Abstract
Purpose
To evaluate the efficacy of micropulse transscleral cyclophotocoagulation (MP-TSCPC) considering different characteristics: glaucoma subtypes and lens status.
Methods
A retrospective case-series study was designed to evaluate intraocular pressure (IOP), and the number of IOP-lowering medications, used by glaucoma patients treated with MP-TSCPC between 2016 and 2019. Cases had a follow-up period of 12 months. Achieving an IOP reduction higher than 20%, or the decrease of at least one IOP-lowering medication, was considered a successful outcome. The same population was analyzed by classifying them in two groups as: glaucoma subtypes and lens status. The baseline spherical equivalent (SE) was also calculated for considering association with the achieved IOP.
Results
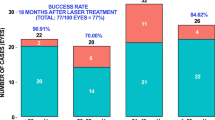
A total of 86 eyes were included. In most cases, IOP and IOP-lowering medications were decreased with a statistically significant difference (p < 0.0001), and all of them had a successful outcome. The percentage of IOP drop oscillated between 25.9% (open-angle glaucoma sub-group) and 37.5% (pseudoexfoliative glaucoma sub-group), 12 months after surgery. The difference between the groups was not statistically significant (p 0.20 and 0.32 for glaucoma subtypes and lens status, respectively). The Pearson’s coefficient obtained was low for the SE and IOP association, at the 12 -month postoperative mark (− 0.009; p < 0.001).
Conclusions
The MP-TSCPC treatment was successful in decreasing IOP and IOP-lowering medications, in different glaucoma subtypes. Differences between groups (glaucoma subtypes, phakic and pseudophakic eyes) were not statistically significant. No association was found between the SE and the IOP achieved value after MS-TSCPC treatment.






Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
XLMiner Analysis Toolpak Frontline Systems Inc. was used. It is a free software to perform statistical analysis in Google Sheets.
References
Jiang Y, Ondeck (2020) A Review of new medications and future directions of medical therapies in glaucoma. Semin Ophthalmol 35:280–286
Cvenkel B, Kolko M (2020) Current medical therapy and future trends in the management of glaucoma treatment. J Ophthalmol 2020:6138132. https://doi.org/10.1155/2020/6138132
Garg A, Gazzard G (2020) Treatment choices for newly diagnosed primary open angle and ocular hypertension patients. Eye (Lond) 34:60–71
Lee RMH, Bouremel Y, Eames I (2020) Translating minimally invasive glaucoma surgery devices. Clin Transl Sci 13:14–25
Do AT, Parikh H, Panarelli JF (2020) Subconjunctival microinvasive glaucoma surgeries: an update on the Xen gel stent and the PreserFlo MicroShunt. Curr Opin Ophthalmol 31:132–138
Mistlberger A, Liebmann JM, Tschiderer H, Ritch R, Ruckhofer J, Grabner G (2001) Diode laser transscleral cyclophotocoagulation for refractory glaucoma. J Glaucoma 10:288–293. https://doi.org/10.1097/00061198-200108000-00008
Ishida K (2013) Update on results and complications of cyclophotocoagulation. Curr Opin Ophthalmol 24:102–110
Tan AM, Chockalingam M, Aquino MC, Lim ZI, See JL, Chew PT (2010) Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Exp Ophthalmol 38:266–272
Aquino MC, Barton K, Tan AM, Li X, Loon SC, Chew PT (2015) Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Exp Ophthalmol 43:40–46
Emanuel ME, Grover DS, Fellman RL, Godfrey DG, Smith O, Butler MR et al (2017) Micropulse cyclophotocoagulation: initial results in refractory glaucoma. J Glaucoma 26:726–729
Williams AL, Moster MR, Rahmatnejad K, Resende AF, Horan T, Reynolds M et al (2018) Clinical efficacy and safety profile of micropulse transscleral cyclophotocoagulation in refractory glaucoma. J Glaucoma 27:445–449
Sanchez FG, Lerner F, Sampaolesi J, Noecker R, Becerra N, Iribarren G et al (2018) Efficacy and safety of micropulse® transscleral cyclophotocoagulation in glaucoma. Arch Soc Esp Oftalmol 93:573–579
Zaarour K, Abdelmassih Y, Arej N, Cherfan G, Tomey KF, Khoueir Z (2019) Outcomes of micropulse transscleral cyclophotocoagulation in uncontrolled glaucoma patients. J Glaucoma 28:270–275
