Abstract
Purpose
To assess changes in monocyte-to-high-density lipoprotein (HDL) ratio (MHR), neutrophil-to-lymphocyte ratio (NLR), and systemic immune-inflammation index (SII) with Graves’ ophthalmopathy (GO) and their possible relation with GO disease activity and severity.
Methods
A total of 20 patients with GO and 24 healthy controls were involved in the study. The thyroid status, MHR (monocyte count/HDL cholesterol level), NLR (neutrophil count/lymphocyte count) and SII [(neutrophil count × platelet count)/lymphocyte count] were compared between the groups. The relation of systemic inflammation parameters with disease activity and severity was evaluated.
Results
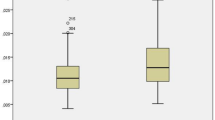
The mean Clinical Activity Score (CAS) was 0.75 ± 0.78 in the GO group. None of the patients were active. The severity was mild for 14 (70.0%) patients and moderate-to-severe for 6 (30.0%) patients. MHR (17.28 ± 5.56 vs. 13.28 ± 5.08), NLR (2.51 ± 1.09 vs. 1.69 ± 0.53) and SII [600.42 (391.79–837.16) vs. 413.69 (344.26–603.82)] values were significantly increased in GO patients than in the controls (p = 0.017, p = 0.005 and p = 0.036, respectively). CAS was significantly correlated with MHR (r = 0.815, p < 0.001), NLR (r = 0.768, p = 0.017) and SII (r = 0.837, p < 0.001). The severity of GO was associated with increased MHR, NLR and SII (p = 0.019, p = 0.036 and p = 0.008, respectively). ROC analysis demonstrated that MHR, NLR and SII have a good ability to differentiate GO patients from healthy individuals.
Conclusion
GO patients have higher MHR and SII levels than healthy controls. Higher MHR, NLR and SII values were associated with increasing disease severity and activity, supporting the efficacy of these non-invasive, low-cost markers in determining the course of GO. Future prospective controlled trials are needed to elucidate the relation between inflammatory markers and GO.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, [BYT], upon reasonable request.
References
Hiromatsu Y, Eguchi H, Tani J, Kasaoka M, Teshima Y (2014) Graves’ ophthalmopathy: epidemiology and natural history. Intern Med 53:353–360. https://doi.org/10.2169/internalmedicine.53.1518
Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, Perros P, Salvi M, Wiersinga WM, European Group on Graves’ Orbitopathy (EUGOGO) (2016) The 2016 European Thyroid Association/European Group on Graves’ Orbitopathy Guidelines for the Management of Graves’ Orbitopathy. Eur Thyroid J 5:9–26. https://doi.org/10.1159/000443828
Khong JJ, McNab AA, Ebeling PR, Craig JE, Selva D (2016) Pathogenesis of thyroid eye disease: review and update on molecular mechanisms. Br J Ophthalmol 100:142–150. https://doi.org/10.1136/bjophthalmol-2015-307399
Li N (2008) Platelet-lymphocyte cross-talk. J Leukoc Biol 83:1069–1078. https://doi.org/10.1189/jlb.0907615
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102:5–14
Celik T (2018) Assessment of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with dry eye disease. Ocul Immunol Inflamm 26:1219–1222. https://doi.org/10.1080/09273948.2017.1340486
Erol MK, Balkarli A, Yucel O, Akar Y, Dogan B, Suren E (2017) Neutrophil/lymphocyte ratio and mean platelet volume in central serous chorioretinopathy. Ther Clin Risk Manag 13:945–950. https://doi.org/10.2147/TCRM.S138581
Katipoğlu Z, Mirza E, Oltulu R, Katipoglu B (2020) May monocyte/HDL cholesterol ratio (MHR) and neutrophil/lymphocyte ratio (NLR) be an indicator of inflammation and oxidative stress in patients with keratoconus? Ocul Immunol Inflamm 28:632–636. https://doi.org/10.1080/09273948.2019.1611876
Şatırtav G, Mirza E, Oltulu R, Mirza GD, Kerimoğlu H (2020) Assessment of monocyte/HDL ratio in branch retinal vein occlusion. Ocul Immunol Inflamm 28:463–467. https://doi.org/10.1080/09273948.2019.1569244
Tang B, Li S, Han J, Cao W, Sun X (2020) Associations between blood cell profiles and primary open-angle glaucoma: a retrospective case-control study. Ophthalmic Res 63:413–422. https://doi.org/10.1159/000504450
