 2009). During the day, cortisol values decline and the lowest levels are in the evening (Corbett & Simon, 2014). Goldman et al. (2017) found similar cortisol levels in individuals with and without ASD. However, other studies have found differences. When compared to those who do not have ASD, adolescents with ASD have elevated evening cortisol levels (Muscatello & Corbett, 2018; Tomarken et al., 2015) with evidence of a blunted diurnal slope; a more stable level of cortisol throughout most of the day rather than a decline that is seen in typical adolescents (Edmiston et al., 2017; Taylor & Corbett, 2014; Tomarken et al., 2015; Tordjman et al., 2014). Some adults with ASD, without a co-morbid diagnosis of anxiety and/or depression, exhibit low cortisol levels throughout the day suggesting disregulation of the HPA axis (Baker et al., 2019). Another study found a small proportion of adolescents with ASD lacked a decline of cortisol throughout the day, indicating dysregulation of the diurnal rhythm (Bitsika et al., 2017). Likewise, evidence suggests that elevated evening cortisol levels in adults with ASD are associated with poor sleep (Baker et al., 2019). It has been suggested that cortisol response in adolescents with ASD is different because the regions of the brain impacted by ASD such as the hippocampus, prefrontal cortex, and the amygdala share connections with the HPA axis (Corbett & Simon, 2014; Muscatello & Corbett, 2018).
Emotional Regulation, Heart Rate Variability, and Autism
Emotional regulation involves the person’s ability to change their emotional responses independently for positive functioning, including the processes by which individuals modulate their emotional state through strategies (Reyes et al., 2019) and is associated with better mental health (Hu et al., 2014). Unfortunately, individuals with ASD often display autonomic nervous system (ANS) dysfunction (Benevides & Lane, 2013) with poor emotional regulation, including irritability, and more negative emotional reactions under stress (Quek et al., 2012), less use of cognitive appraisal, more repetitive behaviors (Samson et al., 2015a, 2015b), and less self-soothing behaviors than other developing adolescents (Edmiston et al., 2017). Since an improvement in emotional regulation could benefit both interpersonal relationships and successful transition to adulthood through work or further education, interventions that improve emotional regulation should be considered (Mazefsky et al., 2013; Reyes et al., 2019).
Researchers have assessed the effect of the ability to self-regulate negative emotions on the activity of the autonomic nervous system (McCraty et al., 1998, 2009). Heart rate variability (HRV) reflects the individual’s ability to adapt to stress and environmental demands. Researchers have linked vagally-mediated HRV to self-regulation (Reynard et al., 2011), emotional regulation (Geisler et al., 2010) and social interaction (Geisler et al., 2013). Heart rhythm patterns reflect the dynamics and provide information on the degree of synchronized activity or coherence. Coherence is the opposite of stress in that it is measure of the stability and order of the heart rhythm (McCraty & Zayas, 2014). Positive emotions such as appreciation, care, and love generate a smoother sine-wave like pattern in the heart’s rhythms (McCraty & Tomasino, 2006; McCraty et al., 1998).
Recreational Therapy Interventions for Stress Management
Currently, recreational therapists, as well as other disciplines, use both animal-assisted interventions and mindfulness techniques in their practice with youth with autism to address stress management and emotional regulation especially with regard to transition goals related to social independence. Since lack of self-regulation in the face of high levels of stress in social settings is a barrier to social interaction and independence in the community (Maisel et al., 2016), recreational therapists use protocol-driven interventions to manage stress in social situations (Abishira et al., 2020; Kemeny et al., 2019). Therapeutic horseback riding (THR), a specific modality of animal-assisted interventions using horses, has been studied primarily with children with autism up to 18 years of age (Abihsira et al., 2020; Goodwin et al., 2016; Kemeny et al., 2019). Research also exists on mindfulness as a stress management modality for youth on the autism spectrum (Bemmer et al., 2021).
Therapeutic Horseback Riding
Most animal-assisted interventions research with people with autism has focused on horses and dogs (O’Haire, 2017). Less research has been conducted with other animals such as dolphins and guinea pigs (O’Haire, 2017). In canine-assisted interventions research, touching the animal is an important link to stress reduction (Wijker et al., 2019, 2020), and time-on-task (Hill et al., 2020). Moreover, studies using parent-report suggest that interaction with dogs improves social communication (e.g. giving commands and prompting questions) and emotional regulation (e.g. self-calming) and better understanding of their emotional state (Berry et al., 2013; London et al., 2020). The human-animal interaction has been shown to decrease arousal (Barker et al., 2010; Odendaal & Meintjes, 2003) and social stress through a positive focus of attention (Fine & Beck, 2015). In an exploration of service dogs living with a child with autism, Viau et al. (2010) found a reduction in the stress-related cortisol level only during the time that the dog was with the family, suggesting sensitivity of the measure to the human-animal bond. There is some evidence that when a youth with autism interacts with animals, they perceive a greater reward and less sense of threat (Solomon, 2012; Whyte et al., 2015).
Like canine-assisted interventions, equine-assisted services (EAS) are promising for adolescents with autism for multiple reasons: (1) horses prefer routine (Arnold, 2015; Dunlop & Tsantefski, 2017); (2) horses communicate without verbal exchange and provide opportunities for reciprocal interaction (Arnold, 2015); (3) riders often express sense of self-efficacy and control based on directing the horse or caring for the horse (Dunlop & Tsantefski, 2017; Goodwin et al., 2016); (4) EAS may produce a regulated state of arousal by providing rhythm, proprioceptive, and tactile opportunities that can promote relaxation through vestibular-cerebellar stimulation (Arnold et al., 2015; Gabriels et al., 2012; Souza-Santos et al., 2018); (5) EAS promote a sense of safety and calm (Dunlap & Tsantefski, 2017); and (6) EAS increase brain connectivity from the cerebellum to central and prefrontal cortices (Hyun et al., 2016).
Therapeutic horseback riding is a subset of EAS. Research with younger children with ASD, ages 2–16, suggests that THR improves spontaneous verbalization (Holm et al., 2014), inattention, distractibility (Bass et al., 2009), irritability, hyperactivity, self-regulation (Abishira et al., 2020; Gabriels et al., 2012, 2015; Pan et al., 2019), autistic behaviors, adaptive behaviors, and receptive communication skills (Ajzenman et al., 2013; Lanning et al., 2014), social functioning (Abishira et al., 2020; Anderson & Meints, 2016; Harris & Williams, 2017) and quality of life (Kern, 2011). Using meta-analytic technique, Trzmiel et al. (2019) found evidence that for ages 6–16, EAS promoted improved socialization, engagement, and decreased maladaptive behaviors.
Mindfulness Interventions and Autism
Mindfulness is another widely used intervention to support coping skills and stress management. Polyvagal-informed treatment (Porges, 2018) supports emotional regulation. Porges (2018) describes polyvagal theory interventions that promote an optimal state of safety in which the autonomic system in not in defense mode, the social engagement system regulates the sympathetic nervous system and dorsal vagal circuit, and the environment provides cues of safety. Taking advantage of neuroplasticity during adolescence, mindfulness training over an extended period of time is associated with modification of cognitive and emotional processes that become second nature, supporting academic success and well-being (Moffitt et al., 2011; Oberle & Schonert-Reichl, 2014).
One example of stress management treatment, cognitive behavioral therapy (CBT), which challenges cognitive distortions and seeks to promote coping skills and emotional regulation, has been used for people with ASD to reduce fear and avoidance of social situations (Bemmer et al., 2021; Scarpa et al., 2013; Sofronoff et al., 2007; Ung et al., 2015; Vasa et al., 2016; Wood et al., 2009). However, due to the cognitive processes involved in thought restructuring, CBT may not be appropriate for every adolescent with autism (Lickel et al., 2012). Mindfulness-based interventions (Oberle & Schonert-Reichl, 2014), in which the adolescent learns resilience by becoming more aware of their internal state and how to tolerate stressful situations, are recognized by some as a more effective avenue for emotional regulation for people with ASD (Scarpa et al., 2013). When comparing CBT and mindfulness therapy, Sizoo and Kuiper (2017) found that both interventions were equally effective in treating anxiety and depression with respect to autistic symptoms, rumination, and global mood. However, mindfulness was a preferred technique for people with ASD and co-morbid anxiety.
The main outcomes of mindfulness-based interventions are emotional regulation, increased awareness, and anatomical changes in areas associated with cortical regulation (Gu et al., 2015; Holzel et al., 2011; Ives-Deliperi et al., 2011). While there are different mindfulness interventions, one Mindfulness-Based Stress Reduction group program addresses distress and teaches coping skills to deal with symptoms of anxiety (Fjorback et al., 2011).
As a result of mindfulness interventions, a person learns to direct their attention internally and avoid the “automatic pilot” that takes over the brain when stressed (Cachia et al., 2016). Some research exists with the use of modifications of mindfulness interventions (EASE, MyMind) to improve emotional regulation, impulse control, emotional acceptance (Conner & White, 2018; Conner et al., 2019; Salem-Guirgis et al., 2019), anxiety and rumination (Spek et al., 2013), quality of life (Ridderinkhof et al., 2018), attention (Ridderinkhof et al., 2020); and aggression (Singh et al., 2011). While some studies did modify the mindfulness intervention to decrease the use of metaphors and shorter sessions for people with autism (Conner & White, 2018; Kiep et al., 2015; Sizoo & Kuiper, 2017), it is unclear what improvement these modifications made for participants.
HeartMath (HM) is a well-established, structured program aimed at improving mental and emotional self-regulation among youth and adults (HeartMath Institute, 2015). The modular program, displayed in visual format, requires a facilitator certification, consists of mental and emotional self-regulation and mindfulness techniques that use pictures and concrete examples (e.g. anchoring a positive thought) (HeartMath Institute, 2015). When an individual has inappropriate ANS arousal, reduced heart-rate variability, and emotional dysregulation, HM techniques are designed to self-regulate stress (McCraty & Zayas, 2014). The first step of most of the techniques is “heart-focused breathing” which includes putting one’s attention in the chest center and breathing using visualization. Deliberate regulation of breathing at 10 s rhythm increases cardiac coherence (McCraty & Zayas, 2014). After this technique is learned and strong emotions are experienced, breathing decreases the intensity of the reaction. With conscious control of breathing over time, it allows the participant to modulate and gradually increase stability of the vagal afferent nerve traffic, sympathetic outflow, and the emotional experience (McCraty et al., 2009). The method also depends on the shift to increased cardiac coherence with self-induced positive emotions (McCraty et al., 2014). Mindfulness has been associated with lower cortisol levels during conflict discussion and more positive cognitive appraisals (Hertz et al., 2015). HeartMath interventions have improved emotional regulation of stress in adolescents with ASD and attention-deficit/hyperactivity disorder (ADHD) (Aguinaga, 2006; McCraty et al., 1999).
