Abstract
Purpose
To analyse the ocularist’s perspective on the management of the anophthalmic socket and external ocular prosthesis (EOP).
Methods
Ocularists from two countries were invited to participate in an online questionnaire. Data were collected on demographics, anophthalmic socket and EOP management (manufacturing, use, cleaning), complications, follow-up visits and multidisciplinary care. The frequency and proportions of the responses were statistically analysed.
Results
The questionnaire was addressed to 20 Brazilian and 17 Spanish ocularists, obtaining a response rate of 65% and 64.7%, respectively. 62.5% of respondents were men. The most common cause of anophthalmia in Brazil (69.2%) and Spain (36.4%) is an eye disease (chi square: p = 0.188). Polymethylmethacrylate (PMMA) is the most commonly used material in EOP manufacture (chi square: p = 0.448), and 70.8% reported using customized EOPs (chi square: p = 0.069). Deposits are frequently observed in both countries (chi square: p = 0.157). Changing the prosthesis is recommended after 5 to 10 years by Brazilian ocularists, and after less than 5 years of use by Spanish ocularists (81.8%) (chi square: p = 0.041). Annual follow-up is recommended by Spanish ocularists (45.5%), while semestral (38.5%) and case-dependent (38.5%) follow-up is recommended by Brazilian ocularists (chi square: p = 0.267). Daily cleaning is advocated by 61.5% of Brazilian ocularists and once a month by 45.5% of Spanish ocularists (chi square: p = 0.098), with 75% of ocularists from both countries not recommending EOP removal at night (Fisher´s exact test: p = 0.166). Good communication between ocularists and ophthalmologists was reported by 87.5% of our responders (chi square: p = 0.642).
Conclusion
Although there are no unified protocols on the management of EOPs, Brazilian and Spanish ocularists follow similar guidelines. Differences between countries were the patients´ referral and the prosthesis´ useful life.
Similar content being viewed by others
References
Hatamleh MM, Abbariki M, Alqudah N, Cook AE (2017) Survey of Ocular prosthetics rehabilitation in the United Kingdom, part 1: Anophthalmic patients’ aetiology, opinions, and attitudes. J Craniofac Surg 28:1293–1296. https://doi.org/10.1097/SCS.0000000000003370
Bonaque-González S, Amigó A, Rodríguez-Luna C (2015) Recommendations for post-adaption care of an ocular prosthesis: a review. Contact Lens Anterior Eye 38:397–401. https://doi.org/10.1016/j.clae.2015.06.003
Choudhury M, Banu F, Natarajan S, Kumar A, Padmanabhan TV (2018) A multidisciplinary approach for rehabilitation of enucleated sockets: ocular implants with custom ocular prosthesis. Cureus 10:e2201. https://doi.org/10.7759/cureus.2201
Goiato MC, Bannwart LC, Haddad MF, Dos Santos DM, Alves Pesqueira A, Issamu Miyahara G (2014) Fabrication techniques for ocular prostheses–an overview. Orbit 33:229–233. https://doi.org/10.3109/01676830.2014.881395
Changal N, AlRasheed W, Khandekar R (2020) Ocularists the less known mid eye care professionals and their contribution in eye health care. Saudi J Ophthalmol Off J Saudi Ophthalmol Soc 34:195–197. https://doi.org/10.4103/1319-4534.310403
Baino F, Perero S, Ferraris S, Miola M, Balagna C, Verné E, Vitale-Brovarone C, Coggiola A, Dolcino D, Ferraris D (2014) Biomaterials for orbital implants and ocular prostheses: overview and future prospects. Acta Biomater 10:1064–1087. https://doi.org/10.1016/j.actbio.2013.12.014
Osborn KL, Hettler D (2010) A survey of recommendations on the care of ocular prostheses. Optometry 81:142–145. https://doi.org/10.1097/ICL.0000000000000020
Ho VWM, Hussain RN, Czanner G, Heimann H, Damato BE (2017) Porous versus nonporous orbital implants after enucleation for Uveal melanoma: a randomized study. Ophthal Plast Reconstr Surg 33:452–458. https://doi.org/10.1097/IOP.0000000000000824
Chinnery H, Thompson SBN, Noroozi S, Dyer B, Rees K (2017) Questionnaire study to gain an insight into the manufacturing and fitting process of artificial eyes in children: an ocularist perspective. Int Ophthalmol 37:1175–1183. https://doi.org/10.1007/s10792-016-0383-4
Hintschich C, Baldeschi L (2001) Rehabilitation of anophthalmic patients. Results of a survey. Ophthalmologe 98:74–80. https://doi.org/10.1007/s003470170203
Timothy NH, Freilich DE, Linberg JV (2003) Evisceration versus enucleation from the ocularist’s perspective. Ophthalmic Plast Reconstr Surg 19:417–420. https://doi.org/10.1097/01.IOP.0000096162.94415.98
Goiato MC, Zucolotti BRC, Mancuso DN, Dos Santos DM, Pellizzer EP, Verri FR (2010) Care and cleaning of maxillofacial prostheses. J Craniofac Surg 21:1270–1273. https://doi.org/10.1097/SCS.0b013e3181e1b431
Parr GR, Goldman BM, Rahn AO (1983) Postinsertion care of the ocular prosthesis. J Prosthet Dent 49:220–224. https://doi.org/10.1016/0022-3913(83)90506-1
Pine KR, Sloan BH, Jacobs RJ (2015). Clinical Ocular Prosthetics. Springer Charm, Switzerland
Ocularists training in the United Kingdom. Available from: http://ocularists.net/education-and-training/ocularist-training-in-the-united-kingdom/.
