Abstract
Purpose
To compare vascular microcirculation changes of the optic nerve head (ONH) and to evaluate the peripapillary retinal nerve fiber layer (RNFL) in the patients with unilateral pseudoexfoliation syndrome (PEXS), other eyes of these patients without PEXS and healthy control eyes using optical coherence tomography angiography (OCTA) and spectral domain optical coherence tomography (SD-OCT).
Methods
This cross-sectional study enrolled 29 pseudoexfoliative (PEX) and 29 fellow eyes of patients with unilateral PEXS, and 28 healthy eyes as controls. According to inclusion criteria the study group with asymmetric PEXS were normotensive and no glaucoma diagnosis. The vascularity of optic disc was evaluated with OCTA and peripapillary retinal nerve fiber layer with SD-OCT. ONH 4.5 × 4.5 mm OCTA gave us perfusion density (PD) and flow index (FI). Differences between the groups according to continuous variables were determined by independent samples t test. A p value less than 0.05 was considered as significant.
Results
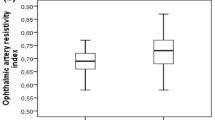
Twenty-nine patients with the mean age of 66.21 ± 7.55 (49–79) years was compared with 28 individuals in control group with mean age of 66.79 ± 4.43 (60–75) years. There was no difference regarding the age (p = 0.725). Female and male distribution in two groups were same (p = 0.219). Intraocular pressure (IOP) in PEXS group was measured as 16.17 ± 4.58 (10–21) mmHg, however IOP in the fellow eye was measured as 14.79 ± 3.35 (11–19) mmHg (p = 0.064) and control group was measured as 12.53 ± 1.66 (10–17) mmHg (p = 0.000). In the group with PEXS, the superior FI was found to be lower 0.39 ± 0.06 (0.26–0.45) (p = 0.008) than control group 0.42 ± 0.21 (0.36–0.45), and temporal FI in PEXS eyes was measured 0.42 ± 0.06 (0.32–0.52), which was significantly lower than control group (p = 0.022). Nasal FI was the parameter which was found significantly different from the PEXS free fellow eyes. The nasal FI value of eyes with PEX was 0.40 ± 0.05 (0.30–0.46), while the same value in PEX free fellow eyes was 0.42 ± 0.04 (0.33–0.47) (p = 0.029).
Conclusions
ONH evaluation with OCTA especially in the nasal segment is important for early diagnosis. OCTA can be a new method in follow-up and early diagnosis of patients with asymmetric PEXS to control ONH microcirculation and to evaluate early glaucomatose changes in both eyes.

Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are not publicly available due to the involvement of human participants, but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Ritch R, Schlotzer-Schrehardt U (2001) Exfoliation syndrome. Surv Ophthalmol 45(4):265–315. https://doi.org/10.1016/s0039-6257(00)00196-x
Schlotzer-Schrehardt U, Naumann GO (2006) Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol 141(5):921–937. https://doi.org/10.1016/j.ajo.2006.01.047
Hansen E, Sellevold OJ (1969) Pseudoexfoliation of the lens capsule. II. Development of the exfoliation syndrome. Acta Ophthalmol (Copenh) 47 (1):161–173. https://doi.org/10.1111/j.1755-3768.1969.tb05619.x