To date, the research using parent-report or self-report measures indicates that mindfulness techniques can benefit youth with ASD. Few controlled studies exist with biometric outcome measures with adequate rigor (Hartley et al., 2019; Hourston & Achtley, 2017). No known study has measured mindfulness stress management with both HRV and cortisol response in adolescents with ASD. Nor is it clear how mindfulness interventions might compare to EAS in terms of HRV, perceived stress, and cortisol levels.
Rationale for Research Question
While some evidence exists about adolescents up to age 21 with THR (McDaniel-Peters & Wood, 2017) and mindfulness stress management training (Hourston & Achtley, 2017), questions linger about the relative effectiveness of these non-pharmacological interventions for individuals with autism. Not all adolescents have access to both THR and mindfulness sessions. Since there is limited time and resources, which intervention is more effective for the adolescent with autism? Several systematic reviews have suggested that there is large variability among individuals with autism (McDaniel-Peters & Wood, 2017; O’Haire, 2017) and suggest the importance of determining which people benefit from EAS and under what circumstances. One way this might be accomplished is through comparative effectiveness research (Arnold, 2015; McDaniel-Peters & Wood, 2017). O’Haire (2017) suggests the need for objective assessments to corroborate parent report which are prone to bias and the need for controls and/or comparisons. Others have suggested the need for manualized protocols that specify dose, activity sequence, and duration (McDaniel-Peters & Wood, 2017; Mesibov & Shea, 2011). This review also reported that only 9% of studies confirmed that research participants had diagnoses of ASD, indicating a need for more research with participants who have received a formal diagnosis (McDaniel-Peters & Wood, 2017). Similarly, with regard to mindfulness interventions for people with autism, several systematic reviews concluded there were too few controlled studies, lack of consistency in interventions across studies, too many small samples, and measures that relied on parent-report (Hartley et al., 2019; Hourston & Acchtley, 2017). Mazefsky et al. (2013) suggests a multi-faceted approach (e.g. subjective, behavioral, physiological) to understanding emotional regulation.
A few comparison studies do currently exist. The results of randomized control trials comparing THR to a barn no-horse control for children up to 16 years with ASD are promising for THR, indicating improvements in measures of irritability, social communication, social cognition, and hyperactivity (Gabriels et al., 2015; Pan et al., 2019). A prospective study found a reduction in severity of autism symptoms for children with ASD following THR treatment (Kern et al., 2011). In one comparative effectiveness study with individuals with ASD, Souza-Santos et al. (2018) found that THR and dance combined was more effective for ASD symptoms and functional independence than either intervention by itself. A similar comparative effectiveness study in people with ADHD found no difference between medications and EAS in terms of attention, impulsivity, and quality of life (Oh et al., 2018). Likewise, Hesselmark et al. (2014) compared group mindfulness to a generic group recreational activity, finding that group mindfulness was more effective in self-reports of quality of life and lack of dropout. No known studies compare THR to a mindfulness intervention and control for youth on the autism spectrum in order to better understand the effectiveness for managing stress levels. Although the two interventions may appear quite different, both involve a social component (interaction with other humans and/or animals). Both also involve a degree of awareness of the present; within the HM mindfulness protocol, this is facilitated. The THR intervention requires participants to direct and communicate with a large animal that is responsive to human feedback- this is likely to encourage participants’ attention to the present moment (Earles et al., 2015). The aim of this study is to compare the effectiveness of HM mindfulness techniques, THR, and no intervention control on stress and emotional regulation of adolescents with ASD as measured by self-report, parent-report, salivary cortisol, and heart rate variability.
Methods
Inclusion and Exclusion Criteria
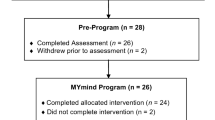
This study used a three-period randomized crossover design to compare a HM mindfulness protocol to a THR protocol to no treatment control for 27 young adults with ASD. The inclusion criteria were: (1) physician diagnosis of autism spectrum disorder, (2) ages 12–21 at the start of the study; (3) score above 59 on the Social Responsiveness Scale (SRS-2) (Constantino, 2012) which measures the severity of social function. The exclusion criteria were: (1) extreme fear or prior mistreatment of animals, (2) extreme anxiety to the point that the individual could not tolerate being in a group setting, and (3) taking corticosteroids or related medications. The crossover design allows for comparison of youth with ASD to themselves, rather than another group with ASD (Tse et al., 2018; Welleck & Blettner, 2012). Even when the two groups of people with ASD are randomized into an intervention and control, there is the likelihood of variability due to the wide variability on the autism spectrum (Wozniak et al., 2017). The research was approved by the local Institutional Review Board (IRB protocol # 027-71-C) for the protection of human subjects and the Institutional Animal Care and Use Committee (IACUC) for the protection of animals. Before beginning the research, both informed consent and assent were given by the subject and/or legal guardians.
Design
The research study had three separate 10-week periods. To avoid bias in order of testing, the order in which the individuals received each intervention was randomized. Interventions included THR, HM, or control, with a “wash out” period of at least 2 months between each 10-week period (Fig. 1). The researchers collected outcome measures and monitored the process, but separate certified individuals facilitated each intervention. To heighten treatment fidelity, the same THR and HM facilitators were used throughout the research study. Moreover, to control for the impact of the outdoor farm environment, the HM sessions were held in a building on the same property about 0.5 mile away from the equestrian center with the same view of woodlands and pastures as the THR group. However, the HM group could not see or interact with the horses.
Crossover study design protocol: baseline and follow-up cortisol samples were taken over two consecutive days at four time points (awakening, 30 min post-awakening, session time, and within 30 min of bedtime), pre/post cortisol samples were taken immediately before and after each individual THR or HM session, and coherence was recorded during each individual session
The outcome measures for stress level were: (1) salivary cortisol; (2) perceived stress from the perspective of the adolescent with ASD; and (3) parent report of social responsiveness. Emotional regulation (coherence) was measured through heart rate variability (HRV). As seen in Fig. 1, before (baseline) and after (follow-up) each 10-week period (THR, HM Mindfulness, or Control), salivary cortisol, self-report of perceived stress (Cohen et al., 1983), self-report of stress survey for persons with autism (Goodwin et al., 2007) and parent report of social responsiveness scale (SRS-2) (Constantino, 2012) were collected. During each of the 10 intervention sessions, salivary cortisol samples and HRV were collected.
Self-Report and Parent-Report
Three questionnaires were used before and after the 10-week periods and were collected six times. Self-reported perceived stress (Cohen et al., 1983), Cohen’s Perceived Stress Scale, has established validity and reliability and the 10-item tool measures the degree to which situations are appraised as stressful and to understand how unpredictable and uncontrollable individuals find their lives. Stress Survey Schedule for Persons with Autism and Other Developmental Disabilities (SSS; Groden et al., 2001) is a valid and reliable 49-item tool for discerning which areas are more or less stressful for individuals with autism (Goodwin et al., 2007). With adequate divergent validity and internal consistency (Woodard et al., 2021), the SSS contains 49 items specific to individuals on the autism spectrum (e.g. rate the intensity of stress reaction to waiting to talk about a desired topic). The scale variables focus on the intensity of stress related to “changes,” “positive events,” “anticipation,” “sensory,” “social,” “unpleasant events,” “food,” and “rituals.”
While parents are not able to reliably perceive the internal stress level of their youth, they can report on the frequency of observed socially-related behaviors. The Social Responsiveness Scale (SRS-2; Constantino, 2012), which collects data on 65 items on everyday behaviors reported on a four-point Likert scale from the parents, and has five treatment subscales awareness, cognitive, communication, motivation, and restrictive repetitive behaviors (RRB) and a total raw score which can be converted to a T-score. The scale has excellent psychometric properties (Constantino et al., 2003) and provides information on the presence and severity of social impairment within the autism spectrum.
Human Cortisol Sampling
During each day of an intervention (each of the 10 sessions), a pre-intervention (immediately before) and post-intervention (immediately after) saliva sample was collected from each subject. Baseline and follow-up, before and after each 10-week period, saliva samples were collected from home over two consecutive days at four time points per day to obtain cortisol values to characterize the diurnal rhythm of each participant. Baseline samples were collected over a Saturday and Sunday within 1 week of starting each of the three periods, and follow-up samples were collected over a Saturday and Sunday within one week of ending each of the three periods. For each of the two days, the sampling times were awakening, 30-min post-awakening, afternoon at time of intervention, and 30-min before bedtime, thus resulting in 8 home samples in total. Parents and participants were provided with specific instructions for sample collection and sampling restrictions, along with a check sheet to assist with keeping track of sampling times or note any issues. Samples were taken using the passive drool method by allowing saliva to pool in the mouth and allowing it to drain from the mouth to a collection tube. For participants who had difficulty with this method, samples were taken by holding a SalivaBio Children’s Swab Device (Salimetrics LLC, State College, PA) under the tongue for 60 s. Parents were asked to plan ahead so that participants did not eat a meal within 60 min prior to sampling or brush teeth within 30 min prior to sampling. Snacks or drinks (including water) were prohibited within 10 min prior to sampling times. During the intervention periods (HM or THR), saliva was also collected in the same manner immediately before (pre) and after (post) each 1-h intervention in the afternoon at the same times each day. The loss of sample from parent-collected saliva was 4%. All saliva samples were stored at − 20 °C until analysis.
Cortisol Assays
The salivary cortisol assay was completed using a competitive salivary cortisol enzyme-linked immunosorbent assay (ELISA) kit (Salimetrics LLC, State College, PA) validated for human saliva. Saliva samples were thawed and centrifuged at 1500× g for 15 min to separate the aqueous component from mucins and other suspended particles in the sample. Standards, a high positive control, a low positive control, a negative control, and samples were tested in duplicate on each plate following standard procedures outlined by the manufacturer (Salimetrics LLC, State College, PA). The plate was read at 450 nm with a secondary filter correction at 492 nm. A 4-parameter non-linear regression curve was determined for the standards on each plate (R2 ≥ 0.98).
Heart Rate Variability (HRV)
Using an individualized emWave Pro sensor clipped on the participant’s ear (HeartMath Institute, 2020), HRV of subjects was measured throughout each session, resulting in an average coherence level for the entire session. During the THR session, the device was placed in a light backpack so that the participant did not need to hold it. During the HM Mindfulness session, the participant held the small 3 inch × 2.5 inch device. At the end of each session, the sensor data was downloaded into the emWave Pro software system on a desktop computer. The coherence level identified by the emWave Pro is a measure of sine-wavelike signal with a very narrow, high-amplitude peak in the low frequency (LF) region of the HRV power spectrum with no major peaks in the very-low-frequency (VLF) or high-frequency (HF) regions, calculating a coherence ratio which reflects peak power/[total power—peak power] based on the integral in a window 0.030 Hz wide, centered on the highest peak in that region (HeartMath Institute, 2020). Heart rhythm data creates a complex set of frequencies all represented in the average. In high coherence, many of these influences quiet, and the heart and breath synchronize into one frequency resulting in one dominant peak clearly defined at the coherence frequency around 0.1 Hertz (HeartMath Institute, 2020).
