Abstract
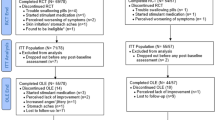
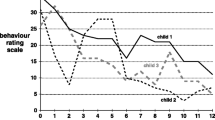
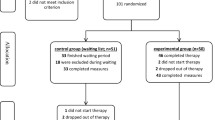
This pilot randomized controlled trial (RCT) investigated benefits of omega-3 fatty acid supplementation and Individual-Family Psychoeducational Psychotherapy (PEP; a family-focused, cognitive-behavioral therapy) for behavior problems among youth with depression. Participants aged 7–14 with DSM-IV-TR depressive disorders (N = 72; 56.9 % male) were randomized to 1 of 4 treatment conditions: PEP + omega-3, PEP monotherapy (with pill placebo), omega-3 monotherapy, or placebo (without active intervention). At screen, baseline, and 2, 4, 6, 9, and 12 weeks post-baseline, parents completed the SNAP-IV, which assesses attention-deficit/hyperactivity disorder symptoms, oppositional defiant disorder symptoms, and overall behavior problems. At screen, baseline (randomization), 6 and 12 weeks, parents completed the Eyberg Child Behavior Inventory (ECBI), which includes Intensity and Problem scales for child behavior problems. Youth who had a completed SNAP-IV or ECBI for at least two assessments during treatment (n = 48 and 38, respectively) were included in analyses of the respective outcome. ClinicalTrials.gov.:NCT01341925. Linear mixed effects models indicated a significant effect of combined PEP + omega-3 on SNAP-IV Total (p = 0.022, d = 0.80) and Hyperactivity/Impulsivity trajectories (p = 0.008, d = 0.80), such that youth in the combined group saw greater behavioral improvement than those receiving only placebo. Similarly, youth in combined treatment had more favorable ECBI Intensity trajectories than youth who received no active treatment (p = 0.012, d = 1.07). Results from this pilot RCT suggest that combined PEP + omega-3 is a promising treatment for co-occurring behavior symptoms in youth with depression.


Similar content being viewed by others
References
Ahn, J., Ahn, H. S., Cheong, J. H., & dela Pena, I. (2016). Natural product-derived treatments for attention-deficit/hyperactivity disorder: safety, efficacy, and therapeutic potential of combination therapy. Neural Plasticity. doi:10.1155/2016/1320423.
Ambrosini, P. J., Metz, C., Prabucki, K., & Lee, J.-C. (1989). Videotape reliability of the third revised edition of the K-SADS. Journal of the American Academy of Child and Adolescent Psychiatry, 28, 723–728. doi:10.1097/00004583-198909000-00013.
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR (4th ed., text revision ed.). Washington, DC: American Psychiatric Association.
Angold, A., & Costello, E. J. (1993). Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. American Journal of Psychiatry, 150, 1779–1791. doi:10.1176/ajp.150.12.1779.
Antshel, K. M., Faraone, S. V., & Gordon, M. (2012). Cognitive behavioral treatment outcomes in adolescent ADHD. Focus, 10, 334–345. doi:10.1176/appi.focus.10.3.334.
Axelson, D., Birmaher, B. J., Brent, D., Wassick, S., Hoover, C., Bridge, J., & Ryan, N. (2003). A preliminary study of the kiddie schedule for affective disorders and schizophrenia for school-age children mania rating scale for children and adolescents. Journal of Child and Adolescent Psychopharmacology, 13, 463–470. doi:10.1089/104454603322724850.
Birmaher, B., Arbelaez, C., & Brent, D. (2002). Course and outcome of child and adolescent major depressive disorder. Child and Adolescent Psychiatric Clinics of North America, 11, 619–637. doi:10.1016/S1056-4993(02)00011-1.
Birmaher, B., Brent, D., & the AACAP Work Group on Quality Issues (2007). Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 1503–1526. doi:10.1097/chi.0b013e318145ae1c.
Bloch, M. H., & Qawasmi, A. (2011). Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 991–1000. doi:10.1016/j.jaac.2011.06.008.
Bos, D. J., Oranje, B., Veerhoek, E. S., Van Diepen, R. M., Weusten, J. M., Demmelmair, H., et al. (2015). Reduced symptoms of inattention after dietary omega-3 fatty acid supplementation in boys with and without attention deficit/hyperactivity disorder. Neuropsychopharmacology, 40, 2298–2306. doi:10.1038/npp.2015.73.
Boylan, K., MacPherson, H. A., & Fristad, M. A. (2013). Examination of disruptive behavior outcomes and moderation in a randomized psychotherapy trial for mood disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 52, –708. doi:10.1016/j.jaac.2013.04.014.
Bridge, J. A., Iyengar, S., Salary, C. B., Barbe, R. P., Birmaher, B., Pincus, H. A., et al. (2007). Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA, 297, 1683–1696. doi:10.1001/jama.297.15.1683.
