Abstract
Purpose
This retrospective study aimed to evaluate the prognostic factors associated with the success of fluid–gas exchange in patients who had undergone failed primary idiopathic macular hole (IMH) surgery.
Methods
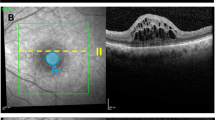
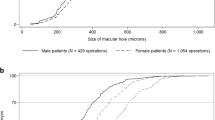
In total, 19 eyes of 19 patients with failed IMH surgery who then underwent fluid–gas exchange were included. Of those, 18 eyes had macular hole (MH) closure (successful, 15 eyes; unsuccessful, 3 eyes). Demographics, pre-operative characteristics, and pre-procedural characteristics were assessed. The patients were divided into successful (U or V-type closure) and unsuccessful groups (W-type or unclosed), following fluid–gas exchange. One eye was unclosed after fluid–gas exchange; therefore, this patient underwent additional vitrectomy for MH closure (unsuccessful).
Results
The outcomes of the fluid–gas exchange were categorized as unclosed or as U-type, V-type, or W-type closure. None of the patients experienced complications after the procedure. The successful group showed a significantly lower pre-operative and pre-procedural minimum diameter, base diameter, and macular hole volume, and higher pre-operative and pre-procedural macular hole index, hole form factor, and tractional hole index values. Moreover, a better visual prognosis was observed in the successful group.
Conclusion
These findings suggest that indices predicting favorable results of primary surgery for IMH are useful for predicting the success of fluid–gas exchange in patients with failed primary MH surgery.


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed in the present study are available from the corresponding author on reasonable request.
References
Kelly NE, Wendel RT (1991) Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol 109:654–659. https://doi.org/10.1001/archopht.1991.01080050068031
Smiddy WE, Feuer W, Cordahi G (2001) Internal limiting membrane peeling in macular hole surgery. Ophthalmology 108:1471–1476. https://doi.org/10.1016/s0161-6420(00)00645-x
Brooks HL Jr (2000) Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 107:1939–1948. https://doi.org/10.1016/s0161-6420(00)00331-6
Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW, Kampik A (2002) Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 86:390–393. https://doi.org/10.1136/bjo.86.4.390
Unsal E, Cubuk MO, Ciftci F (2019) Preoperative prognostic factors for macular hole surgery: which is better? Oman J Ophthalmol 12:20–24. https://doi.org/10.4103/ojo.OJO_247_2017
Imai M, Gotoh T, Iijima H (2005) Additional intravitreal gas injection in the early postoperative period for an unclosed macular hole treated with internal limiting membrane peeling. Retina 25:158–161. https://doi.org/10.1097/00006982-200502000-00007
Ohana E, Blumenkranz MS (1998) Treatment of reopened macular hole after vitrectomy by laser and outpatient fluid–gas exchange. Ophthalmology 105:1398–1403. https://doi.org/10.1016/S0161-6420(98)98019-8
Iwase T, Sugiyama K (2007) Additional gas injection after failed macular hole surgery with internal limiting membrane peeling. Clin Exp Ophthalmol 35:214–219. https://doi.org/10.1111/j.1442-9071.2007.01455.x
Jang JH, Kim YC, Kim KS (2009) The efficacy of fluid–gas exchange for the treatment of postvitrectomy retinal detachment. Korean J Ophthalmol 23:253–258. https://doi.org/10.3341/kjo.2009.23.4.253
Kusuhara S, Teraoka Escaño MF, Fujii S, Nakanishi Y, Tamura Y, Nagai A, Yamamoto H, Tsukahara Y, Negi A (2004) Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol 138:709–716. https://doi.org/10.1016/j.ajo.2004.04.063
Ruiz-Moreno JM, Staicu C, Piñero DP, Montero J, Lugo F, Amat P (2008) Optical coherence tomography predictive factors for macular hole surgery outcome. Br J Ophthalmol 92:640–644. https://doi.org/10.1136/bjo.2007.136176
Ozturk T, Karahan E, Er D, Kaya M, Kocak N, Kaynak S (2016) Effect of macular hole volume on postoperative central macular thickness. Arq Bras Oftalmol 79:137–142. https://doi.org/10.5935/0004-2749.20160043
Shpak AA, Shkvorchenko DO, Sharafetdinov IKh, Yukhanova OA (2016) Predicting anatomical results of surgical treatment of idiopathic macular hole. Int J Ophthalmol 9:253–257. https://doi.org/10.18240/ijo.2016.02.13
Wakely L, Rahman R, Stephenson J (2012) A comparison of several methods of macular hole measurement using optical coherence tomography, and their value in predicting anatomical and visual outcomes. Br J Ophthalmol 96:1003–1007. https://doi.org/10.1136/bjophthalmol-2011-301287
Dai YM, Shen J, Li JK, Jin XH, Li YM (2013) Optical coherence tomography predictive factors for idiopathic macular hole surgery outcome. Zhonghua Yan Ke Za Zhi 49:807–811
Zou JL, Zeng J (2019) The macular microstructure repair and predictive factors of surgical outcomes after vitrectomy for idiopathic macular hole. Int J Ophthalmol 12:852–857. https://doi.org/10.18240/ijo.2019.05.25
Nadal J, Delas B, Piñero A (2012) Vitrectomy without face-down posturing for idiopathic macular holes. Retina 32:918–921. https://doi.org/10.1097/IAE.0b013e318229b20e
Ye T, Yu JG, Liao L, Liu L, Xia T, Yang LL (2019) Macular hole surgery recovery with and without face-down posturing: a meta-analysis of randomized controlled trials. BMC Ophthalmol 19:265. https://doi.org/10.1186/s12886-019-1272-1
Rao X, Wang NK, Chen YP, Hwang YS, Chuang LH, Liu IC, Chen KJ, Wu WC, Lai CC (2013) Outcomes of outpatient fluid–gas exchange for open macular hole after vitrectomy. Am J Ophthalmol 156:326-333.e1. https://doi.org/10.1016/j.ajo.2013.03.031
Acknowledgements
This research was funded by the National Research Foundation of Korea grant [NRF-2019R1G1A1011559].
Funding
This research was funded by the National Research Foundation of Korea grant [NRF-2019R1G1A1011559]. The sponsors had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Conceptualization: YCK and YHL; Methodology: YCK and YHL; Formal Analysis: YCK; Investigation: SJL, JHJ, and YCK; Data Curation: SJL, JHJ, and YCK; Writing–Original Draft Preparation: YHL; Writing–Review & Editing: YCK and YHL; Supervision: YCK; Project Administration: YCK; Funding Acquisition: YCK.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Patient consent was waived because of the retrospective nature of the study.
Ethical approval
This retrospective study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Keimyung University Dongsan Hospital (IRB no. 2020-12-069, 22 December 2020).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, Y.H., Lee, S.J., Jang, J.H. et al. Prognostic factors in fluid–gas exchange after primary idiopathic macular hole surgery. Int Ophthalmol 42, 2811–2818 (2022). https://doi.org/10.1007/s10792-022-02271-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02271-z