Sample Characteristics
After recruitment, 30 participants, all of whom were diagnosed by their medical provider as having ASD or Pervasive Developmental Disorder, Not Otherwise Specified (PDD, NOS) provided assent and consent and began the study. Out of the original 30, 13% had a co-morbid diagnosis of depression and 10% had an official diagnosis of anxiety. Before the end of the study, three participants chose not to continue for various reasons. For the remaining 27 participants who completed the study, the mean and standard deviation of the t-score on the SRS-2 was x̄ = 73 ± 8.75, ranging from 61 to 90. The ages at the start of the study ranged from 12 to 21 years, x̄ = 16.33 ± 2.77 with 25.92% identifying as female and 74.07% identifying as male.
The proportion of female to male participants in the sample is only slightly higher (0.259) than the national average (0.247) for adults with ASD 18 and older (Dietz et al., 2020). A fairly even representation exists in the categories of male participants, ages 12–15 years (35%), 16–18 years (35%), and 19–21 years (30%) [Table 1]. However, when comparing females, more females were in the 16–18 years category (57.14%) versus 12–15 years (28.57%) and 19–21 years (14.28%). With regard to ethnicity, only 3.7% of the participants were non-Hispanic Black, and only 3.7% were Hispanic. Prior to inclusion in the study and throughout the trial, parents were asked to report medication lists for the participants. The study did not include any participants who were taking corticosteroids.
Therapeutic Riding Protocol
In all three periods, the same certified professional association of therapeutic horsemanship (PATH) instructor, who was also a certified therapeutic recreation specialist (CTRS), administered the THR protocol using a manualized program (Kemeny et al., 2019), which consisted of one-half hour of ground work (grooming, tacking, relationship building with horse) and one-half hour of riding consisting of warm-up, teaching a basic riding skill, review, and cool down [Table 2]. Each session progresses on the next to promote growth in the participants’ ability to exercise control, autonomy, and build relationship with the animal. If a participant needed to miss a session, a make-up session was offered at the same time during another day that week. The manual used for the study contained detailed step-by-step procedures for each of the parts of the session. Other aspects integrated into the procedures progressively were: (1) increase time on task; (2) follow a sequence of steps; ((3) increase emotional regulation in social setting (i.e. wait turn to get on horse); (4) initiate verbal interaction with horse or volunteer; and (5) express emotions regarding horse’s well-being. To promote consistency beyond the CTRS facilitator and manualized program, each participant had a 1:1 consistent volunteer who supported the individual participant’s needs in the program (i.e. leading horse during THR or supporting mindfulness walk during HM).
Modified HeartMath Mindfulness Protocol
For all three periods of 10 weeks, the same HM Intervention Specialist, who was a CTRS and HM Coach, administered the modified manualized HM mindfulness program [Table 3]. Each of the techniques builds upon the other to provide the participant the opportunity to gain self-regulation skills. The HM program (HeartMath Institute, 2015), a mindfulness protocol, typically offered in six sessions, was modified for use with people with autism spectrum disorder in a 10-session format. If a participant needed to miss a session, a make-up session was offered at the same time during another day that week. The modified curriculum was manualized with specific step-by-step procedures. The modifications included a slower pace to allow for repetition and processing time, highly structured sessions, reduced expectations for verbalizations (provide options to point to choose or manipulate objects), reduce the use of metaphors, use of hands-on activities, homework, and use of visuals (hand-outs and manipulatives). The participants did not sit in a circle in one place for the entire hour, but they had opportunities to stand up and move around as they desired. These modifications are similar to those used in other research with psycho-social outcomes (White et al., 2018).
Statistical Analyses
Baseline and follow-up were compared for each intervention and control for the computed scales of the self-report of stress survey schedule (SSS) for Autism (8 scales), Cohen’s Perceived Stress Scale (one total score scale), and the Parent-report SRS-2 (5 scales and 1 total score) using two-way repeated measures ANOVA. The dependent variable was self-reported stress or parent-reported social responsiveness and the within-subjects’ factors were treatment (THR, HM, and control), time (baseline and follow-up). Normality of the scale variables was checked using measures of skewness, kurtosis, box plots, and Q-Q plots and all variables had a normal distribution. Mauchly’s test of sphericity was evaluated and sphericity was assumed. When there was an interaction in the repeated measures ANOVA, separate one-way ANOVAs were conducted to confirm main effect. Paired sample t-tests were used to compare the baseline and follow-up for each phase (THR, HM, Control) for each scale.
The salivary cortisol ELISA intra-assay and inter-assay coefficients of variation were calculated using high and low controls. The intra-assay coefficient of variation was 3.8%, and the inter-assay coefficient of variation was 7.4%.
Baseline and follow-up cortisol concentrations were compared for each intervention and control at the four daily sampling times using three-way repeated measures ANOVA. The dependent variable was cortisol and the within-subjects factors were treatment (THR, HM, and control), time (baseline and follow-up), and diurnal sampling time (awakening, 30 min post-awakening, session time, and 30 min before bedtime). Normality of the studentized residuals was checked using the Shapiro–Wilk test, box plots, and Q-Q plots. A few outliers were removed from one of the two sampling days that were averaged for the follow-up samples at bedtime. Subsequently, the baseline and follow-up cortisol concentrations were transformed using a log10 transformation, and normality of residuals was rechecked using the Shapiro–Wilk test and histograms before the final ANOVA was performed. Mauchly’s test of sphericity was evaluated and the Greenhouse–Geisser values were used for data where sphericity could not be assumed. Main effects were compared using post-hoc tests with Bonferroni corrections.
Cortisol awakening response increase (CARi) for baseline and follow-up samples was calculated by using the mean values of the two consecutive collection days and subtracting the awakening values from the 30-min post-awakening values. Cortisol awakening response (CAR) was calculated by subtracting the awakening values from the 30-min post-awaking values, dividing by the awakening value, and multiplying by 100 to find the percent increase. Normality of residuals was checked using the Shapiro–Wilk test, and no transformations were made. The baseline CARi was be compared to the follow-up CARi for each intervention using two-way repeated measures ANOVA. The dependent variable was cortisol CARi and the within-subjects factors were treatment (THR, HM, and control) and time (baseline and follow-up).
Cortisol concentrations immediately before (pre) and after (post) the intervention sessions were also compared. Normality of the differences between the pre and post means were checked using the Shapiro–Wilk test. The data were not normally distributed, so the Wilcoxon signed-rank test was used to compare overall median session cortisol concentrations for THR and HM, as well as median cortisol concentrations for individual sessions 1–10 during the 10-week periods. Median pre and post-session cortisol concentrations were also compared with control baseline. The differences between overall pre and post cortisol concentration medians (pre-post) were also compared between treatments by Wilcoxon signed-rank test.
Dependent t-tests were used to compare coherence levels (heart-rate variability) for HM and THR, both for the overall mean and the means for each session.
Results
Self-Report Measures of Stress
The comparison of the participant’s self-report scales (SSS scales or self-perception total score) from baseline to follow-up suggest that no significant change in stress occurred in THR phase, but the HM phase showed increased perception of stress in social (p = 0.029) and unpleasant events (p = 0.001). There was also an increased perception of stress in the food scale (p = 0.024) during the control phase [Table 4]. The two-way repeated measures ANOVA indicates an interaction between intervention (THR, HM, Control) and time (F = 4.007) and p = 0.027 for perceived stress of unpleasant events [Table 5]. Mean perceived stress of unpleasant events was statistically different over time in the HM phase (F = 16.461, p = 0.001) indicating a main effect, but not statistically different over time in the THR (F = 0.805, p = 0.379) or control phase (F = 0.584, p = 0.453). Perceived stress of unpleasant events was not statistically different when comparing baseline values (THR, HM, or Control) F = 2.974, p = 0.065 nor when comparing follow-up values (THR, HM, Control) F = 1.220, p = 0.308.
When comparing the participants’ self-report of stress focusing on individual items from baseline to follow-up for the THR, HM, and control phases, some comparisons indicated that the THR phase was more effective in reducing self-reported stress [Table 6]. The THR phase showed significant improvement in stress level when compared to HM phase when receiving a reprimand (p = 0.012), receiving criticism (p = 0.022), having something marked incorrectly (p = 0.044), being unable to communicate needs (p = 0.038), being able to assert oneself (p = 0.027), participating in a group activity (p = 0.039), waiting for reinforcement (p = 0.039), and waiting for routine to begin (p = 0.025). The TR phase was more effective than the control phase in the perception of stress with participating in a group activity (p = 0.012), and having a change in staff, teacher, supervisor (p = 0.023). HeartMath Mindfulness was significantly more effective than control in terms of being prevented, following a diet (p = 0.029) and more effective than THR in terms of being prevented from carrying out a ritual (p = 0.042). Control was significantly better than THR with being prevented from carrying out a ritual (p = 0.008) and significantly better than HM in receiving a reprimand (p = 0.036).
Parent Report of Social Responsiveness Scale
The comparison of the parent-report scales compared from baseline to follow-up suggest that no significant change occurred in any phase (THR, HM, Control) [Table 7]. The two-way repeated measures ANOVA also indicates no significant difference between THR, HM, and Control phases for parent-reported scales (Awareness, Cognitive, Communication, Motivation, RRS, and Total Score) of SRS-2 [Table 8]. Analysis of the specific items of the parent-report of SRS-2 provide some additional information. The parent report of the SRS-2 showed mixed results when comparing baseline to follow-up (before and after the 10-week phase) from the different phases [Table 9]. In the control phase, there was a significant increase in “more fidgety in social situations” (x̄ baseline = 1.04, x̄ follow-up = 1.48, p = 0.009), a decrease in “difficulty relating to peers” (x̄ baseline = 1.84, x̄ follow-up = 1.52, p = 0.029), and a decrease in “doesn’t understand cause and effect” (x̄ baseline = n 1.64, x̄ follow-up = 1.24, p = 0.047). In the HM phase, there was a significant decrease in “behave in ways that are strange or bizarre” (x̄ baseline = 1.47, x̄ follow-up = 1.20, p = 0.041), decrease in “difficult in change in routine” (x̄ baseline = 2.07, x̄ follow-up = 1.47, p = 0.023), and decrease in “wandering aimlessly from one activity to another” (x̄ baseline = 1.13, x̄ follow-up = 0.533, p = 0.014). In the THR phase, participants significantly improved ability to, “recognize when something is unfair” (x̄ baseline = 1.96, x̄ follow-up = 1.56, p = 0.016), decreased “avoidance of starting social interactions” (x̄ baseline = 1.39, x̄ follow-up = 0.956, p = 0.038), “difficulty relating to peers” (x̄ baseline = 2.00, x̄ follow-up = 1.48, p = 0.011), “walking between two people who are talking” (x̄ baseline = 1.48, x̄ follow-up = 1.17, p = 0.031), but increased “too tense in social settings” (μ baseline = 1.14, x̄ follow-up = 1.50, p = . 017).