Bussing, R., Fernandez, M., Harwood, M., Hou, W., Garvan, C. W., Eyberg, S. M., & Swanson, J. M. (2008). Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms psychometric properties and normative ratings from a school district sample. Assessment, 15, 317–328. doi:10.1177/1073191107313888.
Chambers, W. J., Puig-Antich, J., Hirsch, M., Paez, P., Ambrosini, P. J., Tabrizi, M. A., & Davies, M. (1985). The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Archives of General Psychiatry, 42, 696–702. doi:10.1001/archpsyc.1985.01790300064008.
Clarke, G. N., Rohde, P., Lewinsohn, P. M., Hops, H., & Seeley, J. R. (1999). Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 272–279. doi:10.1097/00004583-199903000-00014.
Clayton, E. H., Hanstock, T. L., Hirneth, S. J., Kable, C. J., Garg, M. L., & Hazell, P. L. (2009). Reduced mania and depression in juvenile bipolar disorder associated with long-chain omega-3 polyunsaturated fatty acid supplementation. European Journal of Clinical Nutrition, 63, 1037–1040. doi:10.1038/ejcn.2008.81.
Costello, E. J., Erkanli, A., & Angold, A. (2006). Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry, 47, 1263–1271. doi:10.1111/j.1469-7610.2006.01682.x.
Diamond, G. S., Reis, B. F., Diamond, G. M., Siqueland, L., & Isaacs, L. (2002). Attachment-based family therapy for depressed adolescents: a treatment development study. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 1190–1196. doi:10.1097/00004583-200210000-00008.
Eyberg, S. M., & Pincus, D. (1999). Eyberg child behavior inventory & sutter-eyberg student behavior inventory-revised: professional manual. Odessa: Psychological Assessment Resources.
Eyberg, S. M., & Ross, A. W. (1978). Assessment of child behavior problems: the validation of a new inventory. Journal of Clinical Child Psychology, 7, 113–116. doi:10.1080/15374417809532835.
Feingold, A. (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods, 14, 43–53. doi:10.1037/a0014699.
Fristad, M. A., Verducci, J. S., Walters, K., & Young, M. E. (2009). Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Archives of General Psychiatry, 66, 1013–1021. doi:10.1001/archgenpsychiatry.2009.112.
Fristad, M. A., Goldberg-Arnold, J. S., & Leffler, J. M. (2011). Psychotherapy for children with bipolar and depressive disorders. New York: Guilford Press.
Fristad, M. A., Young, A. S., Vesco, A. T., Nader, E. S., Healy, K. Z., Gardner, W., et al. (2015). A randomized controlled trial of individual family psychoeducational psychotherapy & omega-3 fatty acids in youth with subsyndromal bipolar disorder. Journal of Child and Adolescent Psychopharmacology, 25, 764–774. doi:10.1089/cap.2015.0132.
Fristad, M. A., Vesco, A. T., Young, A. S., Healy, K. Z., Nader, E. S., Gardner, W.,… Arnold, L. E. (2016). Pilot RCT of omega-3 and individual-family psychoeducational psychotherapy for children and adolescents with depression. Journal of Clinical Child and Adolescent Psychology (in press).
Gillies, D., Sinn, J., Lad, S. S., Leach, M. J., & Ross, M. J. (2012). Polyunsaturated fatty acids (PUFA) for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database of Systematic Reviews, 7, CD007986. doi:10.1002/14651858.CD007986.pub2.
Jacobs, R. H., Becker-Weidman, E. G., Reinecke, M. A., Jordan, N., Silva, S. G., Rohde, P., & March, J. S. (2010). Treating depression and oppositional behavior in adolescents. Journal of Clinical Child and Adolescent Psychology, 39, 559–567. doi:10.1080/15374416.2010.486318.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988. doi:10.1097/00004583-199707000-00021.
Knapp, M., McCrone, P., Fombonne, E., Beecham, J., & Wostear, G. (2002). The Maudsley long-term follow-up of child and adolescent depression 3. Impact of comorbid conduct disorder on service use and costs in adulthood. British Journal of Psychiatry, 180, 19–23. doi:10.1192/bjp.180.1.19.
Kovacs, M. (1996). Presentation and course of major depressive disorder during childhood and later years of the life span. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 705–715. doi:10.1097/00004583-199606000-00010.
Lewinsohn, P. M., Clarke, G. N., Hops, H., & Andrews, J. (1990). Cognitive-behavioral treatment for depressed adolescents. Behavior Therapy, 21, 385–401. doi:10.1016/s0005-7894(05)80353-3.
Nemets, H., Nemets, B., Apter, A., Bracha, Z., & Belmaker, R. H. (2006). Omega-3 treatment of childhood depression: a controlled, double-blind pilot study. American Journal of Psychiatry, 163, 1098–1100. doi:10.1176/ajp.2006.163.6.1098.
