Abstract
Previous studies of associations between ASD and conception using assisted reproductive technology (ART) are inconsistent and few studies have examined associations with other infertility treatments or infertility disorders. We examined associations between ASD and maternal/paternal infertility disorders and numerous maternal treatments among 1538 mother–child pairs in the Study to Explore Early Development, a population-based case-control study. ASD was associated with any female infertility diagnosis and several specific diagnoses: blocked tubes, endometriosis, uterine-factor infertility, and polycystic ovarian syndrome. Stratified analyses suggested associations were limited to/much stronger among second or later births. The findings were not explained by sociodemographic factors such as maternal age or education or multiple or preterm birth. ASD was not associated with ART or non-ART infertility treatments.
Similar content being viewed by others
References
Ananth, C. V., Wilcox, A. J., Savitz, D. A., Bowes, W. A. Jr., & Luther, E. R. (1996). Effect of maternal age and parity on the risk of uteroplacental bleeding disorders in pregnancy. Obstetrics and Gynecology, 88(4 Pt 1), 511–516.
Arndt, T. L., Stodgell, C. J., & Rodier, P. M. (2005). The teratology of autism. International Journal Developmental Neuroscience, 23, 189–199.
Barradas, D. T., Barfield, W. D., Wright, V., D’Angelo, D., Manning, S. E., & Schieve, L. A. (2012). Assessment of assisted reproductive technology use questions: Pregnancy Risk Assessment Monitoring System Survey 2004. Public Health Reports, 127(5), 516–523.
Bauman, M. L., & Kemper, T. L. (2005). Neuroanatomic observations of the brain in autism: A review and future directions. International Journal Developmental Neuroscience, 23, 183–187.
Berlac, J. F., Hartwell, D., Skovlund, C. W., Langhoff-Roos, J., & Lidegaard, Ø. (2017) Endometriosis increases the risk of obstetrical and neonatal complications. Acta Obstetricia et Gynecologica Scandinavica. doi:10.1111/aogs.13111.
Blumberg, S. J., Bramlett, M. D., Kogan, M. D., Schieve, L. A., Jones, J. R., & Lu, M. C. (2013). Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011–2012. National Health Statistics Report, 65, 1–11.
Bolton, P. F., Golding, J., Emond, A., & Steer, C. D. (2012). Autism spectrum disorder and autistic traits in the Avon Longitudinal Study of Parents and Children: Precursors and early signs. Journal American Academy of Child & Adolescent Psychiatry, 51, 249–260.
Bungum, H. F., Vestergaard, C., & Knudsen, U. B. (2014). Endometriosis and type 1 allergies/immediate type hypersensitivity: A systematic review. European Journal of Obstetrics Gynecology and Reproductive Biology, 179, 209–215.
Christensen, D. L., Baio, J., Van Naarden Braun, K., et al. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2012. Morbidity and Mortality Weekly Report, 65(3), 1–23.
Conde-Agudelo, A., Rosas-Bermudez, A., & Norton, M. H. (2016) Birth spacing and risk of autism and other neurodevelopmental disabilities: A systematic review. Pediatrics, 137(5), e20153482. doi:10.1542/peds.2015-3482.
Confino, E., & Radwanska, E. (1992). Tubal factors in infertility. Current Opinions in Obstetrics and Gynecology, 4, 197–202.
Coughlin, S. S. (1990). Recall bias in epidemiologic studies. Journal of Clinical Epidemiology, 43(1), 87–91.
de Boer, E. J., den Tonkelaar, I., Burger, C. W., & van Leeuwen, F. E., OMEGA Project Group. (2005) Validity of self-reported causes of subfertility. American Journal of Epidemiology, 161(10), 978–986.
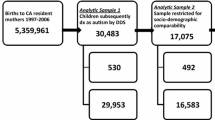
Fountain, C., Zhang, Y., Kissin, D. M., Schieve, L. A., Jamieson, D. J., Rice, C., & Bearman, P. (2015). Association between assisted reproductive technology conception and autism in California, 1997–2007. American Journal of Public Health, 105, 963–971.
Grether, J. K., Qian, Y., Croughan, M. S., Wu, Y. W., Schembri, M., Camarano, L., & Croen, L. A. (2013). Is infertility associated with childhood autism? Journal of Autism & Developmental Disorders, 43, 663–672.
