Abstract
Purpose
To evaluate the four measurement approaches on the determination of effective optical zone (EOZ) using Scheimpflug tomography after small-incision lenticule extraction surgery in eyes with high myopia.
Setting
Corneal refractive surgery conducted in an eye hospital in southern China.
Design
This is a retrospective cohort study.
Methods
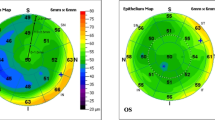
In total, 74 subjects were recruited. EOZ was measured at 3 months postoperatively using vertex-based (EOZV), pupil-based (EOZP), 4 mm-ring-based total corneal refraction method (EOZ4) and tangential curvature difference map method (EOZD), and their consistencies were compared. EOZs and planned optical zone (POZ) were compared and analyzed with eccentricity, ablation degree (AD) and total corneal aberrations.
Results
At 3 months after surgery, the mean root mean square of ΔHOA, ΔComa, ΔTrefoil and ΔSA were 0.53 ± 0.27 μm, 0.36 ± 0.20 μm, 0.01 ± 0.84 μm and 0.16 ± 0.14 μm, respectively. EOZV, EOZP, EOZ4 and EOZD were 5.87 ± 0.44 mm, 5.85 ± 0.45 mm, 4.78 ± 0.40 mm and 5.29 ± 0.27 mm, respectively, which were significantly smaller than POZ 6.48 ± 0.16 mm. Bland–Altman plots showed a good consistency among the four EOZs. The difference between the EOZV and EOZP was 0.02 mm within the range of clinically acceptable difference. In addition, the eccentricity was positively correlated with ΔHOA, ΔComa and ΔSA.
Conclusions
All 4 measurement approaches demonstrated the reduction of EOZs compared to POZ. The EOZV was the closest to POZ, followed by EOZP. The ΔEOZs showed no significant difference with eccentricity, AD and corneal aberrations.



Similar content being viewed by others
Data availability statement
Data could be available upon request to the corresponding author.
References
Boxer BS, Wachler VuN, Huynh AF, Ayman-Shiaty FEl et al (2002) Evaluation of corneal functional optical zone after laser in situ keratomileusis. J Cataract Refract Surg 28(6):948–953
Tabernero J, Klyce SD, Sarver EJ et al (2007) Functional optical zone of the cornea. Invest Ophthalmol Vis Sci 48(3):1053–1060
Zhang JH, Wang SR, He YX et al (2020) The best optical zone for small-incision lenticule extraction in high myopic patients. J Cataract Refract Surg 46(9):1302–1307
Bueeler M, Mrochen M (2005) Simulation of eye-tracker latency, spot size, and ablation pulse depth on the correction of higher order wavefront aberrations with scanning spot laser systems. J Refract Surg 21:28–36
Bueeler M, Mrochen M, Seiler T (2003) Maximum permissible lateral decentration in aberration-sensing and wavefront-guided corneal ablation. J Cataract Refract Surg 29:257–263
Pidro A, Biscevic A, Pjano MA et al (2019) Excimer lasers in refractive surgery. Acta Inform Med 27(4):278–283
Arba Mosquera S, de Ortueta D, Verma S (2018) Corneal functional optical zone under monocular and binocular assessment. Eye Vis (Lond) 5:3
Dupps WJ, Wilson SE (2006) Biomechanics and wound healing in the cornea. Exp Eye Res 83:709–720
Kling S, Hafezi F (2017) Corneal biomechanics-a review. Ophthalmic Physiol Opt 37:240–252
Roberts CJ (2016) Importance of accurately assessing biomechanics of the cornea. Curr Opin Ophthalmol 27:285–291
Hou J, Lei YL, Zheng XR (2018) Optical zone and effective optical zone after corneal refractive surgery. Int Rev Ophthalmol 42:240–244
Huang J, Zhou X, Qian Y (2019) Decentration following femtosecond laser small incision lenticule extraction (SMILE) in eyes with high astigmatism and its impact on visual quality. BMC Ophthalmol 17(19):151–160
Li M, Zhao J, Miao H et al (2014) Mild decentration measured by a scheimpflug camera and its impact on visual quality following SMILE in the early learning curve. Invest Ophthalmol Vis Sci 55:3886–3892
