Abstract
Purpose
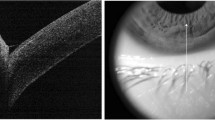
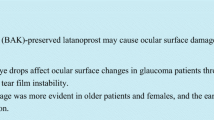
The probability of the coexistence of conjunctivochalasis and pseudoexfoliation syndrome (PES) in the same individual may increase with aging. We investigated the effects of conjunctivochalasis accompanied by PES on the ocular surface (OS) and anterior segment (AS) structures.
Methods
Cases with only conjunctivochalasis were determined as Group 1 (n = 62), cases with conjunctivochalasis accompanied by PES as Group 2 (n = 45), and healthy individuals as Group 3 (n = 56). The OS and AS parameters of the groups were compared.
Results
There were a higher grade-3 conjunctivochalasis rate (17.7% vs. 46.7%, p = 0.039), a greater “mean grade of conjunctivochalasis” value (1.72 ± 0.24 vs. 2.29 ± 0.32, p = 0.036), and a higher “total conjunctivochalasis score” (4.27 ± 1.13 vs. 6.12 ± 1.35, p = 0.025) in Group 2 than in Group 1. Additionally, Group 2 had a shorter tear film break-up time (TBUT) (9.17 ± 2.53 vs. 5.41 ± 1.32, p = 0.010) and a greater OS disease index (OSDI) score (16.28 ± 3.15 vs. 27.36 ± 4.12, p = 0.037) than Group 1. Moreover, both Group 1 and Group 2 had shorter TBUTs (Group 1–3: p = 0.004; Group 2–3: p < 0.001) and greater OSDI scores (Group 1–3: p = 0.042; Group 2–3: p = 0.019) compared to Group 3. The groups’ ocular surface staining scores, Schirmer 1 tests, central corneal thicknesses, keratometries, axial lengths, anterior chamber depths, lens thicknesses, and intraocular pressures were similar (p > 0.05).
Conclusions
To our knowledge, this was the first study comprehensively investigating the effects of conjunctivochalasis accompanied by PES on the OS and AS structures together. We found that conjunctivochalasis might cause the OS disease, while the presence of PES in conjunctivochalasis cases might worsen both the OS disease and conjunctivochalasis findings.

Similar content being viewed by others

References
Marmalidou A, Kheirkhah A, Dana R (2018) Conjunctivochalasis: a systematic review. Surv Ophthalmol 63(4):554–564. https://doi.org/10.1016/j.survophthal.2017.10.010
Gan JY, Li QS, Zhang ZY, Zhang W, Zhang XR (2017) The role of elastic fibers in pathogenesis of conjunctivochalasis. Int J Ophthalmol 10(9):1465–1473. https://doi.org/10.18240/ijo.2017.09.21
Meller D, Li DQ, Tseng SC (2000) Regulation of collagenase, stromelysin, and gelatinase B in human conjunctival and conjunctivochalasis fibroblasts by interleukin-1beta and tumor necrosis factor-alpha. Invest Ophthalmol Vis Sci 41(10):2922–2929
Xiang MH, Zhang XR, Zhang ZY, Li QS, Wang HM, Han ZM, Zhou HM, Jia YL, Chen XX (2017) Expressions of matrix metalloproteinases 1 and 3 and their tissue inhibitors in the conjunctival tissue and fibroblasts cultured from conjunctivochalasis. Int J Ophthalmol 10(4):555–559. https://doi.org/10.18240/ijo.2017.04.09
Meller D, Tseng SC (1998) Conjunctivochalasis: literature review and possible pathophysiology. Surv Ophthalmol 43(3):225–232. https://doi.org/10.1016/s0039-6257(98)00037-x
Li DQ, Meller D, Liu Y, Tseng SC (2000) Overexpression of MMP-1 and MMP-3 by cultured conjunctivochalasis fibroblasts. Invest Ophthalmol Vis Sci 41(2):404–410
Acera A, Vecino E, Duran JA (2013) Tear MMP-9 levels as a marker of ocular surface inflammation in conjunctivochalasis. Invest Ophthalmol Vis Sci 54(13):8285–8291. https://doi.org/10.1167/iovs.13-12235
Schlötzer-Schrehardt U, Naumann GO (2006) Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol 141(5):921–937. https://doi.org/10.1016/j.ajo.2006.01.047
Ghaffari Sharaf M, Amidian S, Rathod V, Crichton A, Damji KF, Wille H, Unsworth LD (2020) Structural polymorphisms in fibrillar aggregates associated with exfoliation syndrome. Sci RepSep 10(1):15860. https://doi.org/10.1038/s41598-020-72737-6
