Abstract
Background
Femtosecond laser-assisted in situ keratomileusis (FS-LASIK) with accelerated corneal crosslinking (FS-LASIK Xtra) is a recent procedure to achieve safer corneal ablation in myopic patients with borderline corneal thickness. Despite its well-accepted effectiveness, the development of remarkable interface haze is a potential concern but has rarely been reported and discussed.
Methods
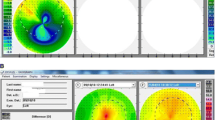
We report for the first time a case series of 11 eyes of 7 patients who developed typical interface haze 1–3 months after FS-LASIK Xtra for the correction of myopia with astigmatism, with intensity grades ranging from 0.5 + to 3 + at the time of onset.
Results
The preclinical spherical diopters of the 7 patients ranged from − 2.25 D to − 9.25 D and cylindrical diopters ranged from − 0.25 D to − 2.50 D. The haze tended to be self-limiting, and topical anti-inflammatory therapy was given to moderate and severe cases, who responded well to treatment.
Conclusions
The development of clinically significant interface haze is a relatively rare complication after FS-LASIK Xtra but tends to have a higher incidence and intensity compared to conventional stromal surgery such as FS-LASIK. Timely treatment and close follow-up are essential to patients undertaking FS-LASIK Xtra.




Similar content being viewed by others
References
Tomita M (2016) Combined laser in-situ keratomileusis and accelerated corneal cross-linking: an update. Curr Opin Ophthalmol 27(4):304–310. https://doi.org/10.1097/ICU.0000000000000281
Xu W, Tao Y, Wang L et al (2017) Evaluation of biomechanical changes in myopia patients with unsatisfactory corneas after femto second-laser in situ keratomileusis (FS-LASIK) concurrent with accelerated corneal collagen cross-linking using corvis-ST: two-year follow-up results. Med Sci Monit 23:3649–3656. https://doi.org/10.12659/MSM.905493
Zhao L, Yin Y, Hu T et al (2023) Comprehensive management of post-LASIK ectasia: from prevention to treatment. Acta Ophthalmol. https://doi.org/10.1111/aos.15636
Dong R, Zhang Y, Yuan Y et al (2022) A prospective randomized self-controlled study of LASIK combined with accelerated cross-linking for high myopia in Chinese: 24-month follow-up. BMC Ophthalmol 22(1):280. https://doi.org/10.1186/s12886-022-02491-y
Tan J, Lytle GE, Marshall J (2015) Consecutive laser in situ keratomileusis and accelerated corneal crosslinking in highly myopic patients: preliminary results. Eur J Ophthalmol 25(2):101–107. https://doi.org/10.5301/ejo.5000543
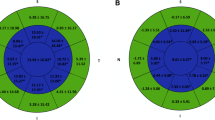
Zhang J, Chen T, Wang J et al (2022) Laser in Situ Keratomileusis (LASIK) combined with prophylactic corneal cross-linking for correction of myopia: regional analysis of corneal morphology. Ophthalmol Ther 11(4):1423–1439. https://doi.org/10.1007/s40123-022-00510-1
Tamayo GE (2012) Predictable visual outcomes with accelerated corneal cross-linking concurrent with laser in situ keratomileusis. J Cataract Refract Surg 38(12):2206. https://doi.org/10.1016/j.jcrs.2012.10.023
Lu NJ, Hafezi F, Torres-Netto EA et al (2023) Effect of fluence levels on prophylactic corneal cross-linking for laser in situ keratomileusis and transepithelial photorefractive keratectomy. Acta Ophthalmol 101(2):e185–e196. https://doi.org/10.1111/aos.15230
Lim L, Lim EWL, Rosman M et al (2020) Three-year outcomes of simultaneous accelerated corneal crosslinking and femto-lasik for the treatment of high myopia in asian eyes. Clin Ophthalmol 14:2865–2872. https://doi.org/10.2147/OPTH.S260088
Fantes FE, Hanna KD, Waring Iii GO et al (1990) Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol 108(5):665–675
Charpentier S, Keilani C, Maréchal M et al (2021) Corneal haze post photorefractive keratectomy. J Fr Ophtalmol 44(9):1425–1438. https://doi.org/10.1016/j.jfo.2021.05.006
Torricelli AA, Santhanam A, Wu J et al (2016) The corneal fibrosis response to epithelial-stromal injury. Exp Eye Res 142:110–118. https://doi.org/10.1016/j.exer.2014.09.012
Wilson SE, Torricelli AAM, Marino GK (2020) Corneal epithelial basement membrane: structure, function and regeneration. Exp Eye Res 194:108002. https://doi.org/10.1016/j.exer.2020.108002
Hafezi F, Hillen M, Kollros L et al (2022) Corneal cross-linking in thin corneas: from origins to state of the art. Eur Ophthalmic Rev 16(1):13–16. https://doi.org/10.17925/USOR.2022.16.1.13