Owen, C., Rees, A.-M., & Parker, G. (2008). The role of fatty acids in the development and treatment of mood disorders. Current Opinion in Psychiatry, 21, 19–24. doi:10.1097/YCO.0b013e3282f29841.
Pliszka, S., & AACAP Work Group on Quality Issues (2007). Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 894–921. doi:10.1097/chi.0b013e318054e724.
Raine, A., Portnoy, J., Liu, J., Mahoomed, T., & Hibbeln, J. R. (2015). Reduction in behavior problems with omega-3 supplementation in children aged 8-16 years: a randomized, double-blind, placebo-controlled, stratified, parallel-group trial. Journal of Child Psychology and Psychiatry, 56, 509–520. doi:10.1111/jcpp.12314.
Richardson, A. J. (2003). The importance of omega-3 fatty acids for behaviour, cognition and mood. Scandinavian Journal of Nutrition, 47, 92–98. doi:10.1080/11026480310007944.
Rohde, P., Clarke, G. N., Lewinsohn, P. M., Seeley, J. R., & Kaufman, N. K. (2001). Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 795–802. doi:10.1097/00004583-200107000-00014.
Smeets, K. C., Leeijen, A. A., van der Molen, M. J., Scheepers, F. E., Buitelaar, J. K., & Rommelse, N. N. (2015). Treatment moderators of cognitive behavior therapy to reduce aggressive behavior: a meta-analysis. European Child & Adolescent Psychiatry, 24, 255–264. doi:10.1007/s00787-014-0592-1.
Sonuga-Barke, E. J., Brandeis, D., Cortese, S., Daley, D., Ferrin, M., Holtmann, M., et al. (2013). Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. American Journal of Psychiatry, 170, 275–289. doi:10.1176/appi.ajp.2012.12070991.
Steiner, H., Remsing, L., & AACAP Work Group on Quality Issues (2007). Practice parameter for the assessment and treatment of children and adolescents with oppositional defiant disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 126–141. doi:10.1097/01.chi.0000246060.62706.af.
Sukhodolsky, D. G., Kassinove, H., & Gorman, B. S. (2004). Cognitive-behavioral therapy for anger in children and adolescents: a meta-analysis. Aggression and Violent Behavior, 9, 247–269. doi:10.1016/j.avb.2003.08.005.
Swanson, J. M. (1992). School-based assessments and interventions for ADD students. Irvine: KC Publishing.
Swanson, J. M., Kraemer, H. C., Hinshaw, S. P., Arnold, L. E., Conners, C. K., Abikoff, H. B., et al. (2001). Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 168–179. doi:10.1097/00004583-200102000-00011.
TADS Team (2004). Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: treatment for adolescents with depression study (TADS) randomized controlled trial. JAMA, 292, 807–820. doi:10.1001/jama.292.7.807.
Tammam, J. D., Steinsaltz, D., Bester, D. W., Semb-Andenaes, T., & Stein, J. F. (2016). A randomised double-blind placebo-controlled trial investigating the behavioural effects of vitamin, mineral and n-3 fatty acid supplementation in typically developing adolescent schoolchildren. British Journal of Nutrition, 115, 361–373. doi:10.1017/S0007114515004390.
U.S. Food and Drug Administration (2004). FDA launches a multi-pronged strategy to strengthen safeguards for children treated with antidepressant medications. Silver Spring: U.S. Food and Drug Administration.
Weisz, J. R., McCarty, C. A., & Valeri, S. M. (2006). Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychological Bulletin, 132, 132–149. doi:10.1037/0033-2909.132.1.132.
Acknowledgments
This research was supported by National Institute of Mental Health award# R34 MH85875; the content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. The authors would like to thank staff who collected data and provided therapy, families who participated, and OmegaBrite, who provided study capsules.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Young has received research funding from Psychnostics, LLC. Dr. Arnold has received research funding from Curemark, Forest, Lilly, Neuropharm, Novartis, Noven, Shire, Supernus, and YoungLiving (as well as NIH and Autism Speaks) and has consulted with or been on advisory boards for Arbor, Gowlings, Ironshore, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Roche, Seaside Therapeutics, Sigma Tau, Shire, Tris Pharma, and Waypoint. Dr. Fristad receives royalties from Guilford Press, American Psychiatric Press and CFPSI for treatment manuals, workbooks and a diagnostic instrument reported on in this study and honoraria from Physician’s Post-Graduate Press and the American Occupational Therapy Association.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent/assent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Young, A.S., Arnold, L.E., Wolfson, H.L. et al. Psychoeducational Psychotherapy and Omega-3 Supplementation Improve Co-Occurring Behavioral Problems in Youth with Depression: Results from a Pilot RCT. J Abnorm Child Psychol 45, 1025–1037 (2017). https://doi.org/10.1007/s10802-016-0203-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-016-0203-3