Yildirim Z, Yildirim F, Uçgun NI, Sepici-Dinçel A (2013) The role of the cytokines in the pathogenesis of pseudoexfoliation syndrome. Int J Ophthalmol 6(1):50–53. https://doi.org/10.3980/j.issn.2222-3959.2013.01.10
SarenacVulovic T, Pavlovic S, Lutovac M, Zdravkovic V, Sreckovic S, Zdravkovic N (2019) Regulatory cytokines prescribe the outcome of the inflammation in the process of pseudoexfoliation production. J Chin Med Assoc 82(12):935–940. https://doi.org/10.1097/JCMA.0000000000000214
Zenkel M, Lewczuk P, Jünemann A, Kruse FE, Naumann GO, Schlötzer-Schrehardt U (2010) Proinflammatory cytokines are involved in the initiation of the abnormal matrix process in pseudoexfoliation syndrome/glaucoma. Am J Pathol 176(6):2868–2879. https://doi.org/10.2353/ajpath.2010.090914
Schlötzer-Schrehardt U, Lommatzsch J, Küchle M, Konstas AG, Naumann GO (2003) Matrix metalloproteinases and their inhibitors in aqueous humor of patients with pseudoexfoliation syndrome/glaucoma and primary open-angle glaucoma. Invest Ophthalmol Vis Sci 44(3):1117–1125. https://doi.org/10.1167/iovs.02-0365
Kocabeyoǧlu S, Irkeç M, Orhan M, Mocan MC (2012) Evaluation of the ocular surface parameters in pseudoexfoliation syndrome and conjunctivochalasis. Turk J Ophthalmol 42(5):332–335. https://doi.org/10.4274/tjo.42.392000
Mimura T, Yamagami S, Usui T, Funatsu H, Mimura Y, Noma H, Honda N, Amano S (2009) Changes of conjunctivochalasis with age in a hospital-based study. Am J Ophthalmol 147(1):171-177.e1. https://doi.org/10.1016/j.ajo.2008.07.010
Zhang X, Li Q, Zou H, Peng J, Shi C, Zhou H, Zhang G, Xiang M, Li Y (2011) Assessing the severity of conjunctivochalasis in a senile population: a community-based epidemiology study in Shanghai, China. BMC Public Health 11:198. https://doi.org/10.1186/1471-2458-11-198
You QS, Xu L, Wang YX, Yang H, Ma K, Li JJ, Zhang L, Jonas JB (2013) Pseudoexfoliation: normative data and associations: the Beijing eye study 2011. Ophthalmology 120(8):1551–1558. https://doi.org/10.1016/j.ophtha.2013.01.020
Moghimi S, Mazloumi M, Johari MK, Fard MA, Chen R, Weinreb R, Nouri-Mahdavi K (2017) Comparison of macular choroidal thickness in patients with pseudoexfoliation syndrome to normal control subjects with enhanced depth SD-OCT imaging. J Curr Ophthalmol 29(4):258–263. https://doi.org/10.1016/j.joco.2017.06.009
Mimura T, Iida M, Oshima R, Noma H, Kamei Y, Goto M, Kondo A, Matsubara M (2017) Changes of conjunctivochalasis after cataract surgery via a superior transconjunctival sclerocorneal incision. Int Ophthalmol 37(3):691–700. https://doi.org/10.1007/s10792-016-0328-y
Mimura T, Usui T, Yamagami S, Funatsu H, Noma H, Toyono T, Mori M, Amano S (2011) Relationship between conjunctivochalasis and refractive error. Eye Contact Lens 37(2):71–78. https://doi.org/10.1097/ICL.0b013e31820ca377
Bron AJ, Evans VE, Smith JA (2003) Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 22(7):640–650. https://doi.org/10.1097/00003226-200310000-00008
Eom Y, Lee JS, Keun Lee H, Myung Kim H, Suk Song J (2015) Comparison of conjunctival staining between lissamine green and yellow filtered fluorescein sodium. Can J Ophthalmol 50(4):273–277. https://doi.org/10.1016/j.jcjo.2015.05.007
Begley C, Caffery B, Chalmers R, Situ P, Simpson T, Nelson JD (2019) Review and analysis of grading scales for ocular surface staining. Ocul Surf 17(2):208–220. https://doi.org/10.1016/j.jtos.2019.01.004
Li N, Deng XG, He MF (2012) Comparison of the Schirmer I test with and without topical anesthesia for diagnosing dry eye. Int J Ophthalmol 5(4):478–481. https://doi.org/10.3980/j.issn.2222-3959.2012.04.14