Atılgan CÜ, Şendül SY, Kösekahya P, Çağlayan M, Alkan A, Güven D et al (2018) Evaluation of neutrophil-to-lymphocyte ratio and mean platelet volume in patients with active and inactive thyroid orbitopathy. Sisli Etfal Hastan Tip Bul 52:26–30. https://doi.org/10.14744/SEMB.2017.07269
Celik T (2017) Neutrophil-to-lymphocyte ratio in thyroid ophthalmopathy. Bratisl Lek Listy 118:495–498. https://doi.org/10.4149/BLL_2017_095
Szydełko J, Litwińczuk M, Szydełko M, Matyjaszek-Matuszek B (2020) Neutrophil-to-lymphocyte, monocyte-to-lymphocyte and platelet-to-lymphocyte ratios in relation to clinical parameters and smoking status in patients with graves’ orbitopathy-novel insight into old tests. J Clin Med 9:3111. https://doi.org/10.3390/jcm9103111
Vural G, Gümüsyayla Ş (2018) Monocyte-to-high density lipoprotein ratio is associated with a decreased compound muscle action potential amplitude in patients with diabetic axonal polyneuropathy. Medicine (Baltimore) 97:e12857. https://doi.org/10.1097/MD.0000000000012857
Ganjali S, Gotto AM Jr, Ruscica M, Atkin SL, Butler AE, Banach M et al (2018) Monocyte-to-HDL-cholesterol ratio as a prognostic marker in cardiovascular diseases. J Cell Physiol 233:9237–9246. https://doi.org/10.1002/jcp.27028
Usta A, Avci E, Bulbul CB, Kadi H, Adali E (2018) The monocyte counts to HDL cholesterol ratio in obese and lean patients with polycystic ovary syndrome. Reprod Biol Endocrinol 16:34. https://doi.org/10.1186/s12958-018-0351-0
Yılmaz M, Kayançiçek H (2018) A new inflammatory marker: elevated monocyte to HDL cholesterol ratio associated with smoking. J Clin Med 7:76. https://doi.org/10.3390/jcm7040076
Belviranli S, Oltulu R, Gundogan AO, Mirza E, Okka M (2022) Evaluation of the systemic inflammation in patients with pterygium: monocyte-to- high-density lipoprotein cholesterol ratio and hematologic indexes of inflammation. Middle East Afr J Ophthalmol 28:211–215. https://doi.org/10.4103/meajo.meajo_75_21
Oltulu R, Katipoğlu Z, Gündoğan AO, Mirza E, Belviranlı S (2022) Evaluation of inflammatory biomarkers in patients with keratoconus. Eur J Ophthalmol 32:154–159. https://doi.org/10.1177/11206721211000644
Zhang J, Li Y, Zhou Y, Wang K, Pan C, Zhao Y et al (2021) Monocyte to high-density lipoprotein ratio: a novel predictive marker of disease severity and prognosis in patients with neuromyelitis optica spectrum disorders. Front Neurol 12:763793. https://doi.org/10.3389/fneur.2021.763793
Kim HB, Kim A, Kim Y, Kim GT, Ahn E, So MW et al (2021) Associations of serum monocyte-to-high-density lipoprotein cholesterol ratio with digital ulcers and skin fibrosis in patients with systemic sclerosis. Scand J Rheumatol 50:231–238. https://doi.org/10.1080/03009742.2020.1837237
Ci W, Wan J, Han J, Zou K, Ge C, Pan L et al (2023) Monocyte-to-high-density lipoprotein ratio as a predictor for patients with Takayasu arteritis and coronary involvement: a double-center, observational study. Front Immunol 14:1120245. https://doi.org/10.3389/fimmu.2023.1120245
López P, Rodríguez-Carrio J, Martínez-Zapico A, Pérez-Álvarez ÁI, Suárez-Díaz S, Mozo L et al (2020) Low-density granulocytes and monocytes as biomarkers of cardiovascular risk in systemic lupus erythematosus. Rheumatology (Oxford) 59:1752–1764. https://doi.org/10.1093/rheumatology/keaa016.Erratum.In:Rheumatology(Oxford).2020;59:1795
Uslu AU, Küçük A, Şahin A, Ugan Y, Yılmaz R, Güngör T et al (2015) Two new inflammatory markers associated with Disease Activity Score-28 in patients with rheumatoid arthritis: neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Int J Rheum Dis 18:731–735. https://doi.org/10.1111/1756-185X.12582
Lee HN, Kim YK, Kim GT, Ahn E, So MW, Sohn DH et al (2019) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio as predictors of 12-week treatment response and drug persistence of anti-tumor necrosis factor-α agents in patients with rheumatoid arthritis: a retrospective chart review analysis. Rheumatol Int 39:859–868. https://doi.org/10.1007/s00296-019-04276-x
Duru Z, Altunel O, Alabay B, Sirakaya E, Sirakaya E, Kucuk B et al (2021) Elevated monocyte-to-high-density lipoprotein ratio as an indicator of systemic inflammation in patients with branch retinal vein occlusion. Beyoglu Eye J 6:212–216. https://doi.org/10.14744/bej.2021.94547