Grimes, D. A., & Schulz, K. F. (2002). Bias and causal associations in observational research. Lancet, 359(9302), 248–252.
Horne, A. W., & Critchley, H. O. (2007). The effect of uterine fibroids on embryo implantation. Seminars on Reproductive Medicine, 25, 483–489.
Hvidtjorn, D., Grove, J., Schendel, D., Schieve, L. A., Svaerke, C., Ernst, E., & Thorsen, P. (2011). Risk of autism spectrum disorders in children born after assisted conception: A population-based follow-up study. Journal of Epidemiology and Community Health, 65, 497–502.
Kachuei, M., Jafari, F., Kachuei, A., & Keshteli, A. H. (2012). Prevalence of autoimmune thyroiditis in patients with polycystic ovary syndrome. Archives of Gynecology and Obstetrics, 285, 853–856.
Keskin Kurt, R., Okyay, A. G., Hakverdi, A. U., Gungoren, A., Dolapcioglu, K. S., Karateke, A., & Dogan, M. O. (2014). The effect of obesity on inflammatory markers in patients with PCOS: A BMI-matched case-control study. Archives of Gynecology and Obstetrics, 290, 315–319.
Kissin, D. M., Zhang, Y., Boulet, S. L., Fountain, C., Bearman, P., Schieve, L., Yeargin-Allsopp, M., & Jamieson, D. J. (2015). Association of assisted reproductive technology (ART) treatment and parental infertility diagnosis with autism in ART-conceived children. Human Reproduction, 30, 454–465.
Klemetti, R., Sevón, T., Gissler, M., & Hemminki, E. (2006). Health of children born as a result of in vitro fertilization. Pediatrics, 118, 1819–1827.
Knoester, M., Helmerhorst, F. M., van der Westerlaken, L. A., Walther, F. J., & Veen, S. (2007). Leiden Artificial Reproductive Techniques Follow-up Project (L-art-FUP). Matched follow-up study of 5 8-year-old ICSI singletons: Child behaviour, parenting stress and child (health-related) quality of life. Human Reproduction, 22, 3098–3107.
Kobayashi, H., Higashiura, Y., Shigetomi, H., & Kajihara, H. (2014). Pathogenesis of endometriosis: The role of initial infection and subsequent sterile inflammation (Review). Molecular Medicine Reports, 9, 9–15.
Kosidou, K., Dalman, C., Widman, L., Arver, S., Lee, B. K., Magnusson, C., & Gardner, R. M. (2016). Maternal polycystic ovary syndrome and the risk of autism spectrum disorders in the offspring: A population-based nationwide study in Sweden. Molecular Psychiatry, 21, 1441–1448.
Lyall, K., Baker, A., Hertz-Picciotto, I., & Walker, C. K. (2013). Infertility and its treatments in association with autism spectrum disorders: A review and results from the CHARGE study. International Journal of Environmental Research and Public Health, 10, 3715–3734.
Lyall, K., Pauls, D. L., Spiegelman, D., Santangelo, S. L., & Ascherio, A. (2012). Fertility therapies, infertility and autism spectrum disorders in the Nurses’ Health Study II. Paediatric and Perinatal Epidemiology, 26, 361–372.
Ornoy, A., Weinstein-Fudim, L., & Ergaz, Z. (2016). Genetic syndromes, maternal diseases and antenatal factors associated with autism spectrum disorders (ASD). Frontiers in Neuroscience, 10, 316. doi:10.3389/fnins.2016.00316.
Ott, J., Kurz, C., Braun, R., Promberger, R., Seemann, R., Vytiska-Binstorfer, E., & Walch, K. (2014). Overt hypothyroidism is associated with the presence of uterine leiomyoma: A retrospective analysis. European Journal of Obstetrics Gynecology and Reproductive Biology, 177, 19–22.
Palomba, S., Marotta, R., Di Cello, A., Russo, T., Falbo, A., Orio, F., Tolino, A., Zullo, F., Esposito, R., & La Sala, G. B. (2012). Pervasive developmental disorders in children of hyperandrogenic women with polycystic ovary syndrome: A longitudinal case-control study. Clinical Endocrinology, 77, 898–904.
Parazzini, F., Tozzi, L., & Bianchi, S. (2016). Pregnancy outcome and uterine fibroids. Best Practice & Research Clinical Obstetrics & Gynecology, 34, 74–84.