Comparison of Salivary Cortisol Levels at Baseline and Follow-up
Descriptive statistics show a diurnal rhythm of higher salivary cortisol concentrations observed in the morning, and lower salivary cortisol concentrations observed in the afternoon and evening [Table 10]. For the control phase, descriptive statistics revealed that cortisol levels increased from awakening (x̄ baseline = 0.347 µg/dL, x̄ follow-up = 0.346 µg/dL) to 30 min post awakening (x̄ baseline = 0.380 µg/dL, x̄ follow-up = 0.488 µg/dL), indicating a CAR of 9.5% and 41% at baseline and follow-up, respectively. There was a decrease in salivary cortisol concentration at session time (x̄ baseline = 0.178 µg/dL, x̄ follow-up = 0.171 µg/dL) and further decrease at bedtime (x̄ baseline = 0.100 µg/dL, x̄ follow-up = 0.095 µg/dL). Salivary cortisol results for the THR phase were numerically lower at follow-up than baseline at all four time points: awakening, (x̄ baseline = 0.402 µg/dL, x̄ follow-up = 0.298 µg/dL), 30 min post-awakening (x̄ baseline = 0.395 µg/dL, x̄ follow-up = 0.295 µg/dL), session time (x̄ baseline = 0.154 µg/dL, x̄ follow-up = 0.144 µg/dL), and bedtime (x̄ baseline = 0.122 µg/dL, x̄ follow-up = 0.114 µg/dL), and showed a decrease at each time point throughout the day. This led to a CAR of -1.7% (baseline) and -1% (follow-up). For the HM phase, awakening results were numerically lower at follow-up compared to baseline (x̄ baseline = 0.470 µg/dL, x̄ follow-up = 0.361 µg/dL). There was a lack of CAR at baseline (-13.4%) but an increase at follow-up (24.9%), with 30-min post-awakening results of x̄ baseline = 0.407 µg/dL and x̄ follow-up = 0.451 µg/dL. Cortisol concentrations decreased at session time (x̄ baseline = 0.157 µg/dL, x̄ follow-up = 0.156 µg/dL) and bedtime (x̄ baseline = 0.118 µg/dL, x̄ follow-up = 0.113 µg/dL).
The three-way repeated measures ANOVA for the log10 transformed salivary cortisol data did not identify a statistically significant three-way interaction between diurnal sampling time, baseline versus follow-up, and treatment, or any significant two-way interactions between any of the variables [Table 11]. Diurnal sampling time of day was statistically significant as a main effect and had a large effect size on log10 transformed salivary cortisol concentration [F(3, 57) = 78, p < 0.001, ηp2 = 0.80]. Post-hoc tests indicated no statistical difference between awakening and 30-min post-awakening samples, but all other sampling time of day comparisons were statistically significant (p < 0.001). There was a trend for treatment as a main effect with medium effect size on log10 transformed salivary cortisol concentration [F(1.4, 27) = 2.8, p = 0.093, ηp2 = 0.129]. Post-hoc tests showed a trend for a difference between THR and HM (p = 0.076), but no differences between either treatment and control. The two-way repeated measures ANOVA for the CARi identified a statistically significant result for the main effect of baseline versus follow up with large effect size (F(1, 19) = 4.4, p = 0.049, ηp2 = 0.189), with higher follow-up CARi values compared to baseline [Table 11]. There was no effect of treatment or treatment × baseline versus follow up.
Comparison of Therapeutic Riding and Mindfulness during Sessions
Coherence
A comparison of the overall mean coherence values showed that HM mindfulness yielded a significant improvement in coherence levels when compared to THR [Table 12]. Moreover, when individual sessions were compared, the mean of all participants’ coherence values during sessions 2, 5, 7, 8, 9, and 10 was significantly higher for HM than THR.
Cortisol
A comparison of the median pre and post cortisol concentrations during the 10 sessions of HM and THR phases revealed significant decreases in cortisol levels following both HM and THR interventions [Table 13]. When analyzing each session separately, more THR sessions (10 sessions) resulted in a significant decrease in cortisol than HM sessions (7 sessions); however, there was no statistically significant difference when comparing the overall session cortisol concentration decreases (pre-post) between the two treatments. The overall (all 10 sessions combined) comparisons for pre-session versus post-session were statistically significant for both THR and HM. There was no statistically significant difference between treatments when comparing overall (10 sessions combined) HM pre-session cortisol concentration medians with THR pre-session medians, or comparing overall THR and HM post-session cortisol concentration medians. There was no statistically significant difference when comparing control baseline median (0.154 µg/dL) with THR pre-session cortisol concentration median (0.143 µg/dL), but THR post-session cortisol concentration median (0.093 µg/dL) was significantly lower than the control baseline median (z = − 1.96, p = 0.049). There was a statistically significant difference when comparing HM pre-session median cortisol concentration (0.129 µg/dL) with control baseline (z = − 2.54, p = 0.011) or HM post-session median cortisol concentration (0.092 µg/dL) with control baseline (z = − 4.02, p < 0.001).
Discussion
Self-Report of Stress
No significant changes were seen in Cohen’s general PSS total score over any phase, but participants showed a significant increase in perceived stress with respect to unpleasant events during the HM intervention when compared to the THR intervention or control. T-test comparisons suggested increased perceived stress in the social and unpleasant categories for the HM phase and food for the control phase. When focusing only on descriptives for the scale variables, with the exception of “stress about positive events,” THR intervention showed a decrease in the mean values for perceived stress while HM showed an increase in self-perceived stress in all areas except PSS total. During the control phase, participants increased their stress level for all scales except anticipation, sensory, social and the PSS total. One difference in the THR, HM, and Control periods is that the HM period sessions focused on the topic of stress, stress triggers, and specific goal-oriented education on learning to self-regulate [Table 3]. There is a possibility that overt awareness and identification of stressors during the HM sessions may have increased self-perceived stress in the area of social and unpleasant events at follow-up after the sessions. Mazefsky & White, (2014) in their research on emotional regulation and ASD indicate that individuals with ASD often lack the motivational component integral to on-going emotional regulation. Moreover, cognitive factors (e.g. deficits in problem-solving, rigidity, and lack of perspective-taking promote further difficulties in emotional regulation (Mazefsky & White, 2014). Perhaps, during the facilitation of the HM mindfulness session, the participant can be guided to better coherence, but at the end of the HM phase, they have more awareness about stress, but less ability to practice stress-reduction on their own. Individuals need both awareness and coping self-efficacy (Oswald et al., 2018). The participants experienced physiological stress-reduction during HM sessions (cortisol levels drop and coherence rises), but they need continued support and facilitation to experience stress-reduction on their own.
On the other hand, with THR, the stress-reduction mechanism is less an education process and more experiential. O’Haire (2017) reports that a high frequency of positive outcomes from AAI related to social interaction, verbal language, and positive emotions. The THR sessions allowed for more natural social interaction and touching the horses rather than only interacting with people. Moreover, Wijker et al., (2019, 2020) suggested that touching the animal promoted stress reduction. The emphasis in the sessions was interacting, grooming, and directing the horse, and practicing emotional regulation in a natural setting (i.e. waiting for other participants to mount) rather than cognitively examining stress triggers or actively working at stress reduction. In other words, the time with the horse creates a positive focus of attention (Fine & Beck, 2015) to interact with an accepting animal with little “fear of negative evaluation” that accompanies peer social interaction (Capriola et al., 2017). Other research supports that caring for the horse through grooming and interacting promotes self-efficacy and a sense of control (Goodwin et al., 2016).
Parent-Report of Social Responsiveness
While no significant difference exists in the comparison of SRS-2 baseline to follow-up for THR, HM, and Control or comparison of the three phases on parent-report of SRS, a discussion on the individual items of the scale provides some further information. O’Haire (2017) suggested that the core of the SRS focuses on internalizing and externalizing behaviors, but her review found these behaviors are not typically impacted by AAI. Parents reported a substantial increase in fidgetiness in the control phase, but a slight decrease in difficulty relating to peers and not understanding cause and effect. Pan et al. (2019) found a decrease in hyperactivity and irritability with therapeutic riding but not control. In this study, fidgetiness actually increased during the control phase with an absence of any intervention. By anecdotal report, both participants and parents positively anticipated participating in either intervention. It is possible that the parents noticed more restlessness when the child had a lack of intervention during the control phase. In the HM phase, parents reported decreases in anti-social behaviors such as behaving strangely, difficulty with changes in routine, and wandering aimlessly between activities. This parent report fits the salivary cortisol and coherence findings, but does not correspond to the self-report findings about HM and self-perceived stress of unpleasant events (if these are considered unpleasant events for the person with autism). The HM session did include a booklet which the participants brought home. In some cases, the parents may perceive that the adolescent was calmer over the HM phase as they were asked to comment on behaviors over a wide span of time, but the self-report was an indication of how the adolescent felt in the moment of filling it out.
In the THR phase, there was an improvement in a prosocial behavior and recognizing unfairness, and a decrease in anti-social behaviors such as avoidance of initiating social interactions, difficulty relating to peers, and walking between two people who are talking. The parent report of improvements in recognizing unfairness and decreases in anti-social behaviors correspond with decrease in salivary cortisol with THR as does the participants’ self-report of positive improvements in their response to participating in a group and having to wait. Gabriels et al. (2015), also used the SRS and found improvements in communication and cognition, but no change in motivation or awareness with equine-assisted activity. Parent perception of AAI captured by other research has reported the presence of animals improved motivation, engagement, communication, and community participation (London et al., 2020). One discrepancy with the self-report and salivary cortisol findings was the parent report of an increase in the participant being tense in social settings after the THR phase. While “being tense” should have some relationship to self-reported stress, coherence, and salivary cortisol, it is important to recognize that the follow-up is completed after the phase and may not reflect how the participant is reacting on a session day to THR. Perhaps, certain aspects such as a stress in a group is defined or perceived differently by the parent and the adolescent participant. The participant would be determining stress levels from internal levels, where the parent would be using observation to determine if their child is “being tense.” There is an advantage to viewing the results from multiple perspectives: the parents, the adolescent themself, and biometric measures. However, differences in perception may impact the self-report and parent-report measures. Van der Steen et al. (2019) compared outcome measures of one child with therapeutic riding and found differences between outcome measures on the same child with autism. On the other hand, Ozsivadjian et al. (2014) found agreement between self-report and parent-report in youth with autism on the areas of anxiety, depression, and negative thoughts.