Tang X, Tan Y, Yang Y, Li M, He X, Lu Y et al (2021) Association of the monocyte-to-high-density lipoprotein cholesterol ratio with diabetic retinopathy. Front Cardiovasc Med 8:707008. https://doi.org/10.3389/fcvm.2021.707008
Mirza E, Oltulu R, Katipoğlu Z, Mirza GD, Özkağnıcı A (2020) Monocyte/HDL ratio and lymphocyte/monocyte ratio in patients with pseudoexfoliation syndrome. Ocul Immunol Inflamm 28:142–146. https://doi.org/10.1080/09273948.2018.1545913
Fu S, Yan J, Tan Y, Liu D (2021) Prognostic value of systemic immune-inflammatory index in survival outcome in gastric cancer: a meta-analysis. J Gastrointest Oncol 12:344–354. https://doi.org/10.21037/jgo-20-252
Fois AG, Paliogiannis P, Scano V, Cau S, Babudieri S, Perra R et al (2020) The systemic inflammation index on admission predicts in-hospital mortality in COVID-19 patients. Molecules 25:5725. https://doi.org/10.3390/molecules25235725
Yang YL, Wu CH, Hsu PF, Chen SC, Huang SS, Chan WL et al (2020) Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest 50:e13230. https://doi.org/10.1111/eci.13230
Zuo W, Chen T, Song J, Ai M (2023) Assessment of systemic immune-inflammation index levels in patients with retinal vein occlusion. Ocul Immunol Inflamm 31:491–495. https://doi.org/10.1080/09273948.2022.2032199
Ozarslan Ozcan D, Kurtul BE, Ozcan SC, Elbeyli A (2022) Increased systemic immune-inflammation index levels in patients with dry eye disease. Ocul Immunol Inflamm 30:588–592. https://doi.org/10.1080/09273948.2020.1821899
Kurtul BE, Cakmak AI, Elbeyli A, Ozcan SC, Ozarslan Ozcan D, Kimyon G (2021) Evaluation of systemic immune-inflammation index level as a novel marker for severity of noninfectious uveitis. Int Ophthalmol 41:3615–3622. https://doi.org/10.1007/s10792-021-01924-9
Yavuz S, Ece A (2014) Mean platelet volume as an indicator of disease activity in juvenile SLE. Clin Rheumatol 33:637–641. https://doi.org/10.1007/s10067-014-2540-3
Ozdemir R, Karadeniz C, Doksoz O, Celegen M, Yozgat Y, Guven B et al (2014) Are mean platelet volume and platelet distribution width useful parameters in children with acute rheumatic carditis? Pediatr Cardiol 35:53–56. https://doi.org/10.1007/s00246-013-0738-9
Tecer D, Sezgin M, Kanık A, İncel NA, Çimen ÖB, Biçer A, Şahin G et al (2016) Can mean platelet volume and red blood cell distribution width show disease activity in rheumatoid arthritis? Biomark Med 10:967–974. https://doi.org/10.2217/bmm-2016-0148
Sepas HN, Negahi A, Mousavie SH, Nasiri M (2019) Evaluation of the potential association of platelet levels, mean platelet volume and platelet distribution width with acute appendicitis. Open Access Maced J Med Sci 7:2271–2276. https://doi.org/10.3889/oamjms.2019.244
Acknowledgements
None.
Funding
No specific funding was received from any funding bodies in the public, commercial or not for-profit sectors to carry out the work described in this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: BYT; Methodology: BYT; Formal analysis and investigation: BYT; Writing—original draft preparation: BYT; Writing—review and editing: BYT, AE, BÖ. Funding acquisition: none, Resources: none; Supervision: BYT and BÖ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Ethical approval
The study was reviewed and approved by the local ethics committee of Kocaeli University (Approval number: GOKAEK-2022/11.01).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was presented in Turkish Ophthalmological Association 45. Spring Symposium in Istanbul/Turkey as an oral presentation. This article is an expanded and detailed version of the oral presentation.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yılmaz Tuğan, B., Ergen, A. & Özkan, B. Monocyte-to-high-density lipoprotein ratio and systemic immune-inflammation index: Potential parameters for the evaluation of disease activity and severity in Graves’ ophthalmopathy?. Int Ophthalmol 44, 154 (2024). https://doi.org/10.1007/s10792-024-03077-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03077-x