Abstract
Purpose
To investigate the relationship between the development of corrected 1-year-old refraction values and risk factors in preterm infants who underwent laser photocoagulation (LPC) therapy for retinopathy of prematurity (ROP).
Methods
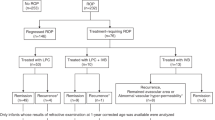
The ophthalmic examination findings of preterm neonates who had developed Type I ROP and received LPC therapy were evaluated retrospectively. The association between spherical equivalent (SE) values and clinical findings were analyzed by using multivariable linear regression analysis.
Results
The study included 157 eyes of 80 neonates with a mean birth week of 27.1 ± 2.2 weeks (23 to 32 weeks) and a mean birth weight of 995 ± 273 g (565 to 1760 g). The treatments were administered on an average of 36.8 ± 2.7 (32 to 45 weeks) postmenstrual age. LPC treatment was applied bilaterally to 77 of the 80 neonates included in the study, and unilaterally to 3 of them. The mean ± standard deviation of the SE value was 0.31 ± 1.89 diopters (D) (− 8.00 to 4.63 D) according to the results of the 1-year corrected age refraction examination. In univariate analysis, no significant association between GA, BW, and ROP zone and SE value, while the number of laser spots (ß = − 0.27 ± 0.00 D, p = 0.00) and stage 3 ROP (ß = − 0.29 ± 0.37 D, p = 0.00) were significantly associated with the SE value. In multivariable linear regression analysis, a significant association between number of laser spot, stage 3 ROP and SE value (ß = − 0.25 ± 0.00 D, p = 0.01 for number of laser spot, ß = − 0.28 ± 0.36 D, p = 0.00 for stage 3 ROP).
Conclusion
In conclusion, this study supports that stage of ROP and the number of laser spots count applied in photocoagulation treatment for ROP is significantly correlated with degree of myopia (p < 0.05).

Similar content being viewed by others
References
Hartnett ME (2017) Advances in understanding and management of retinopathy of prematurity. Surv Ophthalmol 62:257–276. https://doi.org/10.1016/j.survophthal.2016.12.004
Gaber R, Sorour OA, Sharaf AF, Saad HA (2021) Incidence and risk factors for retinopathy of prematurity (ROP) in biggest neonatal intensive care unit in Itay Elbaroud City, Behera Province. Egypt Clin Ophthalmol 15:3467–3471. https://doi.org/10.2147/OPTH.S324614
Al-Qahtani B, Al-Otaibi M, Alabdulajabbar K, Selayem NB, Alshehri W, Omair A et al (2019) Retinopathy of prematurity incidence and risk factors in a tertiary hospital in Riyadh, Saudi Arabia. Middle East Afr J Ophthalmol 26:235–239. https://doi.org/10.4103/meajo.MEAJO_131_18
Dhingra D, Katoch D, Dutta S, Samanta R, Aggarwal K, Dogra MR (2019) Change in the incidence and severity of retinopathy of prematurity (ROP) in a neonatal intensive care unit in Northern India after 20 years: comparison of two similar prospective cohort studies. Ophthalmic Epidemiol 26:169–174. https://doi.org/10.1080/09286586.2018.1562082
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S et al (2015) Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 314:1039–1051. https://doi.org/10.1001/jama.2015.10244
Shah PK, Prabhu V, Karandikar SS, Ranjan R, Narendran V, Kalpana N (2016) Retinopathy of prematurity: past, present and future. World J Clin Pediatr 5:35–46. https://doi.org/10.5409/wjcp.v5.i1.35
Kim J, Kim SJ, Chang YS, Park WS (2014) Combined intravitreal bevacizumab injection and zone I sparing laser photocoagulation in patients with zone I retinopathy of prematurity. Retina 34:77–82. https://doi.org/10.1097/IAE.0b013e318296e26d
Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR (2015) Outcomes after intravitreal bevacizumab versus laser photocoagulation for retinopathy of prematurity: a 5-year retrospective analysis. Ophthalmology 122:1008–1015. https://doi.org/10.1016/j.ophtha.2014.12.017
Mintz-Hittner HA, Kennedy KA, Chuang AZ (2011) Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 364:603–615. https://doi.org/10.1056/NEJMoa1007374
Good WV (2004) Final results of the early treatment for retinopathy of prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc 102:233–248
Fielder AR, Quinn GE (1997) Myopia of prematurity: nature, nurture, or disease? Br J Ophthalmol 81:2–3. https://doi.org/10.1136/bjo.81.1.2