Maxillofacial Prosthetic Rehabilitation MSc, Kings College University, London. Available from: https://www.kcl.ac.uk/study/postgraduate-taught/courses/maxillofacial-prosthetic-rehabilitation-msc/.
National Examining Board of Ocularists (NEBO). Available from: https://neboboard.org/.
Association of European Ocularists. Available from: https://www.aeo2023.com/.
American Society of Ocularists. Available from: https://ocularist.org/.
Ocularists Association of Australia. Available from: http://ocularistsaustralia.com/
Indian Society of Ocularists. Available from: http://www.ocularist.co.in/.
Ocularists Association of Southern Africa. Available from: http://www.oasa.org.za/.
International Anaplastology Association. Aailable from: https://www.anaplastology.org/
International Academy of Ocularistry. Available from: https://www.academyofocularistry.org/
Rokohl AC, Koch KR, Adler W, Trester M, Trester W, Pine NS, Pine KR, Heindl LM (2018) Concerns of anophthalmic patients-a comparison between cryolite glass and polymethyl methacrylate prosthetic eye wearers. Graefes Arch Clin Exp Ophthalmol 256:1203–1208. https://doi.org/10.1007/s00417-018-3942-8
Rokohl AC, Mor JM, Trester M, Koch KR, Heindl LM (2019) Rehabilitation of Anophthalmic patients with prosthetic eyes in germany today—supply possibilities, daily use, complications and psychological aspects. Klin Monbl Augenheilkd 236:54–62. https://doi.org/10.1055/a-0764-4974
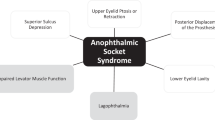
Quaranta-Leoni FM, Fiorino MG, Quaranta-Leoni F, Di Marino M (2021) Anophthalmic socket syndrome: prevalence, impact and management strategies. Clin Ophthalmol 15:3267–3281. https://doi.org/10.2147/OPTH.S325652
Rokohl AC, Trester M, Mor JM, Loreck N, Koch KR, Heindl LM (2019) Customizing a Cryolite glass prosthetic eye. J Vis Exp 31:152. https://doi.org/10.3791/60016
Rokohl AC, Trester M, Mor JM, Pine KR, Heindl LM (2019) Risk of breakage of cryolite glass prosthetic eyes. Graefes Arch Clin Exp Ophthalmol 257:437–438. https://doi.org/10.1007/s00417-018-4155-x
Litwin AS, Worrell E, Roos JCP, Edwards B, Malhotra R (2018) Can we improve the tolerance of an ocular prosthesis by enhancing its surface finish? Ophthal Plast Reconstr Surg 34:130–135. https://doi.org/10.1097/IOP.0000000000000891
Rokohl AC, Adler W, Koch KR, Mor JM, Jia R, Trester M, Pine NS, Pine KR, Heindl LM (2019) Cryolite glass prosthetic eyes-the response of the anophthalmic socket. Graefes Arch Clin Exp Ophthalmol 257:2015–2023. https://doi.org/10.1007/s00417-019-04395-y
Rokohl AC, Koch KR, Trester M, Trester W, Pine KR, Heindl LM (2018) Concerns of Anophthalmic patients wearing Cryolite glass prosthetic eyes. Ophthalmic Plast Reconstr Surg 34(4):369–374. https://doi.org/10.1097/IOP.0000000000001021
Acknowledgements
To all the participants in the survey.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
EM-F and CPB collected data and wrote the manuscript. HS-T and DMZ reviewed material, method and helped with statistics. SAS and AG-F reviewed the whole manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors do not have a personal or family ownership or potential rights to more than 1% of the company or competing company or any interest in marketing any product, drug, instrument, or piece of equipment discussed in the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martinez-Fernandez, E., Pereira Bigheti, C., Sanchez-Tocino, H. et al. Management of external ocular prosthesis by ocularists: results of an online survey conducted in Brazil and Spain. Int Ophthalmol 43, 4297–4304 (2023). https://doi.org/10.1007/s10792-023-02841-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02841-9