Henry JC, Krupin T, Schmitt M, Lauffer J, Miller E, Ewing MQ, Scheie HG (1987) Long-term follow-up of pseudoexfoliation and the development of elevated intraocular pressure. Ophthalmology 94(5):545–552. https://doi.org/10.1016/s0161-6420(87)33413-x
Klemetti A (1988) Intraocular pressure in exfoliation syndrome. Acta Ophthalmol Suppl 184:54–58. https://doi.org/10.1111/j.1755-3768.1988.tb02629.x
Plateroti P, Plateroti AM, Abdolrahimzadeh S, Scuderi G (2015) pseudoexfoliation syndrome and pseudoexfoliation glaucoma: a review of the literature with updates on surgical management. J Ophthalmol 2015:370371. https://doi.org/10.1155/2015/370371
Suwan Y, Geyman LS, Fard MA, Tantraworasin A, Chui TY, Rosen RB, Ritch R (2018) Peripapillary perfused capillary density in exfoliation syndrome and exfoliation glaucoma versus POAG and healthy controls: an OCTA study. Asia Pac J Ophthalmol (Phila) 7 (2):84–89. https://doi.org/10.22608/APO.2017318
Yasmeen N, Fatima N, Qamar Ul I (2016) Comparison of retinal nerve fiber layer thickness in patients having pseudo exfoliation syndrome with healthy adults. Pak J Med Sci 32 (6):1533–1536. https://doi.org/10.12669/pjms.326.11075
Puska PM (2002) Unilateral exfoliation syndrome: conversion to bilateral exfoliation and to glaucoma: a prospective 10-year follow-up study. J Glaucoma 11(6):517–524. https://doi.org/10.1097/00061198-200212000-00012
Yuksel N, Karabas VL, Arslan A, Demirci A, Caglar Y (2001) Ocular hemodynamics in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Ophthalmology 108(6):1043–1049. https://doi.org/10.1016/s0161-6420(01)00572-3
Rao HL, Pradhan ZS, Suh MH, Moghimi S, Mansouri K, Weinreb RN (2020) Optical coherence tomography angiography in glaucoma. J Glaucoma 29(4):312–321. https://doi.org/10.1097/IJG.0000000000001463
Werner AC, Shen LQ (2019) A review of OCT angiography in glaucoma. Semin Ophthalmol 34(4):279–286. https://doi.org/10.1080/08820538.2019.1620807
Kose HC, Tekeli O (2020) Optical coherence tomography angiography of the peripapillary region and macula in normal, primary open angle glaucoma, pseudoexfoliation glaucoma and ocular hypertension eyes. Int J Ophthalmol 13 (5):744–754. https://doi.org/10.18240/ijo.2020.05.08
Van Melkebeke L, Barbosa-Breda J, Huygens M, Stalmans I (2018) Optical coherence tomography angiography in glaucoma: a review. Ophthalmic Res 60(3):139–151. https://doi.org/10.1159/000488495
Chansangpetch S, Lin SC (2018) Optical coherence tomography angiography in glaucoma Care. Curr Eye Res 43(9):1067–1082. https://doi.org/10.1080/02713683.2018.1475013
Chen CL, Zhang A, Bojikian KD, Wen JC, Zhang Q, Xin C, Mudumbai RC, Johnstone MA, Chen PP, Wang RK (2016) Peripapillary retinal nerve fiber layer vascular microcirculation in glaucoma using optical coherence tomography-based microangiography. Invest Ophthalmol Vis Sci 57 (9):OCT475–485. https://doi.org/10.1167/iovs.15-18909
Robbins CB, Grewal DS, Thompson AC, Soundararajan S, Yoon SP, Polascik BW, Scott BL, Fekrat S (2021) Identifying peripapillary radial capillary plexus alterations in Parkinson’s disease using optical coherence tomography angiography. Ophthalmol Retina. https://doi.org/10.1016/j.oret.2021.03.006
CIRRUS HD-OCT . User manual—Models 500, 5000. Carl Zeiss Meditec, Inc.; (2017).