Davitt BV, Dobson V, Good WV, Hardy RJ, Quinn GE, Siatkowski RM et al (2005) Prevalence of myopia at 9 months in infants with high-risk prethreshold retinopathy of prematurity. Ophthalmology 112:1564–1568. https://doi.org/10.1016/j.ophtha.2005.03.025
Dhawan A, Dogra M, Vinekar A, Gupta A, Dutta S (2008) Structural sequelae and refractive outcome after successful laser treatment for threshold retinopathy of prematurity. J Pediatr Ophthalmol Strabismus 45:356–361. https://doi.org/10.3928/01913913-20081101-02
Yang CS, Wang AG, Shih YF, Hsu WM (2013) Long-term biometric optic components of diode laser-treated threshold retinopathy of prematurity at 9 years of age. Acta Ophthalmol 91:e276-282. https://doi.org/10.1111/aos.12053
Chan-Ling T, Gole GA, Quinn GE, Adamson SJ, Darlow BA (2018) Pathophysiology, screening and treatment of ROP: a multi-disciplinary perspective. Prog Retin Eye Res 62:77–119. https://doi.org/10.1016/j.preteyeres.2017.09.002
Geloneck MM, Chuang AZ, Clark WL, Hunt MG, Norman AA, Packwood EA et al (2014) Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. JAMA Ophthalmol 132:1327–1333. https://doi.org/10.1001/jamaophthalmol.2014.2772
Harder BC, Schlichtenbrede FC, von Baltz S, Jendritza W, Jendritza B, Jonas JB (2013) Intravitreal bevacizumab for retinopathy of prematurity: refractive error results. Am J Ophthalmol 155(1119–1124):e1111. https://doi.org/10.1016/j.ajo.2013.01.014
Gunay M, Celik G, Gunay BO, Aktas A, Karatekin G, Ovali F (2015) Evaluation of 2-year outcomes following intravitreal bevacizumab (IVB) for aggressive posterior retinopathy of prematurity. Arq Bras Oftalmol 78:300–304. https://doi.org/10.5935/0004-2749.20150079
Houston SK, Wykoff CC, Berrocal AM, Hess DJ, Murray TG (2013) Laser treatment for retinopathy of prematurity. Lasers Med Sci 28:683–692. https://doi.org/10.1007/s10103-011-1021-z
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A et al (2021) International classification of retinopathy of prematurity, third edition. Ophthalmology 128:51–68. https://doi.org/10.1016/j.ophtha.2021.05.031
Katoch D, Sanghi G, Dogra MR, Beke N, Gupta A (2011) Structural sequelae and refractive outcome 1 year after laser treatment for type 1 prethreshold retinopathy of prematurity in Asian Indian eyes. Indian J Ophthalmol 59:423–426. https://doi.org/10.4103/0301-4738.86306
Inoue T, Asaoka R, Hashimoto Y, Kitamoto K, Kitano M, Fujita A et al (2021) Does the number of laser applications for ROP treatment influence the degree of myopia? Graefes Arch Clin Exp Ophthalmol 259:317–322. https://doi.org/10.1007/s00417-020-04946-8
Mori Y, Arima M, Ueda E, Fujiwara K, Seki E, Nakama T et al (2021) Risk factors for myopia at 1-year corrected age following laser photocoagulation for retinopathy of prematurity. Eye (Lond) 35:2820–2825. https://doi.org/10.1038/s41433-020-01321-z
Pennefather PM, Clarke MP, Strong NP, Cottrell DG, Fritz S, Tin W (1995) Ocular outcome in children born before 32 weeks gestation. Eye (Lond) 9:26–30
Lok JYC, Yip WWK, Luk ASW, Chin JKY, Lau HHW, Young AL (2018) Visual outcome and refractive status in first 3 years of age in preterm infants suffered from laser-treated Type 1 retinopathy of prematurity (ROP): a 6-year retrospective review in a tertiary centre in Hong Kong. Int Ophthalmol 38:163–169. https://doi.org/10.1007/s10792-016-0439-5
Huo L, Qi Y, Zhao S (2021) Refractive errors and risk factors for myopia in infants aged 1–18 months in Tianjin. China BMC Ophthalmol 21:403. https://doi.org/10.1186/s12886-021-02172-2
Varghese RM, Sreenivas V, Puliyel JM, Varughese S (2009) Refractive status at birth: its relation to newborn physical parameters at birth and gestational age. PLoS ONE 4:e4469. https://doi.org/10.1371/journal.pone.0004469
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EKY and CK. The first draft of the manuscript was written by EKY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Health Science (2022/06)
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kıran Yenice, E., Kara, C. Development of myopia in laser-treated ROP infants: prematurity or laser photocoagulation?. Int Ophthalmol 43, 1453–1458 (2023). https://doi.org/10.1007/s10792-022-02540-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02540-x