Abstract
Purpose
The Corvis Biomechanical Index-Laser Vision Correction (CBI-LVC) is a biomechanical index to detect ectasia in post-refractive surgery patients (PRK, LASIK, SMILE). This study aims to evaluate the distribution of the CBI-LVC in stable patients who underwent Phototherapeutic Keratectomy (PTK) compared to PRK patients.
Methods
Patients who underwent PRK and PTK performed between 2000 and 2018 in Humanitas Research Hospital, Rozzano, Milan, Italy and remained stable for at least four years post-surgery were included. All eyes were examined with the Corvis ST (Oculus, Germany), whose output allows the calculation of the CBI-LVC. The distribution and specificity of the CBI-LVC in the two populations were estimated using a Wilcoxon Mann–Whitney test and compared.
Results
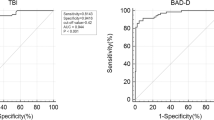
175 eyes of 148 patients were included (85 eyes of 50 PTK patients and 90 eyes of 90 PRK patients). The distribution of CBI-LVC in the two groups showed a minor difference, with a median value in PRK patients of 0.000 (95% CI 0.000; 0.002) and 0.008 (95% CI 0.000; 0.037) in PTK patients (Mann–Whitney U test p = 0.023). The statistical analysis showed that the CBI-LVC provided a specificity of 92.22% in the PRK group, while in the PTK group it was 82.35%. Nevertheless, this difference was not statistically significant (Chi-squared test with Yates, p = 0.080).
Conclusion
CBI-LVC provided similar specificity in stable PTK patients compared to those who underwent PRK. These results suggest that the CBI-LVC could be a useful tool to aid corneal surgeons in managing PTK patients.


Similar content being viewed by others
References
Spadea L, Cantera E, Cortes M, Conocchia NE, Stewart CW (2012) Corneal ectasia after myopic laser in situ keratomileusis: a long-term study. Clin Ophthalmol 6:1801–1813. https://doi.org/10.2147/OPTH.S37249
Woodward MA et al (2008) Visual rehabilitation and outcomes for ectasia after corneal refractive surgery. J Cataract Refract Surg 34:383–388. https://doi.org/10.1016/j.jcrs.2007.10.025
Seiler T, Quurke AW (1998) Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg 24:1007–1009. https://doi.org/10.1016/s0886-3350(98)80057-6
Roszkowska AM, Sommario MS, Urso M, Aragona P (2017) Post photorefractive keratectomy corneal ectasia. Int J Ophthalmol 10:315–317. https://doi.org/10.18240/ijo.2017.02.22
Moshirfar M et al (2017) Ectasia following small-incision lenticule extraction (SMILE): a review of the literature. Clin Ophthalmol 11:1683–1688. https://doi.org/10.2147/OPTH.S147011
Ambrosio R Jr (2019) Post-LASIK ectasia: twenty years of a conundrum. Semin Ophthalmol 34:66–68. https://doi.org/10.1080/08820538.2019.1569075
Wolle MA, Randleman JB, Woodward MA (2016) Complications of refractive surgery: ectasia after refractive surgery. Int Ophthalmol Clin 56:127–139. https://doi.org/10.1097/IIO.0000000000000102
Randleman JB, Woodward M, Lynn MJ, Stulting RD (2008) Risk assessment for ectasia after corneal refractive surgery. Ophthalmology 115:37–50. https://doi.org/10.1016/j.ophtha.2007.03.073
Santhiago MR (2016) Percent tissue altered and corneal ectasia. Curr Opin Ophthalmol 27:311–315. https://doi.org/10.1097/ICU.0000000000000276
Giri P, Azar DT (2017) Risk profiles of ectasia after keratorefractive surgery. Curr Opin Ophthalmol 28:337–342. https://doi.org/10.1097/ICU.0000000000000383
Esporcatte LPG et al (2020) Biomechanical diagnostics of the cornea. Eye Vis (Lond). https://doi.org/10.1186/s40662-020-0174-x
Ambrosio R Jr et al (2017) Corneal Biomechanics in ectatic diseases: refractive surgery implications. Open Ophthalmol J 11:176–193. https://doi.org/10.2174/1874364101711010176
Ambrosio R Jr et al (2016) Ectasia detection by the assessment of corneal biomechanics. Cornea 35:e18-20. https://doi.org/10.1097/ICO.0000000000000875
Salomão MQ et al (2020) The role of corneal biomechanics for the evaluation of ectasia patients Int. J Environ Res Public Health. https://doi.org/10.3390/ijerph17062113