Greenstein SA, Hersh PS (2021) Corneal crosslinking for progressive keratoconus and corneal ectasia: summary of US multicenter and subgroup clinical trials. Transl Vis Sci Technol 10(5):13. https://doi.org/10.1167/tvst.10.5.13
Salomão MQ, Chaurasia SS, Sinha-Roy A et al (2011) Corneal wound healing after ultraviolet-A/riboflavin collagen cross-linking: a rabbit study. J Refract Surg 27(6):401–407. https://doi.org/10.3928/1081597x-20101201-02
Lim EWL, Lim L (2019) Review of laser vision correction (LASIK, PRK and SMILE) with simultaneous accelerated corneal crosslinking–long-term results. Curr Eye Res 44(11):1171–1180. https://doi.org/10.1080/02713683.2019.1656749
Marino GK, Santhiago MR, Torricelli AAM et al (2016) Corneal molecular and cellular biology for the refractive surgeon: the critical role of the epithelial basement membrane. J Refract Surg 32(2):118–125. https://doi.org/10.3928/1081597X-20160105-02
Kymionis GD, Karavitaki AE, Portaliou DM et al (2010) Interface haze formation after ultra thin flap laser in situ keratomileusis. Ophthalmic Surg Lasers Imaging. https://doi.org/10.3928/15428877-20100215-66
Esquenazi S, He J, Li N et al (2010) Immunofluorescence of rabbit corneas after collagen cross-linking treatment with riboflavin and ultraviolet A. Cornea 29(4):412–417. https://doi.org/10.1097/ICO.0b013e3181bdf1cc
Covre J, Cristovam P, Loureiro R et al (2013) Evaluation of the riboflavin and ultraviolet light effect on keratocytes cultivated in vitro. Investig Ophthalmol Vis Sci 54(15):1021
Margo JA, Munir WM (2016) Corneal haze following refractive surgery: A review of pathophysiology, incidence, prevention, and treatment. Int Ophthalmol Clin 56(2):111–125. https://doi.org/10.1097/IIO.0000000000000112
Furukawa H, Nakayasu K, Gotoh T et al (1997) Effect of topical tranilast and corticosteroids on subepithelial haze after photorefractive keratectomy in rabbits. J Refract Surg 13(5):S457–S458
Pakbin M, Khabazkhoob M, Pakravan M et al (2020) Duration of topical steroid application after photorefractive keratectomy with mitomycin C. J Cataract Refract Surg 46(4):622–632. https://doi.org/10.1097/j.jcrs.0000000000000060
Gartry DS, Muir MGK, Lohmann CP et al (1992) The effect of topical corticosteroids on refractive outcome and corneal haze after photorefractive keratectomy: a prospective, randomized, double-blind trial. Arch Ophthalmol 110(7):944–952
Aras C, Özdamar A, Aktunç R et al (1998) The effects of topical steroids on refractive outcome and corneal haze ,thickness, and curvature after photorefractive keratectomy with a 6.0-mm ablation diameter. Ophthalmic Surg Lasers 29(8):621–627
Soya K, Obata H, Amano S et al (1997) Effects of topical corticosteroids on subepithelial haze after excimer laser corneal surgery objective and quantitative method for evaluating haze. J Jpn Ophthalmol Soc 101(2):152–157
Zhang X, Shen Z, Sun H et al (2023) Efficacy and safety of loteprednol etabonate versus fluorometholone in the treatment of patients after corneal refractive surgery: a meta-analysis. Int Ophthalmol. https://doi.org/10.1007/s10792-023-02646-w
Funding
This work was supported by the Science & Technology Department of Sichuan Province (China) funding project (No. 2021YFS0221, No.2023YFS0179), 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (No.2022HXFH032, ZYJC21058, 2021-023, 2022-014), and the Postdoctoral Research Funding of West China Hospital (No. 2020HXBH044).
Author information
Authors and Affiliations
Contributions
All authors conducted clinical observation and the literature search. LW wrote the manuscript. HY the surgery and provided supervision. HY and KM revised the manuscript
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Human rights statement
The studies involving human participants were reviewed and approved by the Ethics Committee of West China Hospital.
Informed consent
The patients whose case reports are given in this manuscript provided their written informed consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yin, H., Wang, L., Gong, R. et al. Development of interface haze after femtosecond laser-assisted in situ keratomileusis with accelerated corneal crosslinking: a case series. Int Ophthalmol 43, 4333–4342 (2023). https://doi.org/10.1007/s10792-023-02800-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02800-4