Sandin, S., Nygren, K. G., Iliadou, A., Hultman, C. M., & Reichenberg, A. (2013). Autism and mental retardation among offspring born after in vitro fertilization. JAMA: The Journal of the American Medical Association, 10, 75–84.
Schendel, D. E., Diguiseppi, C., Croen, L. A., Fallin, M. D., Reed, P. L., Schieve, L. A., Wiggins, L. D., Daniels, J., Grether, J., Levy, S. E., et al. (2012). The Study to Explore Early Development (SEED): A multisite epidemiologic study of autism by the Centers for Autism and Developmental Disabilities Research and Epidemiology (CADDRE) network. Journal of Autism and Developmental Disorders, 42, 2121–2140.
Schieve, L. A., Fountain, C., Boulet, S. L., Yeargin-Allsopp, M., Kissin, D. M., Jamieson, D. J., Rice, C., & Bearman, P. (2015). Does autism diagnosis age or symptom severity differ among children according to whether assisted reproductive technology was used to achieve pregnancy? Journal of Autism and Developmental Disorders, 45, 2991–3003.
Schieve, L. A., Rice, C., Devine, O., Maenner, M. J., Lee, L. C., Fitzgerald, R., Wingate, M. S., Schendel, D., Pettygrove, S., Van Naarden Braun, K. et al. (2011). Have secular changes in perinatal risk factors contributed to the recent autism prevalence increase? Development and application of a mathematical assessment model. Annals of Epidemiology, 21, 930–945.
Tobias, D. K., Gaskins, A. J., Missmer, S. A., Hu, F. B., Manson, J. E., Buck Louis, G. M., Zhang, C., & Chavarro, J. E. (2015). History of infertility and risk of type 2 diabetes mellitus: A prospective cohort study. Diabetologia, 58, 707–715.
Vannuccini, S., Clifton, V. L., Fraser, I. S., Taylor, H. S., Critchley, H., Giudice, L. C., & Petraglia, F. (2016). Infertility and reproductive disorders: Impact of hormonal and inflammatory mechanisms on pregnancy outcome. Human Reproduction Update, 22, 104–115.
Wen, W., & Wen, S. W. (2014). Expanding upon the ‘extreme male brain’ theory of autism as a common link between other major risk factors: A hypothesis. Medical Hypotheses, 82, 615–618.
Young, A. M., Chakrabarti, B., Roberts, D., Lai, M. C., Suckling, J., & Baron-Cohen, S. (2016). From molecules to neural morphology: Understanding neuroinflammation in autism spectrum condition. Molecular Autism, 7, 9. doi:10.1186/s13229-016-0068-x.
Zachor, D. A., & Ben Itzchak, E. (2011). Assisted reproductive technology and risk for autism spectrum disorder. Research in Developmental Disabilities, 32, 2950–2956.
Funding
This study was supported by six cooperative agreements from the Centers for Disease Control and Prevention: Cooperative Agreement Number U10DD000180, Colorado Department of Public Health; Cooperative Agreement Number U10DD000181, Kaiser Foundation Research Institute (CA); Cooperative Agreement Number U10DD000182, University of Pennsylvania; Cooperative Agreement Number U10DD000183, Johns Hopkins University; Cooperative Agreement Number U10DD000184, University of North Carolina at Chapel Hill; and Cooperative Agreement Number U10DD000498, Michigan State University.
Author information
Authors and Affiliations
Contributions
LAS made substantial contributions to acquisition of data, study conception and design, analysis and interpretation of data, drafting the article, revising the article critically for important intellectual content, and gave final approval of the version to be published. CD-B and SH made substantial contributions to study conception and design, analysis and interpretation of data, revising the article critically for important intellectual content, and gave final approval of the version to be published. CN, JD, CD, LAC, and GCW made substantial contributions to acquisition of data, study conception and design, interpretation of data, revising the article critically for important intellectual content, and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflict of interest for this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all participants in this study.
Additional information
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schieve, L.A., Drews-Botsch, C., Harris, S. et al. Maternal and Paternal Infertility Disorders and Treatments and Autism Spectrum Disorder: Findings from the Study to Explore Early Development. J Autism Dev Disord 47, 3994–4005 (2017). https://doi.org/10.1007/s10803-017-3283-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-017-3283-1