Vinciguerra R, Ambrosio R, Wang Y et al (2023) Detection of keratoconus with a new corvis biomechanical index optimized for chinese populations. Am J Ophthalmol 252:182–187. https://doi.org/10.1016/j.ajo.2023.04.002
Ambrósio R Jr, Machado AP, Leão E et al (2023) Optimized artificial intelligence for enhanced ectasia detection using scheimpflug-based corneal tomography and biomechanical data. Am J Ophthalmol 251:126–142. https://doi.org/10.1016/j.ajo.2022.12.016
Ambrosio R Jr et al (2017) Integration of scheimpflug-based corneal tomography and biomechanical assessments for enhancing ectasia detection. J Refract Surg 33:434–443. https://doi.org/10.3928/1081597X-20170426-02
Vinciguerra R et al (2016) Detection of keratoconus with a new biomechanical index. J Refract Surg 32:803–810. https://doi.org/10.3928/1081597X-20160629-01
Vinciguerra R, Ambrosio R Jr, Roberts CJ, Azzolini C, Vinciguerra P (2017) Biomechanical characterization of subclinical keratoconus without topographic or tomographic abnormalities. J Refract Surg 33:399–407. https://doi.org/10.3928/1081597X-20170213-01
Wang B et al (2016) Comparison of the change in posterior corneal elevation and corneal biomechanical parameters after small incision lenticule extraction and femtosecond laser-assisted LASIK for high myopia correction. Cont Lens Anterior Eye 39:191–196. https://doi.org/10.1016/j.clae.2016.01.007
Vinciguerra R et al (2021) Detection of postlaser vision correction ectasia with a new combined biomechanical index. J Cataract Refract Surg 47:1314–1318. https://doi.org/10.1097/j.jcrs.0000000000000629
Nagpal R et al (2020) Phototherapeutic keratectomy. Surv Ophthalmol 65:79–108. https://doi.org/10.1016/j.survophthal.2019.07.002
Rapuano CJ (1996) Excimer laser phototherapeutic keratectomy. Int Ophthalmol Clin 36:127–136. https://doi.org/10.1097/00004397-199603640-00017
Miyata K, Takahashi T, Tomidokoro A, Ono K, Oshika T (2001) Iatrogenic keratectasia after phototherapeutic keratectomy. Br J Ophthalmol 85:247–248. https://doi.org/10.1136/bjo.85.2.238j
Vinciguerra R et al (2016) Influence of pachymetry and intraocular pressure on dynamic corneal response parameters in healthy patients. J Refract Surg 32:550–561. https://doi.org/10.3928/1081597X-20160524-01
Roberts CJ et al (2017) Introduction of two novel stiffness parameters and interpretation of air puff-induced biomechanical deformation parameters with a dynamic scheimpflug analyzer. J Refract Surg 33:266–273. https://doi.org/10.3928/1081597X-20161221-03
Dupps WJ Jr, Wilson SE (2006) Biomechanics and wound healing in the cornea. Exp Eye Res 83:709–720. https://doi.org/10.1016/j.exer.2006.03.015
Feizi S, Karjou Z, Abbasi H, Javadi MA, Azari AA (2020) Characterization of In Vivo biomechanical properties in macular corneal dystrophy. Am J Ophthalmol 215:8–13. https://doi.org/10.1016/j.ajo.2020.03.003
Marcos-Fernandez MA, Tabernero SS, Herreras JM, Galarreta DJ (2018) Impact of herpetic stromal immune keratitis in corneal biomechanics and innervation. Graefes Arch Clin Exp Ophthalmol 256:155–161. https://doi.org/10.1007/s00417-017-3826-3
Funding
No fundings.
Author information
Authors and Affiliations
Contributions
R.V. and G.C. wrote the manuscript, A.E, R.A, A.E and B.L revised and improved the manuscript, P.V supervised the all project and revised the initial and final manuscript
Corresponding author
Ethics declarations
Conflict of interest
Riccardo Vinciguerra, Paolo Vinciguerra, Renato Ambrósio Jr., and Ahmed Elsheikh are consultants for OCULUS Optikgeräte GmbH. OCULUS Optikgeräte GmbH did not take part in the design, analysis, or interpretation of the results. Except where noted, none of the remaining authors have financial interests to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vinciguerra, R., Cancian, G., Ambrósio, R. et al. Assessment of the specificity of corvis biomechanical index-laser vision correction (CBI-LVC) in stable corneas after phototherapeutic keratectomy. Int Ophthalmol 43, 4289–4295 (2023). https://doi.org/10.1007/s10792-023-02840-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02840-w