Salivary Cortisol
Participant salivary cortisol was higher in the morning and decreased throughout the day, with the lowest values just before bedtime. However, there was some variability between the salivary cortisol concentrations, even within the control phase. Corbett et al. (2008) found that, compared with a group of children without ASD, children with ASD had higher between and within subject variability in diurnal cortisol values, as well as higher values at night, which was hypothesized to possibly correspond to stressful events of the day. Our mean bedtime cortisol concentrations were all lower than the afternoon session time cortisol concentrations for baseline and follow-up, and most of our variability was seen in the morning samples. As this was a crossover study, any variability in our findings was within subjects. Brosnan et al. (2009) found that adolescent males diagnosed with Asperger syndrome showed a diurnal decrease in cortisol throughout the day, but lacked a significant CAR, while the control group of participants without Asperger syndrome displayed a consistent and significant CAR, as well as a diurnal decrease in cortisol throughout the day. We found that participants lacked a CAR at baseline for THR and HM. Participants displayed a CAR at follow-up of HM and control, but lacked a CAR at follow-up of THR. Another study where children with ASD were placed with a service dog found the CAR to decrease from 58 to 10% following the addition of the service dog, and then increase again to 48% once the service dog was removed (Viau et al., 2010). The authors of that study hypothesized that better quality of sleep due to the presence of the service dogs may have led to the decrease in CAR. There could have been a “de-arousing effect” due to the presence of the animal (Berry et al., 2013). A meta-analysis of studies evaluating CARi found increased CARi to be associated with general life stress and job stress, and decreased CARi to be associated with positive psychological traits, as well as fatigue and exhaustion (Chida & Steptoe, 2009). The participant self-reports denoted decreased stress level for the THR phase and would support the CARi decrease being associated with lesser stress. Another study found that children who participated in cardiovascular exercise displayed increased CARi, whereas children in the motor exercise group displayed decreased CARi (Wegner et al., 2019). A meta-analysis found lower basal cortisol to be associated with increased physical activity or physical fitness (Mücke et al., 2018). Physical fitness was not evaluated in this study and the participants underwent low intensity exercise in the TR phase, but perhaps higher intensity riding exercises or more frequent lessons could lead to statistically significant differences in future study.
When comparing individual sessions, there was a significant decrease in salivary cortisol concentration after the intervention in all of the THR sessions and seven of the HM sessions, and the overall post-session median cortisol concentration was significantly decreased from pre-session for both treatments, indicating that salivary cortisol was reduced through both interventions. Similarly, in a pilot study of children with ASD, Pan et al. (2019) found that salivary cortisol concentrations decreased following THR lessons; however, in that study there was no difference from the control group practicing unmounted activities in the barn using a stuffed horse. Barker et al. (2010) found that 30-min interaction with an unfamiliar dog or the participant’s own dog was found to be associated with decreases in salivary cortisol, blood pressure, and heart rate below no-dog baseline measures following exposure to a stressor. In our study, when comparing control baseline cortisol concentration to post-session cortisol concentrations, post-THR session and post-HM session cortisol concentrations were significantly lower than control baseline samples taken at the same time of day, further supporting that both interventions were effective in reducing salivary cortisol concentrations. We found no difference when comparing overall session cortisol concentrations between the two treatments (but both had statistically significant decreases in salivary cortisol from pre-post session), indicating that both interventions could be equally useful for stress management for adolescents with ASD.
Coherence
The coherence results for the sessions point to a higher coherence in the HM sessions when compared to the THR sessions. Although THR involved low-intensity riding skills, changes during the activity, such as going from walk to trot, could alter HRV. On the other hand, some of the difference may be related to the protocol for collecting the heart-rate variability values. While on horseback, so that they could hold the reins, the participants wore the device in a light backpack on their backs. During the mindfulness sessions, the participants held their devices and could see the values on the devices. In this case, the devices may have been reinforcing more even breathing and calmer responses as the participants saw an immediate result of their practice. By nature of the intent of each session, HM is more focused on self-management of stress. In the THR sessions, the participant was not being focused on self-management of stress; the participant was focusing on the content of the therapeutic riding session.
The study’s applicability may have been improved by the fact that it measured interventions in a natural rural setting. Each facilitator of the interventions had the same educational discipline-specific recreational therapy training with specific certificates in either HeartMath or therapeutic riding, providing a consistency of approaches (rather than comparing a social worker or psychologist facilitated group to a recreational therapist conducting therapeutic riding). Moreover, a strength of the design allowed for each person to complete each intervention and control phase, comparing within the subjects, rather than using data from three different randomly selected groups. The design triangulated different perspectives (participant self-report, parent-report, and biometric measures) to gain an in-depth picture of the response to interventions.
Limitations
The two interventions, THR and HM, have not been compared in prior research. While they both are used in practice to reduce stress, one focuses completely on facilitator/peer social interaction and the other focuses on animal interaction with some facilitator interaction. Both interventions did allow the participants to move around gently (with no strenuous aerobic exercise in either intervention). However, there is certainly more movement and vestibular-cerebellar stimulation in THR related to the movement of the horse (Arnold, 2015). Although they were not the only measures used in the study, self-report and parent-report have inherent limitations as the results may be influenced by response bias (e.g. not understanding, misreading, rushing, or social desirability) (Rosenman et al., 2011). Moreover, this study did not compare the participants in their response to THR and HM based upon verbal skills, adaptive functioning, behavioral level, anxiety level or sleep patterns. The sample was too small to compare the response to interventions based on gender, race, or ethnicity. While this study did not measure anxiety level, self-reported stress and cortisol levels are related constructs. Furthermore, not enough is known about the variability of anxiety among people with autism (Kerns et al., 2014) and how individuals respond to non-pharmacological interventions. Research on autism and anxiety disorders has raised concerns about a one-size fits all approach (Herrington et al., 2017; South et al., 2017).
Future Research
Future research on larger samples could compare individuals on the spectrum’s response to various interventions based on severity of autism and level of verbal skills. Future research may focus on stress in autistic adolescents/young adults with comorbid intellectual disability. Moreover, it may be important to investigate gender differences of people with autism in response to stress management and therapeutic riding interventions (McVey et al., 2017; Pisula et al., 2017).
For example, HeartMath mindfulness sessions, with the dependence on receptive comprehension and self-management, may not be an appropriate approach for adolescents who are lower functioning in terms of their receptive or expressive communication ability or high level of anxiety in groups. Therapeutic riding does not require the same extent of interpersonal communication as the HeartMath; although participants may be asked to verbally communicate with the instructor, peers, volunteers, or the horse, there is a greater emphasis on non-verbal communication with the horse. Because of the greater response of the horse to touch versus verbal cues (Arnold, 2015), THR may be a better approach for stress reduction for participants with lower verbal skills. Therapeutic riding may also be more motivating for some individuals than others. It would also be interesting to evaluate the effectiveness of THR programming that intentionally incorporates mindfulness activities and evaluates mindfulness as an outcome. Earles et al. (2015) found that a program of unmounted equine activities using the Equine Partnering Naturally© program led to significantly increased mindfulness scores for individuals with PTSD. Combining riding and mindfulness activities could be beneficial and motivating for some participants and warrants future study.
Conclusion
This study contributes to the literature by using a manualized pre-tested procedure, facilitated by professionals with consistent discipline and specialization certification in the intervention. Moreover, a randomized crossover design, by comparing the individual to themselves over time, avoids the inherent issues with heterogeneity in the population of adolescents with autism. This comparison of manualized interventions has a multifaceted data collection methodology which has the potential to be useful to parents, transition specialists, and therapists as they support the individual youth with autism in decision-making among alternate approaches.
The 10-week HM mindfulness and therapeutic riding manualized protocols were equally beneficial in decreasing cortisol levels immediately following a session. Participants showed a higher CARi following the control and HM phases, and a lower CARi following the THR phase. Participants report of perceived stress of unpleasant events after the HM phase when compared to control and THR may be related to increase in awareness of stressors without having independence in coping self-efficacy to handle on-going stress. The impact of the interventions both decreased stress, as evidenced by salivary cortisol and coherence, during the facilitated session. Both interventions, with the manualized protocol, could be considered in the non-pharmacological options for interventions. Therapeutic riding may be an intervention that will be effective despite verbal communication ability, while HeartMath may be more effective for adolescents/young adults with better receptive and expressive verbal skills. In the time of COVID-19, it is easier to practice physical distancing from others with therapeutic riding, but HeartMath would be more easily delivered via telehealth mechanisms. For adolescents with ASD, screening for level of cognition and communication ability may determine which protocol should be used for the particular client needing stress reduction.
References
Abihsira, N., Brown, E., & Breslin, C. F. (2020). Therapeutic horseback riding and social independence in children with autism spectrum disorder. Therapeutic Recreation, 14, 84–95.
Aguinaga, N. (2006). An investigation of the effectiveness of computer-assisted biofeedback for students diagnosed as having autism spectrum disorder. Electronic Theses and Dissertations, 2004–2019, 951.Retrieved from https://stars.library.ucf.edu/etd/951
Ajzenman, H. F., Standeven, J. W., & Shurtleff, T. L. (2013). Effect of hippotherapy on motor control, adaptive behaviors, and participation in children with autism spectrum disorder. The American Journal of Occupational Therapy, 67(6), 653–663.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596
Anderson, S., & Meints, K. (2016). The effects of equine-assisted activities on the social functioning in children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(10), 3344–3352.
Arnold, L. E. (2015). The alone rangers and silver. Journal of the American Academy of Child & Adolescent Psychiatry, 54(7), 535–536.
Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., Warren, Z., Kurzius-Spencer, M., Zahorodny, W., Rosenberg, C. R., White, T., Durkin, M. S., Imm, P., Nikolaou, L., Yeargin-Allsopp, M., Lee, L. C., Harrington, R., Lopez, M., Fitzgerald, R. T., Hewitt, A., … Dowling, N. F. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 Sites, United States, 2014. Surveillance Summaries, 67(6), 1–23.
Baker, E. K., Richdale, A. L., & Hazi, A. (2019). Employment status is related to sleep problems in adults with autism spectrum disorder and no comorbid intellectual impairment. Autism, 23(2), 531–536.
Barker, S. B., Knisley, J. S., McCain, N. L., Schubert, C. M., & Pandurangi, A. K. (2010). Exploratory study of stress buffering response patterns from interaction with a therapy dog. Anthrozoos., 23, 79–91.
Bass, M. M., Duchowny, C. A., & Llabre, M. M. (2009). The effect of therapeutic horseback riding on social functioning in children with autism. Journal of Autism and Developmental Disorders, 39(9), 1261–1267.
Bemmer, E. R., Boulton, K. A., Thomas, E. E., Larke, B., Lah, S., Hickie, I. B., & Guastella, A. J. (2021). Modified CBT for social anxiety and social functioning for young adults with autism spectrum disorder. Molecular Autism, 12, 11.
Benevides, T. W., & Lane, S. J. (2013). A review of cardiac autonomic measures: Consideration for examination of physiological response in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(2), 560–575.
Bennett, A. N., Miller, J. S., Stollon, N., Raghuram, P., & Blum, N. J. (2018). Autism spectrum disorder and transition-aged youth. Current Psychiatry Reports. https://doi.org/10.1007/s11920-018-0967-y
Berry, A., Borgi, M., Francia, N., Alleva, E., & Cirulli, F. (2013). Use of assistance and therapy dogs for children with autism spectrum disorders: A critical review of the current evidence. Journal of Alternative and Complementary Medicine, 19(2), 73–80.