Logioco C, Perrone LD, Caruso D, Albertazzi R, Valvecchia G, Zanutigh V (2020) Assessment of efficacy and safety of micropulse diode laser treatment in glaucoma: one year follow-up. Arch Soc Esp Oftalmol 95:327–333
de Crom RMPC, Slangen CGMM, Kujovic-Aleksov S, Webers CAB, Berendschot TTJM, Beckers HJM (2020) Micropulse trans-scleral cyclophotocoagulation in patients With glaucoma: 1 and 2-year treatment outcomes. J Glaucoma 29:794–798
Liu GJ, Mizukawa A, Okisaka S (1994) Mechanism of intraocular pressure decrease after contact transscleral continuous-wave Nd:YAG laser cyclophotocoagulation. Ophthalmic Res 26:65–79
Tsujisawa T, Ishikawa H, Uga S, Asakawa K, Kono Y, Mashimo K et al (2020) Morphological changes and potential mechanisms of intraocular pressure reduction after micropulse transscleral cyclophotocoagulation in rabbits. Ophthalmic Res. https://doi.org/10.1159/000510596
Sarrafpour S, Saleh D, Ayoub S, Radcliffe NM (2019) Micropulse transscleral cyclophotocoagulation: a look at long-term effectiveness and outcomes. Ophthalmol Glaucoma 2:167–171
Masis Solano M, Lin SC (2018) Cataract, phacoemulsification and intraocular pressure: Is the anterior segment anatomy the missing piece of the puzzle? Prog Retin Eye Res 64:77–83. https://doi.org/10.1016/j.preteyeres.2018.01.003
Wang SY, Azad AD, Lin SC, Hernandez-Boussard T, Pershing S (2020) Intraocular pressure changes after cataract surgery in patients with and without glaucoma: an informatics-based approach. Ophthalmol Glaucoma 3(5):343–349. https://doi.org/10.1016/j.ogla.2020.06.002
Grødum K, Heijl A, Bengtsson B (2001) Refractive error and glaucoma. Acta Ophthalmol Scand 79:560–566
Marcus MW, de Vries MM, Junoy Montolio FG, Jansonius NM (2001) Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology 118:1989-1994.e2
Qiu M, Wang SY, Singh K, Lin SC (2013) Association between myopia and glaucoma in the United States population. Invest Ophthalmol Vis Sci 54:830–835
Shen L, Melles RB, Metlapally R, Barcellos L, Schaefer C, Risch N et al (2016) The association of refractive error with glaucoma in a multiethnic population. Ophthalmology 123:92–101
Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S (2017) Glaucoma. Lancet 390(10108):2183–2193. https://doi.org/10.1016/S0140-6736(17)31469-1
Wang L, Huang W, Huang S, Zhang J, Guo X, Friedman DS et al (2019) Ten-year incidence of primary angle closure in elderly Chinese: the Liwan Eye Study. Br J Ophthalmol 103:355–360
Varikuti VNV, Shah P, Rai O, Chaves AC, Miranda A, Lim BA et al (2019) Outcomes of micropulse transscleral cyclophotocoagulation in eyes with good central vision. J Glaucoma 28:901–905
Vig N, Ameen S, Bloom P, Crawley L, Normando E, Porteous A et al (2020) Micropulse transscleral cyclophotocoagulation: initial results using a reduced energy protocol in refractory glaucoma. Graefes Arch Clin Exp Ophthalmol 258:1073–1079
Laruelle G, Pourjavan S, Janssens X, Marinescu-George C, Boustani G (2021) Real-life experience of micropulse transscleral cyclophotocoagulation (MP-TSCPC) in advanced and uncontrolled cases of several glaucoma types: a multicentric retrospective study. Int Ophthalmol 41(10):3341–3348. https://doi.org/10.1007/s10792-021-01896-w
Acknowledgments
The authors would like to acknowledge Rodrigo M. Torres M.D. Ph.D. for his scientific advice.
Funding
None; this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by VZ, LDP, GGC, FP, GV, and CL. The first draft of the manuscript was written by VZ and CL, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethical approval
The study was conducted following the Helsinki tenets in a private clinic in Buenos Aires (Centro de Ojos Quilmes), Argentina, after the Institutional Review Board approved the study protocol.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zanutigh, V., Perrone, L.D., Gómez-Caride, G. et al. Success rate in micropulse diode laser treatment with regard to lens status, refractive errors, and glaucoma subtypes. Int Ophthalmol 43, 2407–2417 (2023). https://doi.org/10.1007/s10792-023-02640-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02640-2