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, Gupta PK, Karpecki P, Lazreg S, Pult H, Sullivan BD, Tomlinson A, Tong L, Villani E, Yoon KC, Jones L, Craig JP (2017) TFOS DEWS II diagnostic methodology report. Ocul Surf 15(3):539–574. https://doi.org/10.1016/j.jtos.2017.05.001
Ozek D, Karaca EE, Evren Kemer O (2020) The effect of conjunctivochalasis detected by anterior segment optical coherence tomography on tear function in an elderly population. Ther Adv Ophthalmol 12:2515841420930876. https://doi.org/10.1177/2515841420930876
Wang Y, Dogru M, Matsumoto Y, Ward SK, Ayako I, Hu Y, Okada N, Ogawa Y, Shimazaki J, Tsubota K (2007) The impact of nasal conjunctivochalasis on tear functions and ocular surface findings. Am J Ophthalmol 144(6):930–937. https://doi.org/10.1016/j.ajo.2007.07.037
Noori S, Sati A, Moulick PS, Kaushik J, Shankar S, Bose R (2020) Tear film abnormalities in pseudoexfoliation syndrome and normal healthy participants: a comparative analysis. Med J Armed Forces India 76(3):303–306. https://doi.org/10.1016/j.mjafi.2019.01.003
Kozobolis VP, Christodoulakis EV, Naoumidi II, Siganos CS, Detorakis ET, Pallikaris LG (2004) Study of conjunctival goblet cell morphology and tear film stability in pseudoexfoliation syndrome. Graefes Arch Clin Exp Ophthalmol 242(6):478–483. https://doi.org/10.1007/s00417-004-0865-3
Le Q, Cui X, Xiang J, Ge L, Gong L, Xu J (2014) Impact of conjunctivochalasis on visual quality of life: a community population survey. PLoS ONE 9(10):e110821. https://doi.org/10.1371/journal.pone.0110821
Mimura T, Yamagami S, Kamei Y, Goto M, Matsubara M (2013) Influence of axial length on conjunctivochalasis. Cornea 32(8):1126–1130. https://doi.org/10.1097/ICO.0b013e318292b7a2
Doganay S, Tasar A, Cankaya C, Firat PG, Yologlu S (2012) Evaluation of Pentacam-Scheimpflug imaging of anterior segment parameters in patients with pseudoexfoliation syndrome and pseudoexfoliative glaucoma. Clin Exp Optom 95(2):218–222. https://doi.org/10.1111/j.1444-0938.2011.00691.x
Inoue K, Okugawa K, Oshika T, Amano S (2003) Morphological study of corneal endothelium and corneal thickness in pseudoexfoliation syndrome. Jpn J Ophthalmol 47(3):235–239. https://doi.org/10.1016/s0021-5155(03)00022-4
Puska P, Vasara K, Harju M, Setälä K (2000) Corneal thickness and corneal endothelium in normotensive subjects with unilateral exfoliation syndrome. Graefes Arch Clin Exp Ophthalmol 238(8):659–663. https://doi.org/10.1007/s004170000159
Palko JR, Qi O, Sheybani A (2017) Corneal Alterations Associated with Pseudoexfoliation Syndrome and Glaucoma: A Literature Review. J Ophthalm Vis Res 12(3):312–324. https://doi.org/10.4103/jovr.jovr_28_17
Gumus K, Pflugfelder SC (2013) Increasing prevalence and severity of conjunctivochalasis with aging detected by anterior segment optical coherence tomography. Am J Ophthalmol 155(2):238-242.e2. https://doi.org/10.1016/j.ajo.2012.07.014
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Bediz Özen] and [Hakan Öztürk]. The first draft of the manuscript was written by [Bediz Özen] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Written informed consent was obtained from the parents.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was performed with the approval of Izmir Tepecik Training and Research Hospital's Medical Research Ethical Committee (approval number: 2020/10–10) and in-line with the ethical principles of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Özen, B., Öztürk, H. Does the conjunctivochalasis accompanied by pseudoexfoliation syndrome affect the ocular surface and anterior segment structures?. Int Ophthalmol 42, 3079–3087 (2022). https://doi.org/10.1007/s10792-022-02294-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02294-6