Lee JC, Grisafe DJ, Burkemper B, Chang BR, Zhou X, Chu Z, Fard A, Durbin M, Wong BJ, Song BJ, Xu BY, Wang R, Richter GM (2020) Intrasession repeatability and intersession reproducibility of peripapillary OCTA vessel parameters in non-glaucomatous and glaucomatous eyes. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-317181
Garcia-Medina JJ, Rubio-Velazquez E, Lopez-Bernal MD, Parraga-Munoz D, Perez-Martinez A, Pinazo-Duran MD, Del-Rio-Vellosillo M (2020) Optical coherence tomography angiography of macula and optic nerve in autism spectrum disorder: a pilot study. J Clin Med 9 (10). https://doi.org/10.3390/jcm9103123
Richter GM, Chang R, Situ B, Chu Z, Burkemper B, Reznik A, Bedrood S, Kashani AH, Varma R, Wang RK (2018) Diagnostic performance of macular versus peripapillary vessel parameters by optical coherence tomography angiography for glaucoma. Transl Vis Sci Technol 7(6):21. https://doi.org/10.1167/tvst.7.6.21
Quigley HA (2019) 21st century glaucoma care. Eye (Lond) 33(2):254–260. https://doi.org/10.1038/s41433-018-0227-8
Kivela T, Hietanen J, Uusitalo M (1997) Autopsy analysis of clinically unilateral exfoliation syndrome. Invest Ophthalmol Vis Sci 38(10):2008–2015
Schweitzer C (2018) Pseudoexfoliation syndrome and pseudoexfoliation glaucoma. J Fr Ophtalmol 41(1):78–90. https://doi.org/10.1016/j.jfo.2017.09.003
Wang W, He M, Zhou M, Zhang X (2014) Ocular pseudoexfoliation syndrome and vascular disease: a systematic review and meta-analysis. PLoS ONE 9(3):e92767. https://doi.org/10.1371/journal.pone.0092767
Jia Y, Wei E, Wang X, Zhang X, Morrison JC, Parikh M, Lombardi LH, Gattey DM, Armour RL, Edmunds B, Kraus MF, Fujimoto JG, Huang D (2014) Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology 121(7):1322–1332. https://doi.org/10.1016/j.ophtha.2014.01.021
Kim JA, Kim TW, Lee EJ, Girard MJA, Mari JM (2018) Microvascular changes in peripapillary and optic nerve head tissues after trabeculectomy in primary open-angle glaucoma. Invest Ophthalmol Vis Sci 59(11):4614–4621. https://doi.org/10.1167/iovs.18-25038
Ocakoglu O, Koyluoglu N, Kayiran A, Tamcelik N, Ozkan S (2004) Microvascular blood flow of the optic nerve head and peripapillary retina in unilateral exfoliation syndrome. Acta Ophthalmol Scand 82(1):49–53. https://doi.org/10.1046/j.1600-0420.2003.00196.x
Goker YS, Kiziltoprak H (2020) Quantitative analysis of radial peripapillary capillary plexuses in patients with clinically unilateral pseudoexfoliation syndrome. Graefes Arch Clin Exp Ophthalmol 258(6):1217–1225. https://doi.org/10.1007/s00417-020-04643-6
Cinar E, Yuce B, Aslan F (2019) Retinal and choroidal vascular changes in eyes with pseudoexfoliation syndrome: a comparative study using optical coherence tomography angiography. Balkan Med J 37(1):9–14. https://doi.org/10.4274/balkanmedj.galenos.2019.2019.5.5
Subasi S, Yuksel N, Basaran E, Pirhan D (2021) Comparison of vessel density in macular and peripapillary regions between primary open-angle glaucoma and pseudoexfoliation glaucoma using OCTA. Int Ophthalmol 41(1):173–184. https://doi.org/10.1007/s10792-020-01564-5
Simsek M, Kocer AM, Cevik S, Sen E, Elgin U (2020) Evaluation of the optic nerve head vessel density in the patients with asymmetric pseudoexfoliative glaucoma: an OCT angiography study. Graefes Arch Clin Exp Ophthalmol 258(7):1493–1501. https://doi.org/10.1007/s00417-020-04668-x
Safizadeh M, Shaabani A, Kamalipour A, Fard MA, Yeh K, Yaseri M, Hamzeh N, Khatibi N, Rao HL, Weinreb R, Moghimi S (2020) Optic nerve head vessel density in different stages of pseudoexfoliation disease. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-317605
Funding
None relevant to this study. No financial support was received for this submission.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by OD, SLS, CŞ, SK, SK, ABC. The first draft of the manuscript was written by Ozlem Dikmetas and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Hacettepe University School of Medicine Institutional Review Board (GO 20/564) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human or animal participants
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was conducted in the Department of Ophthalmology, Hacettepe University School of Medicine.
Rights and permissions
About this article
Cite this article
Dikmetas, O., Sadigh, S.L., Şekerler, C. et al. Optic nerve head microvascular characteristics in patients with unilateral pseudoexfoliation syndrome: an optical coherence tomography angiography study. Int Ophthalmol 42, 2397–2405 (2022). https://doi.org/10.1007/s10792-022-02239-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02239-z