Bishop-Fitzpatrick, L., Minshew, N., Mazefsky, C. A., & Eack, S. M. (2017). Perception of life as stressful, not biological response to stress is associated with greater social disability in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(1), 1–16.
Bitsika, V., & Sharpley, C. F. (2015). Differences in the prevalence, severity and symptom profiles of depression in boys and adolescents with an autism spectrum disorder versus normally developing controls. International Journal of Disability, Development and Education, 62(2), 158–167.
Bitsika, V., Sharpley, C. F., Andronicos, N. M., & Agnew, L. L. (2017). What worries parents of a child with autism? Evidence from a biomarker for chronic stress. Research in Developmental Disabilities, 62, 209–217.
Brosnan, M., Turner-Cobb, J., Munro-Naan, Z., & Jessop, D. (2009). Absence of a normal cortisol awakening response (CAR) in adolescent males with Asperger syndrome (AS). Psychoneuroendocrinology, 34, 1095–1100.
Cachia, R. L., Anderson, A., & Moore, D. W. (2016). Mindfulness in individuals with autism spectrum disorder: A systematic review and narrative analysis. Journal of Autism and Developmental Disorders, 3(2), 165–178.
Capriola, N. A., Maddox, B. B., & White, S. (2017). No offense intended: Fear of negative evaluation in adolescents and adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(12), 3803–3813.
Chida, Y., & Steptoe, A. (2009). Cortisol awakening response and psychosocial factors: A systematic review and meta-analysis. Biological Psychology, 80, 265–278.
Cohen, S., Kamarack, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(3), 385–396.
Conner, C. M., & White, S. W. (2018). Brief report: Feasibility and preliminary efficacy of individual mindfulness therapy for adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(1), 390–400.
Conner, C. M., White, S. W., Beck, K. B., Golt, J., Smith, I. C., & Mazefsky, C. A. (2019). Improving emotion regulation ability in autism: The emotional awareness and skills enhancement (EASE) program. Autism, 23(5), 1273–1287.
Constantino, J. N. (2012). (SRS-2) Social responsiveness scale (2nd ed.). WPS.
Constantino, J. N., Davis, S. A., Todd, R. D., Schindler, M. K., Gross, M. M., Brophy, S. L., Metzger, L. M., Shoushtari, C. S., Splinter, R., & Reich, W. (2003). Validation of a brief quantitative measure of autistic traits: Comparison of the social responsiveness scale with the autism diagnostic interview-revised. Journal of Autism Developmental Disorders, 33(4), 427–433.
Corbett, B. A., Mendoza, S., Wegelin, J. A., Carmean, V., & Levean, S. (2008). Variable cortisol rhythms in children with autism and anticipatory stress. Journal of Psychiatry Neuroscience, 33(3), 227–234.
Corbett, B. A., Muscatello, R. A., & Baldinger, C. (2019). Comparing stress and arousal systems in response to different social contexts in children with ASD. Biological Psychology, 140, 119–130.
Corbett, B. A., & Simon, D. (2014). Adolescence, stress, and cortisol in Autism Spectrum Disorders. Open Access Autism, 1(1), 2.
Deci, E. L., & Ryan, R. M. (2012). Motivation, personality, and development within embedded social contexts: An overview of self-determination theory. In R. Ryan (Ed.), The Oxford handbook of human motivation (pp. 85–107). Oxford University Press.
Dickerson, S. S. & Kemeny, M. E. (2004). Acute stressors and corticol responses: A theoretical integration and synthesis of laboratory research. Psychology Bulletin, 130(3), 355–391.
Dietz, P. M., Rose, C. E., McArthur, D., & Maenner, M. (2020). National and state estimates of adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(12), 4258–4266.
Dunlop, K., & Tsantefski, M. (2017). A space of safety: Children’s experience of equine-assisted group therapy. Child and Family Social Work, 23(1), 16–24. https://doi.org/10.1111/cfs.12378
Earles, J. L., Vernon, L. L., & Yetz, J. P. (2015). Equine-assisted therapy for anxiety and posttraumatic stress symptoms. Journal of Traumatic Stress, 28, 149–152.
Edmiston, E. K., Blain, S. D., & Corbett, B. (2017). Salivary Cortisol and behavioral response to social evaluative threat in adolescents with autism spectrum disorder. Autism Research, 10(2), 346–358.
Fine, A. H., & Beck, A. M. (2015). Understanding our kinship with animals: Input for health care professionals interested in the human-animal bond. In A. H. Fine (Ed.), Handbook on animal-assisted therapy: Foundations and guidelines for animal-assisted interventions (4th ed., pp. 3–10). San Diego, CA: Elsevier Inc.
Fjorback, L. O., Arendt, M., Ornbol, E., Fink, P., & Walach, H. (2011). Mindfulness-based stress reduction and mindfulness-based cognitive therapy: A systematic review of randomized controlled trials. Acta Psychiatry Scandinavia, 124, 102–119.
Fung, L. K. (2016). Cortisol in individuals with autism spectrum disorders: Meta-analysis and systematic review. Journal of the American Academy of Child & Adolescent Psychiatry, 55(10), 105.
Gabriels, R. L., Agnew, J. A., Holt, K. D., Shoffner, A., Pan, Z., Ruzzano, S., Clayton, G. H., & Mesibov, G. (2012). Pilot study measuring the effects of therapeutic horseback riding on school-age children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders, 6(2), 578–588.
Gabriels, R. L., Pan, Z., Dechant, B., Agnew, J. A., Brim, N., & Mesibov, G. (2015). Randomized controlled trial of therapeutic horseback riding in children and adolescents with autism spectrum disorder. Journal of American Academy of Child Adolescent Psychiatry, 54(7), 541–549.
Geisler, F. C., Kubiak, T., Siewert, K., & Weber, H. (2013). Cardiac vagal tone is associated with social engagement and self-regulation. Biological Psychology, 93, 279–286.
Geisler, F., Vennewald, N., Kubiak, T., & Weber, H. (2010). The impact of heart rate variability on subjective well-being is mediated by emotion regulation. Personality Individual Difference, 4(9), 723–728.
Goldman, S. E., Alder, M. L., Burgess, H. J., Corbett, B. A., Hundley, R., Wofford, D., Fawkes, D. B., Wang, L., Laudenslager, M. L., & Malow, B. A. (2017). Characterizing sleep in adolescents and adults with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 47(6), 1682–1695.
Goodwin, B. J., Hawkins, B. L., Townsend, J. A., Van Puymbroeck, M., & Lewis, S. (2016). Therapeutic riding and children with autism spectrum disorder: An application of the theory of self-efficacy. American Journal of Recreation Therapy, 15(4), 41–47.
Goodwin, M. S., Groden, J., Velicer, W. F., & Diller, A. (2007). Validating the stress survey for persons with autism and other developmental disabilities. Focus on Autism and Other Developmental Disabilities, 22, 183.
Gordis, E. B., Granger, D. A., Susman, E. J., & Trickett, P. K. (2006). Asymmetry between salivary cortisol and amylase reactivity to stress: Relation to aggressive behavior in adolescents. Psychoneuroendocrynology, 31(8), 976–987.
Groden, J., Diller, A., Bausman, M., Velicer, W., Norman, G., & Cautela, J. (2001). The development of a stress survey schedule for persons with autism and other developmental disabilities. Journal of Autism and Developmental Disorders, 31, 207–217.
Gu, J., Strauss, C., Bond, R., & Cavanaugh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-stress reduction improve mental health and well-being? A systematic review and meta-analysis of meditation studies. Clinical Psychology Review, 37, 1–12.
Harris, A., & Williams, J. M. (2017). The impact of horse riding intervention on the social functioning of children with autism spectrum disorder. International Journal of Environmental Research and Public Health, 14(7), 776.
Hartley, M., Dorstyn, D., & Due, C. (2019). Mindfulness for children and adults with autism spectrum disorder and their caregivers: A meta-analysis. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-019-04145-3
HeartMath Institute. (2015). HeartMath coach facilitator guide. HeartMath Institute: Boulder, CO.
HeartMath Institute. (2020). EmWave Pro specifications. Retrieved at https://heartcloud.com/library/asmts-hrv.html
Hebron, J., & Humphrey, N. (2014). Mental health difficulties among young people on the autistic spectrum in mainstream secondary schools: A comparative study. Journal of Research in Special Education Needs, 14(1), 22–32.
Herman, J. P., & Cullinan, W. E. (1997). Neurocircuitry of stress: Central control of the hypothalamo-pituitaryadrenocortical axis. Trends in Neuroscience, 20(2), 78–84.
Herrington, J. D., Maddox, B. B., McVey, A. J., Franklin, M. E., Yerys, B. E., Miller, J. S., & Schultz, R. T. (2017). Negative valence in autism spectrum disorder: The relationship between amygdala activity, selective attention, and co-occurring anxiety. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. https://doi.org/10.1016/j.bpsc.2017.03.009
Hertz, R. M., Laurent, H. K., & Laurent, S. M. (2015). Attachment mediates effects of trait mindfulness on stress responses to conflict. Mindfulness, 6(3), 483–489.
Hesselmark, E., Plenty, S., & Bejerot, S. (2014). Group cognitive behavioral therapy and group recreational activity for adults with autism spectrum disorders: A preliminary randomized control trial. Autism, 18(6), 672–683.
Hill, J., Zivani, J., Driscoll, C., Teoh, J. L., Chua, J. M., & Cawdell-Smith, J. (2020). Canine assisted occupational therapy for children on the autism spectrum: A randomized control trial. Journal of Autism and Developmental Disorders, 50, 4106–4120.
Hilton, C. L., Crouch, M. C., & Israel, H. (2008). Out-of-school participation patterns in children with high-functioning autism spectrum disorders. American Journal of Occupational Therapy, 62(5), 554–563.
Hirvikoski, T., & Blomqvist, M. (2015). High self-perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism, 19(6), 752–757.
Holm, M. B., Baird, J. M., Kim, Y. J., Rajora, K. B., D’Silva, D., Podolinsky, L., Mazefsky, C., & Minshew, N. (2014). Therapeutic horseback riding outcomes of parent-identified goals for children with autism spectrum disorder. Journal of Autism and Developmental Disabilities, 44(4), 937–947.
Holzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M., Gard, T., & Lazar, S. M. (2011). Mindfulness practice leads to increases in regional gray matter density. Psychiatry Research, 191(1), 36–43.
Hong, J., Bishop-Fitzpatrick, L., Smith, L., Greenberg, J., & Mailick, M. (2016). Factors associated with subjective quality of life of adults with autism spectrum disorder: Self-report vs. maternal report. Journal of Autism & Developmental Disorders, 46(4), 1368–1378.
Hourston, S., & Achtley, R. (2017). Autism and mind–body therapies: A systematic review. The Journal of Alternative and Complementary Medicine, 23(5), 331–339.