Verdon W, Bullimore M, Maloney RK (1996) Visual performance after photorefractive keratectomy. A prospective study. Arch Ophthalmol 114(12):1465–1472
Hou J, Wang Y, Lei Y, Zheng X (2018) Comparison of effective optical zone after small-incision lenticule extraction and femtosecond laser–assisted laser in situ keratomileusis for myopia. J Cataract Refract Surg 44:1179–1185
Han T, Shang J, Zhou X, Xu Y, Ang M, Zhou X (2020) Refractive outcomes comparing small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis for high myopia. J Cataract Refract Surg 46:419–427
Wang Y, Ma J (2019) Future developments in smile: higher degree of myopia and hyperopia. Asia Pac J Ophthalmol (Phila) 8:412–416
Klyce SD (2007) Night vision disturbances after corneal refractive surgery. Br J Ophthalmol 91:992–993
Liu Q, Yang X, Lin L et al (2019) Review on centration, astigmatic axis alignment, pupil size and optical zone in SMILE. Asia Pac J Ophthalmol (Phila) 8:385–390
Qazi MA, Pepose JS, Sanderson JP, Mahmoud AM, Roberts CJ (2009) Novel objective method for comparing ablation centration with and without pupil tracking following myopic laser in situ keratomileusis using the bausch & lomb technolas 217A. Cornea 28:616–625
Nepomuceno RL, Boxer Wachler BS, Scruggs R (2005) Functional optical zone after myopic LASIK as a function of ablation diameter. J Cataract Refract Surg 31:379–384
Qian Y, Huang J, Zhou X et al (2015) Corneal power distribution and functional optical zone following small incision lenticule extraction for myopia. J Refract Surg 31(8):532–538
He S, Luo Y, Chen P et al (2022) Prospective, randomized, contralateral eye comparison of functional optical zone, and visual quality after SMILE and Fs-Lasik for high myopia. Transl Vis Sci Technol 11(2):13–24
Fu D, Wang L, Zhou X et al (2018) Functional optical zone after small-incision lenticule extraction as stratified by attempted correction and optical zone. Cornea. 9(37):1110–1117
Ryu IH, Kim BJ, Lee JH et al (2017) Comparison of corneal epithelial remodeling after femtosecond laser-assisted lasik and small incision lenticule extraction (SMILE). J Refract Surg 33(4):250–256
Dupps WJ Jr, Roberts C (2001) Effect of acute biomechanical changes on corneal curvature after photokeratectomy. J Refract Surg 17:658–669
Doane JF, Cavanaugh TB, Durrie DS (1995) Relation of visual symptoms to topographic ablation zone decentration after excimer laser photorefractive keratectomy. Ophthalmology 102(1):42–47. https://doi.org/10.1016/S0161-6420(95)31056-1
Acknowledgements
We would like to express our deepest gratitude to all the participants in this study. This work was supported by the Shantou Medical Health, Science and Technology Project Fund (project code: 190615215268728 to L.S.), China.
Funding
This study was funded by the Shantou Medical Health, Science and Technology Project Fund (project code: 190615215268728 to L.S.), China.
Author information
Authors and Affiliations
Contributions
L.S. and R.Z. conceived and designed the study; H.N.L. and R.J. collected and/or assembled the data; H.N.L. analyzed and interpreted the data and wrote the manuscript; and R.Z., V.J. and T.K.N. critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Ethical approval
The study protocol was approved by the Ethics Committee for Human Medical Research at the Joint Shantou International Eye Center of Shantou University and the Chinese University of Hong Kong.
Informed consent
Informed consent was obtained from all participants in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, L., Lin, HN., Jhanji, V. et al. Changes in effective optical zone after small-incision lenticule extraction in high myopia. Int Ophthalmol 42, 3703–3711 (2022). https://doi.org/10.1007/s10792-022-02367-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02367-6