Abstract
Purpose
The purpose of the study was to investigate the parapapillary choroidal microvasculature in thyroid eye disease (TED) using optical coherence tomography angiography (OCTA).
Methods
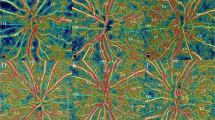
Only one eye of each subject was included in the study. Patients with TED and controls were included in the study. Participants were divided into three groups: control, inactive TED (ITED) and active TED (ATED). OCTA scans of the optic discs were obtained in a 4.5 × 4.5-mm rectangular area. Radial peripapillary capillary (RPC) density and peripapillary retinal nerve fibre layer (pRNFL) thickness were automatically calculated by the device software. Parapapillary choroidal microvasculature (PPCMv) density was automatically calculated using MATLAB software.
Results
Forty-one patients with TED and 40 controls were included in the study. RPC density was significantly decreased in the ATED and dysthyroid optic neuropathy (DON) group compared to the controls and ITED group. There was significant increase in pRNFL in the ATED group. PPCMv density increased in the ATED group compared to the controls in whole ring area. The RPC density was significantly correlated with the TSHr Ab level (r < − 0.396, p < 0.001). Clinical activity score correlated positively with PPCMv density (r = 0.349, p = 0.001) but negatively with RPC density (r = − 0.321, p = 0.004).
Conclusion
Changes in peripapillary microvascular perfusion may play a role in the development of DON. As the severity of TED increases with clinical activity, so do the changes observed in peripapillary parameters. The decrease in RPC density may be due to compression caused by optic disc oedema, which may result in reduced blood flow. The increase in PPCMv density may be related to factors such as orbital congestion.


Similar content being viewed by others

Data availability
The data sets generated and/or analysed in the current study are available from the corresponding author upon reasonable request.
References
Weiler DL (2017) Thyroid eye disease: a review. Clin Exp Optom 100(1):20–25
Gupta S, Douglas R (2011) The pathophysiology of thyroid eye disease (TED): implications for immunotherapy. Curr Opin Ophthalmol 22(5):385
Shan SJ, Douglas RS (2014) The pathophysiology of thyroid eye disease. J Neuroophthalmol 34(2):177–185
Scott IU, Siatkowski RM (1999) Thyroid eye disease. Semin Ophthalmol 4(2):52–61
Mourits M, Koornneef L, Wiersinga W et al (1989) Clinical criteria for the assessment of disease activity in Graves’ ophthalmopathy: a novel approach. Br J Ophthalmol 73(8):639–644
Bartalena L, Baldeschi L, Boboridis K et al (2016) The 2016 European thyroid association/European group on graves’ orbitopathy guidelines for the management of Graves’ orbitopathy. Eur Thyroid J 5(1):9–26
Jia Y, Wei E, Wang X et al (2016) Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology 121(7):1322–1332
Fard MA, Safizadeh M, Shaabani A et al (2021) Automated evaluation of parapapillary choroidal microvasculature in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Am J Ophthalmol 224:178–184
Konuk O, Onaran Z, Ozhan Oktar S et al (2009) Intraocular pressure and superior ophthalmic vein blood flow velocity in Graves’ orbitopathy: relation with the clinical features. Graefe’s Arch Clin Exp Ophthalmol 247:1555–1559
Özkan B, Koçer ÇA, Altintaş Ö et al (2016) Choroidal changes observed with enhanced depth imaging optical coherence tomography in patients with mild graves orbitopathy. Eye 30(7):917–924
Hayreh SS (2001) The blood supply of the optic nerve head and the evaluation of it—Myth and reality. Prog Ret Eye Res 20(5):563–593
Hojati S, Kafieh R, Fardafshari P et al (2020) A MATLAB package for automatic extraction of flow index in OCT-A images by intelligent vessel manipulation. SoftwareX 12:100510
Fard MA, Salabati M, Mahmoudzadeh R et al (2020) Automated evaluation of parapapillary choroidal microvasculature in ischemic optic neuropathy and open angle glaucoma. Invest Ophthalmol Vis Sci 61(3):35
Delaey C, Van de Voorde J (2000) Regulatory mechanisms in the retinal and choroidal circulation. Ophthalmic Res 32(6):249–256
Alm A, Bill A (1973) Ocular and optic nerve blood flow at normal and increased intraocular pressures in monkeys (Macaca irus): a study with radioactively labelled microspheres including flow determinations in brain and some other tissues. Exp Eye Res 15(1):15–29
Coskun E, Gurler B, Pehlivan Y et al (2013) Enhanced depth imaging optical coherence tomography findings in Behcet disease. Ocul Immunol Inflamm 21(6):440–445
Çalışkan S, Acar M, Gürdal C (2017) Choroidal thickness in patients with Graves’ ophthalmopathy. Curr Eye Res 42(3):484–490
Agrawal R, Gupta P, Tan K-A et al (2016) Choroidal vascularity index as a measure of vascular status of the choroid: measurements in healthy eyes from a population-based study. Sci Rep 6(1):1–9
Loiudice P, Pellegrini M, Marinò M et al (2021) Choroidal vascularity index in thyroid-associated ophthalmopathy: a cross-sectional study. Eye Vis 8(1):1–8
Dave TV, Jonnadula GB, Lanka P et al (2022) Choroidal vascularity index in thyroid eye disease: comparison with controls and application in diagnosing non-inflammatory active disease. Orbit 41(1):89–96
Zhang T, Xiao W, Ye H et al (2019) Peripapillary and macular vessel density in dysthyroid optic neuropathy: an optical coherence tomography angiography study. Invest Ophthalmol Vis Sci 60(6):1863–1869
Jian H, Wang Y, Ou L et al (2022) Altered peripapillary vessel density and nerve fiber layer thickness in thyroid-associated ophthalmopathy using optical coherence tomography angiography. Int Ophthalmol 42(3):855–862
Jamshidian Tehrani M, Mahdizad Z, Kasaei A et al (2019) Early macular and peripapillary vasculature dropout in active thyroid eye disease. Graefe’s Arch Clin Exp Ophthalmol 257:2533–2540
Diana T, Kahaly GJ (2018) Thyroid stimulating hormone receptor antibodies in thyroid eye disease—Methodology and clinical applications. Ophthalmic Plast Reconst Surg 34(4S):S13–S19
Balzan S, Del Carratore R, Nicolini G et al (2012) Proangiogenic effect of TSH in human microvascular endothelial cells through its membrane receptor. J Clin Endocrinol 97(5):1763–1770
Dolman P (2021) Dysthyroid optic neuropathy: evaluation and management. J Endocrinol Invest 44(3):421–429
Funding
The authors declare that no funding, grants or other support were received during the preparation of this manuscript. The authors have no relevant financial interests to disclose.
Author information
Authors and Affiliations
Contributions
HS contributed to methodology, data curation, formal analysis, statistical and image processing software and writing—original draft. FO helped in conceptualisation, data curation, investigation, validation and writing—revision and editing. MU helped in methodology, project management, visualisation and writing—revision and editing. DGS helped in validation, visualisation and writing—revision and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no potential conflicts of interest.
Ethics approval and informed consent
The study protocol was approved by the local ethics committee of Erciyes University (No.: 2021/356). Written informed consent was obtained from all individual participants.
Consent for publication
This paper has not been published elsewhere. It is not currently under consideration for publication elsewhere.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sener, H., Ozer, F., Unlu, M. et al. Automated evaluation of parapapillary choroidal microvasculature in thyroid eye disease. Int Ophthalmol 43, 4323–4331 (2023). https://doi.org/10.1007/s10792-023-02844-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02844-6