Hu, T., Zhang, D., Wang, J., Mistry, R., Ran, G., & Wang, X. (2014). Relation between emotion regulation and mental health: A meta-analysis review. Psychological Reports, 114(2), 341–362.
Hyun, G. J., Jung, T. W., Park, J. H., Kang, K. D., Kim, S. M., Son, Y. D., Cheong, J. H., Kim, B. N., & Han, D. H. (2016). Changes in gait balance and brain connectivity in response to equine-assisted activity and training in children with attention deficit hyperactivity disorder. The Journal of Alternative and Complementary Medicine, 22(4), 286–293.
Ives-Deliperi, V. L., Solms, M., & Meintjes, E. M. (2011). The neural substrates of mindfulness: An fMRI investigation. Social Neuroscience, 6(3), 231–242.
Kemeny, B., Hutchins, D., Gramlich, C., Craine, C., & Crandell, L. (2019). Identifying the best protocol: Social engagement or groundwork prior to therapeutic riding. American Journal of Recreation Therapy, 18(1), 19–30.
Kern, J. K., Fletcher, C. L., Garver, C. R., Mehta, J. A., Grannemann, B. D., Knox, K. R., Richardson, T. A., & Trivedi, M. H. (2011). Pcspective trial of equine-assisted activities in autism spectrum disorder. Alternative Therapies in Health and Medicine, 17(3), 14–20.
Kerns, C. M., Kendall, P. C., Berry, L., Souders, M. C., Franklin, M. E., Schultz, R. T., Miller, J., & Herrington, J. (2014). Traditional and atypical presentations of anxiety in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(11), 2851–2861. https://doi.org/10.1007/s10803-014-2141-7
Kiep, M., Spek, A. A., & Hoeben, L. (2015). Mindfulness-based therapy in adults with an autism spectrum disorder: Do treatment effects last? Mindfulness, 6(3), 637–644.
Kreiser, N. L., & White, S. W. (2014). Assessment of social anxiety in children and adolescents with autism spectrum disorder. Clinical Psychology Scientific Practice, 21(1), 18–31.
Kuhlthau, K., McDonnell, E., Coury, D. L., Payakachat, N., & Macklin, E. (2017). Associations of quality of life with health-related characteristics among children with autism. Autism. https://doi.org/10.1177/1362361317704420
Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., & Mandy, W. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. Lancet Psychiatry, 6(10), 819–829.
Lanni, K. E., Schupp, C. W., Simon, D., & Corbett, B. A. (2012). Verbal ability, social stress, and anxiety in children with autistic disorder. Autism, 16(2), 123–138.
Lanning, B. A., Baier, M. E., Ivey-Hatz, J., Krenek, N., & Tubbs, J. D. (2014). Effects of equine assisted activities on autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(8), 1897–1907.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, & coping. Springer.
Lickel, A., MacLean, W. E., Blakeley Smith, A., & Hepburn, S. (2012). Assessment of the prerequisite skills for cognitive behavioral therapy in children with and without autism spectrum disorders. Journal of Autism Developmental Disorders, 42(6), 992–1000.
London, M. D., Mackenzie, L., Lovarini, M., Dickson, C., & Alvarez-Campos, A. (2020). Animal assisted therapy for children and adolescents with autism spectrum disorder: Parent perspectives. Journal of Autism and Developmental Disorders, 50, 4492–4503. https://doi.org/10.1007/s10803-020-04512-5
Maddox, B. B., & White, S. W. (2015). Comorbid social anxiety disorder in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(12), 3949–3960.
Maisel, M. E., Stephenson, K. G., South, M., Rodgers, J., Freeston, M. H., & Gaigg, S. B. (2016). Modeling the cognitive mechanisms linking autism symptoms and anxiety in adults. Journal of Abnormal Psychology, 125(5), 692.
Mazefsky, C. A., Herrington, J., Siegel, M., Scarpa, A., Maddox, B., Scahill, L., & White, S. W. (2013). The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 52(7), 679–688.
Mazefsky, C. A., & White, S. W. (2014). Emotional regulation: Concepts and practice in autism spectrum disorder. Child Adolescent Psychiatry Clinics in North America, 23(1), 15–24.
McCraty, R., Atkinson, M., Tomasino, D., & Bradley, R. (2009). The coherent heart: Heart-brain interactions, psychophysiological coherence, and the emergence of system-wide order. Integral Review, 5(2), 1–106.
McCraty, R., Barrios-Choplin, B., Rozman, D., Atkinson, M., & Watkins, A. D. (1998). The impact of a new emotional self-management program on stress, emotions, heart rate variability, DHEA, and control. Integrated Physiological Behavioral Science, 33(2), 151–170.
McCraty, R., & Tomasino, D. (2006). The coherent heart: Heart-brain interactions, psychophysiological coherence, and the emergence of system-wide order. HeartMath Research Center, Institute of HeartMath.
McCraty, R., & Zayas, M. A. (2014). Cardiac coherence, self-regulation, autonomic stability, and psychosocial well-being. Frontiers in Psychology, 5(1090), 1–13.
McDaniel-Peters, B. C., & Wood, W. (2017). Autism and equine-assisted interventions: A systematic mapping review. Journal of Autism and Developmental Disorders, 47(10), 3220–3242.
McGeown, H. R., Johnstone, E. C., McKirdy, J., Owens, D. C., & Stanfield, A. C. (2013). Determinants of adult functional outcome in adolescents receiving special educational assistance. Journal of Intellectual Disability Research, 57(8), 766–773.
McVey, A. J., Schiltz, H., Haendel, A., Dolan, B. K., Willar, K. S., Pleiss, S., et al. (2017). Brief report: Does gender matter in intervention for ASD? Examining the impact of the PEERS® social skills intervention on social behavior among females with ASD. Journal of Autism and Developmental Disorders, 47(7), 2282–2289.
Mesibov, G., & Shea, V. (2011). Evidence-based practices and autism. Autism, 15(1), 114–133.
Moffitt, T. E., Arseneault, L., Belsky, D., Dickson, N., Hancox, R. J., Harrington, H., Houts, R., Poulton, R., Roberts, B. W., Ross, S., Sears, M. R., Thomson, W. M., & Caspi, A. (2011). A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences USA, 108, 2693–2698.
Mücke, M., Ludyga, S., Colledge, F., & Gerber, M. (2018). Influence of regular physical activity and fitness on stress reactivity as measured with the trier social stress test protocol: A systematic review. Sports Medicine, 48, 2607–2622.
Muris, P., Steerneman, P., Merckelbach, H., Holdrinet, I., & Meesters, C. (1998). Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders, 12(4), 387–393.
Muscatello, R. A., & Corbett, B. A. (2018). Comparing the effects of age, pubertal development, and symptom profile on cortisol rhythm in children and adolescents with autism spectrum disorder. Autism Research, 11(1), 110–120.
O’Haire, M. E. (2017). Research on animal-assisted intervention and autism spectrum disorder, 2012–2015. Applied Developmental Science, 21(3), 200–216.
Oberle, E., & Schonert-Reichl, K. (2014). Mindfulness in adolescence. In G. G. Noam (Ed.), New directions for youth development (p. 142). Wiley.
Odendaal, J. S. J., & Meintjes, R. A. (2003). Neurophysiological correlates of affiliative behaviour between humans and dogs. Veterinary Journal, 165, 296–301.
Oh, Y., Joung, Y. S., Jang, B., Yoo, J. H., Song, J., Kim, J., et al. (2018). Efficacy of hippotherapy versus pharmacotherapy in attention deficit/hyperactivity disorder: A randomized clinical trial. The Journal of Alternative and Complementary Medicine, 24(5), 463–471.
Orsmond, G. I., & Kuo, H. Y. (2011). The daily lives of adolescents with an autism spectrum disorder: Discretionary time use and activity partners. Autism, 15(5), 579–599.
Oswald, T. M., Winder-Patel, B., Ruder, S., Xing, G., Stahmer, A., & Solomon, M. (2018). A pilot randomized controlled trial of the ACCESS program: A group intervention to improve social, adaptive functioning, stress coping, and self-determinism outcomes in young adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(5), 1742–1760.
Ozsivadjian, A., Hibberd, C., & Hollocks, M. J. (2014). Brief report: The use of self-report measures in young people with autism spectrum disorder to assess symptoms of anxiety, depression, and negative thoughts. Journal of Autism and Developmental Disorders, 44(4), 969–974.
Pan, Z., Granger, D. A., Guerin, N. A., Shoffner, A., & Gabriels, R. L. (2019). Replication pilot trial of therapeutic riding and cortisol collection with children on the autism spectrum. Frontiers in Veterinary Science. https://doi.org/10.3389/fvets.2018.00312
Picci, G., & Scherf, K. S. (2015). A two-hit model of autism: Adolescence as the second hit. Clinical Psychological Science, 3(3), 349–371.
Pickard, H., Rijdsvijk, F., Happe, F., & Mandy, W. (2017). Are social and communication difficulties a risk factor for the development of social anxiety? Journal of the American Academy of Child and Adolescent Psychiatry, 56(4), 344–351.
Pisula, E., Pudio, M., & Slowinska, M. (2017). Behavioral and emotional problems in high-functioning girls and boys with autism spectrum disorders: Parents’ reports and adolescent self-reports. Autism, 21(6), 738–748. https://doi.org/10.1177/1362361316675119
Plessow, F., Fischer, R., Kirshbaum, C., & Goschke, T. (2011). Inflexibly focused under stress: Acute psychosocial stress increases shielding of action goals at the expense of reduced cognitive flexibility with increasing time lag to the stressor. Journal of Cognitive Neuroscience, 23(11), 3218–3227.
Porges, S. W. (2018). Polyvagal theory: A primer. In S. W. Porges & D. Dana (Eds.), Clinical applications of the polyvagal theory: The emergence of polyvagal-informed therapies. W. W. Norton & Company.
Quek, L. H., Sheffield, K., White, A., & Kelly, A. (2012). Co-occurring anger in young people with Asperger’s syndrome. Journal of Clinical Psychology, 68(10), 1142–1148.
Reyes, N. M., Pickard, K., & Reaven, J. (2019). Emotion regulation: A treatment target for autism spectrum disorder. Bulletin of the Menninger Clinic, 83(3), 205–234.
Reynard, A., Gevirtz, R., Berlow, R., Brown, M., & Boutelle, K. (2011). Heart rate variability as a marker of self-regulation. Applied Psychophysiology Biofeedback, 36, 209–215. https://doi.org/10.1007/s10484-011-9162-1
Ridderinkhof, A., de Bruin, E. I., Blom, R., & Bögels, S. M. (2018). Mindfulness-based program for children with autism spectrum disorder and their parents: Direct and long-term improvements. Mindfulness, 9(3), 773–791.
Ridderinkhof, A., de Bruin, E., van den Driesschen, S., & Bogels, S. M. (2020). Attention in children with autism spectrum disorder and the effects of a mindfulness-based program. Journal of Attention Disorders, 24(5), 681–692.
Roeser, R. W., & Zelazo, P. D. R. (2012). Contemplative science, education and child development: Introduction to the special section. Child Development Perspectives, 6(2), 143–145.
Rosenman, R., Tennekoon, V., & Hill, L. G. (2011). Measuring bias in self-reported data. International Journal of Behavioral Healthcare Research, 2(4), 320–322.
Salem-Guirgis, S., Albaum, C., Tablon, P., Riosa, P. B., Nicholas, D. B., Drmic, I. E., & Weiss, J. A. (2019). MYmind: A concurrent group-based mindfulness intervention for youth with autism and their parents. Mindfulness. https://doi.org/10.1007/s12671-019-01107-9
Samson, A. C., Hardan, A. Y., Lee, I. A., Phillips, J. M., & Gross, J. J. (2015a). Maladaptive behavior in autism spectrum disorder: The role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders., 45(11), 3424–3432.
Samson, A. A., Hardan, A. Y., Podell, R. W., Phillips, J. M., & Gross, J. J. (2015b). Emotion egulation in children and adolescents with autism spectrum disorder. Autism Research, 8(1), 9–18.
Scarpa, A., White, S. W., & Attwood, T. (Eds.). (2013). CBT for children and adolescents with high-functioning autism spectrum disorders. Guilford Press.
Seltzer, M. M., Shattuck, P., Abbeduto, L., & Greenberg, J. S. (2004). Trajectory of development in adolescents and adults with autism. Mental Retardation and Developmental Disabilities, 10(4), 234–247.
Shattuck, P. T., Seltzer, M. M., Greenburg, J. S., Orsmond, G. I., Bolt, D., Kring, S., Lounds, J., & Lord, C. (2007). Change in autism symptoms and maladaptive behaviors in adolescents and adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 37(9), 1735–1745.
Shirtcliff, E. A., Allison, A. L., Armstrong, J. M., Slattery, M. I., Kalin, N. H., & Essex, M. I. (2012). Longitudinal stability and developmental properties of salivary cortisol levels and circadian rhythms from childhood to adolescence. Developmental Psychology, 54(5), 493–502.
Singh-Giulio, N., Lancioni, G. E., Manikam, R., Winton, A. S., Singh, A. N. A., Singh, J., & Singh, A. D. A. (2011). A mindfulness-based strategy for self-management of aggressive behavior in autism. Research in Autism Spectrum Disorders, 5(3), 1153–1158.
Sizoo, B., & Kuiper, E. (2017). Cognitive behavior therapy and mindfulness-based stress reduction may be equally effective in reducing anxiety and depression in adults with autism spectrum disorders. Research in Developmental Disabilities. https://doi.org/10.1016/j.ridd.2017.03.004
Sofronoff, K., Attwood, T., Hinton, S., & Levin, I. (2007). A randomized controlled trial of a cognitive behavioral intervention for anger management in children diagnosed with Asperger syndrome. Journal of Autism and Developmental Disorders, 37(7), 1203–1214.
Solomon, O. (2012). Doing, being and becoming: The sociality of children with autism in activities with therapy dogs and other people. Cambridge Anthropology, 30(1), 109. https://doi.org/10.3167/ca.2012.300110
South, M., Rodgers, J., & Van Hecke, A. (2019). Anxiety and ASD: Current progress and ongoing challenges. Journal of Autism and Developmental Disorders, 47(12), 3679–3681.
Souza-Santos, C., dos Santos, J. F., Azevedo-Santos, I., & Teixeira-Machado, L. (2018). Dance and equine-assisted therapy in autism spectrum disorder: Crossover randomized clinical trial. Clinical Neuropsychiatry, 15(5), 284–290.
Spain, D., Sin, J., Linder, K. B., McMahon, J., & Happe, F. (2019). Social anxiety in autism spectrum disorder: A systematic review. Research in Autism Spectrum Disorders, 52, 51–68.
Spek, A. A., van Ham, N. C., & Nykliček, I. (2013). Mindfulness-based therapy in adults with an autism spectrum disorder: A randomized controlled trial. Research in Developmental Disabilities, 34(1), 246–253.
Spolskay, R. M., Romero, L. M., & Munck, A. U. (2000). How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews, 21(1), 55–89.
Stahmer, A. C., & Aarons, G. A. (2009). Attitudes toward adoption of evidence-based practices: A comparison of autism early intervention providers and children’s mental health providers. Psychological Services, 6(3), 223–234.
Taylor, J. L., & Corbett, B. A. (2014). A review of the rhythm and responsiveness of cortisol in individuals with autism spectrum disorders. Psychoneuroendricrinology, 49, 207–228.
Taylor, J. L., & Seltzer, M. M. (2012). Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders, 41(5), 566–574.
Thayer, J. F., Friedmand, B. H., & Boorkovec, T. D. (1996). Autonomic characteristics of generalized anxiety disorder and worry. Biological Psychiatry, 39(4), 255–266.
Tomarken, A. J., Hana, G. T., & Corbett, B. A. (2015). Temporal patterns, heterogeneity, and stability of diurnal cortisol rhythms in children with autism spectrum disorder. Psychoneuroendocrinology, 62, 217–226.
Tordjman, S., Anderson, G. M., Kermarrc, S., Bonnot, O., Geoffray, M., Brailly-Tabard, S., Chaouch, A., Colliot, I., Trabado, S., Bronsard, G., Coulon, N., Botbol, M., Charbuy, H., Camus, F., & Touitou, Y. (2014). Altered circadian patterns of salivary cortisol in low functioning children and adolescents with autism. Psychoneuroendocrinology, 50, 227–245.
Trzmiel, T., Purandare, B., Michalak, M., Zasadzka, E., & Pawlaczyk, M. (2019). Equine ssisted activities and therapies in children with autism: A systematic review and meta-analysis. Complementary Therapeutic Medicine, 42, 104–113.
Tse, C. Y. A., Pang, C. L., & Lee, P. H. (2018). Choosing an appropriate physical exercise to reduce stereotypical behavior in children with autism spectrum disorders: A non-randomized crossover study. Journal of Autism and Developmental Disorders, 48(5), 1666–1672.
Ung, D., Selles, R., Small, B. J., & Storch, E. A. (2015). A systematic review and meta-analysis of cognitive-behavioral therapy for anxiety in youth with high-functioning autism spectrum disorders. Child Psychiatry Human Development, 46(4), 533–547.
Van der Steen, S., Heineman, M. M. P., & Ernst, M. J. A. (2019). Evaluating animal-assisted interventions: An empirical illustration of differences between outcome measures. Animals, 9, 645.
Van Steensel, F. J. A., Bogels, S. M., & Perrin, S. (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis clinical child family. Psychology Review, 14(3), 302–317.
Vasa, R. A., Mazurek, M. O., Mahajan, R., Bennett, A. E., Bernal, M. P., Nozzolillo, A. A., Arnold, L. E., & Coury, D. L. (2016). Assessment and treatment of anxiety in youth with autism spectrum disorders. Pediatrics, 137(S2), S115–S123.
Viau, R., Arsenault-Lapierre, G., Fecteau, S., Champagne, N., Walker, C. D., & Lupien, S. (2010). Effect of service dogs on salivary cortisol secretion in autistic children. Psychoneuroendocrinology, 35, 1187–1193.
Wegner, M., Koutsandréou, F., Müller-Alcazar, A., Lautenbach, F., & Budde, H. (2019). Effects of different types of exercise training on the cortisol awakening response in children. Frontiers in Endocrinology. https://doi.org/10.3389/fendo.2019.00463
Welleck, S., & Blettner, M. (2012). On the proper use of crossover design in trials. Deutsches Arzteblatt International, 109(15) 276–281.
White, S. W., Mazefsky, C. A., Dichter, G. S., Chiu, P. H., Richey, J. A., & Ollendick, T. H. (2014). Social-cognitive, physiological, and neural mechanisms underlying emotion regulation impairments: Understanding anxiety in autism spectrum disorder. International Journal of Developmental Neuroscience, 39, 22–36.
White, S. W., Simmons, G. L., Gotham, K. O., Conner, C. M., Smith, I. C., Beck, K. B., & Mazefsky, C. A. (2018). Psychosocial treatments targeting anxiety and depression in adolescents and adults on the autism spectrum: Review of the latest research and recommended future directions. Current Psychiatry Reports, 20(10), 82.
White, W., Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229.
Whyte, E. M., Behrmann, M., Minshew, N. J., Garcia, N. V., & Scherf, K. S. (2015). Animal, but not human, faces engage the distributed face network in adolescents with autism. Developmental Science, 19(2), 306–317. https://doi.org/10.1111/desc.12305
Wijker, C., Leontjevas, R., Spek, A., & Enders-Slegers, M.-J. (2019). Effects of dog assisted therapy for adults with autism spectrum disorder: An exploratory randomized controlled trial. Journal of Autism and Developmental Disorders, 50, 2153–2163.
Wijker, C., van der Steen, S., Spek, A., Leontjevas, R., & Enders-Slegers, M. J. (2020). Social development of adults with autism spectrum disorder during dog-assisted therapy: A detailed observational analysis. International Journal of Environmental Research and Public Health, 17, 5922. https://doi.org/10.3390/ijerph17165922
Wood, J. J., Drahota, A., Sze, K., Har, K., Chiu, A., & Langer, D. A. (2009). Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized controlled trial. Journal of Child Psychology and Psychiatry, 50(3), 224–234.
Woodard, C. R., Harmony, C., Groden, J., & Audet, K. (2021). A comparison of the stress survey schedule in children with autism and typically developing children: A brief report. Journal of Autism and Developmental Disorders, 51(4), 1375–1384.
Wozniak, R. H., Leezenbaum, N. B., Northrup, J. B., West, K. L., & Iverson, J. M. (2017). The development of autism spectrum disorders: Variability and causal complexity. Wiley Interdisciplinary Review in Cognitive Science, 8, 1–2. https://doi.org/10.1002/wcs.1426
Zainal, H., & Magiati, I. (2019). A comparison between caregiver-reported anxiety and other emotional and behavioral difficulties in children and adolescents with autism spectrum disorders attending specialist or mainstream schools. Journal of Autism and Developmental Disorders, 49(7), 2653–2663.
Acknowledgments
Funding for this research was provided by the Horses and Humans Research Foundation. Individuals contributing considerable effort to the research include Jessica Dietrich, Kelly Gross, Emily Jones, Allison Kronyak, Kristen Laird, Mallory Reynolds, Anthony Rock, Morgan Shields, and Dil Singhabahu. The authors also would like to acknowledge support from the Slippery Rock University’s Storm Harbor Equestrian Center and Macoskey Center staff and volunteers.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kemeny, B., Burk, S., Hutchins, D. et al. Therapeutic Riding or Mindfulness: Comparative Effectiveness of Two Recreational Therapy Interventions for Adolescents with Autism. J Autism Dev Disord 52, 2438–2462 (2022). https://doi.org/10.1007/s10803-021-05136-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-021-05136-z