Abstract
Purpose
To study the correlation between retinoblastoma (RB) associated with orbital pseudocellulitis and high-risk histopathology features.
Methods
Retrospective study of 32 patients who underwent primary enucleation for RB presenting with orbital pseudocellulitis.
Results
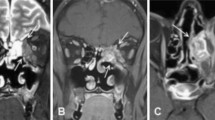
All RB patients presented with orbital pseudocellulitis. The mean age at presentation of RB was 30 months (median, 24 months; range, 3–70 months). There were 14 (44%) males and 18 (56%) females. All patients were referred with a diagnosis of RB with orbital pseudocellulitis. Tumor was bilateral in 12 (38%) patients but orbital pseudocellulitis was unilateral in all cases. The pseudocellulitis features included proptosis (n = 9; 28%), eyelid edema (n = 22; 69%), conjunctival congestion (n = 23; 72%), and conjunctival chemosis (n = 15; 47%). Based on clinical features and orbital imaging, all patients were diagnosed to have group E intraocular RB. All patients received intravenous steroids prior to enucleation. On histopathology, tumor necrosis was present in all cases with a mean % necrosis of 60% (median, 60%; range, 10% to 90%). Most tumors (72%) were poorly differentiated. High-risk histopathology features were noted in 23 (72%) cases and adjuvant chemotherapy was advised for all these patients. The most common high-risk histopathology features included post-laminar optic nerve infiltration (34%) and scleral infiltration (22%). Over a mean follow-up period of 34 months (median, 9 months; range, < 1–188 months), there was no event of metastasis or death in any patient.
Conclusion
RB presenting with orbital pseudocellulitis is associated with high incidence of high-risk histopathology features.

Similar content being viewed by others
Data availability and material
Data are available with the authors.
References
Abramson DH, Frank CM, Susman M, Whalen MP, Dunkel IJ, Boyd NW 3rd (1998) Presenting signs of retinoblastoma. J Pediatr 132(3 Pt 1):505–508
Agarwal M, Biswas J, Shanmugam MP (2004) Retinoblastoma presenting as orbital cellulitis: report of four cases with a review of the literature. Orbit 23(2):93–98
Al Rashaed S, Elkhamary SM, Al Sheikh O, Al Mesfer S, Al-Dhibi H, Al MA (2020) Adult presentation of retinoblastoma in Saudi patient. Saudi J Ophthalmol 34(2):136–138
Balasubramanya R, Pushker N, Bajaj MS, Ghose S, Kashyap S, Rani A (2004) Atypical presentations of retinoblastoma. J Pediatr Ophthalmol Strabismus 41(1):18–24
Ben Meir A, Bardenstein D, Peiffer R (1995) Retinoblastoma presenting with orbital cellulitis: a mechanical hypothesis. Invest Ophthalmol Vis Sci 36:492
Chong EM, Coffee RE, Chintagumpala M, Hurwitz RL, Hurwitz MY, Chévez-Barrios P (2006) Extensively necrotic retinoblastoma is associated with high-risk prognostic factors. Arch Pathol Lab Med 130(11):1669–1672
Foster BS, Mukai S (1996) Intraocular retinoblastoma presenting as ocular and orbital inflammation. Int Ophthalmol Clin 36(1):153–160
Kaliki S (2018) How to do an enucleation for retinoblastoma. Community Eye Health 31(101):20–22
Kaliki S, Gupta S, Ramappa G, Mohamed A, Mishra DK (2020) High-risk retinoblastoma based on age at primary enucleation: a study of 616 eyes. Eye (Lond) 34(8):1441–1448
Kaliki S, Patel A, Iram S, Palkonda VAR (2017) Clinical presentation and outcomes of stage III or stage IV retinoblastoma in 80 Asian Indian patients. J Pediatr Ophthalmol Strabismus 54(3):177–184
Kaliki S, Patel A, Iram S, Ramappa G, Mohamed A, Palkonda VAR (2019) Retinoblastoma in India: clinical presentation and outcome in 1,457 patients (2,074 Eyes). Retina 39(2):379–391
Kaliki S, Shields CL, Eagle RC Jr, Iram S, Shields JA (2018) High-risk intraocular retinoblastoma: comparison between Asian Indians and Americans from two major referral centers. Retina 38(10):2023–2029
Martino F, Gelmi MC, Galluzzi P, De Francesco S, Miracco C, Hadjistilianou D (2020) Orbital pseudocellulitis: a retinoblastoma-associated masquerade syndrome. Ocul Oncol Pathol 6(6):430–437
Mullaney PB, Karcioglu ZA, Huaman AM, Al-Mesfer S (1998) Retinoblastoma associated orbital cellulitis. Br J Ophthalmol 82(5):517–521
Nadol JB Jr (1977) Pseudocellulitis of the orbit. Ann Otol Rhinol Laryngol 86(1 Pt 1):86–88
Nalcı H, Gündüz K, Erden E (2018) Necrotic intraocular retinoblastoma associated with orbital cellulitis. Surv Ophthalmol 63(1):114–118
Read RW, Zamir E, Rao NA (2002) Neoplastic masquerade syndromes. Surv Ophthalmol 47(2):81–124
Sachdeva R, Schoenfield L, Marcotty A, Singh AD (2011) Retinoblastoma with autoinfarction presenting as orbital cellulitis. J AAPOS 15(3):302–304
Shields JA, Shields CL, Suvarnamani C, Schroeder RP, DePotter P (1991) Retinoblastoma manifesting as orbital cellulitis. Am J Ophthalmol 112(4):442–449
Walinjkar J, Krishnakumar S, Gopal L, Ramesh A, Khetan V (2013) Retinoblastoma presenting with orbital cellulitis. J AAPOS 17(3):282–286
Funding
This work is supported by Hyderabad Eye Research Foundation, Hyderabad, India and The Operation Eyesight Universal Institute for Eye Cancer, Hyderabad, India.
Author information
Authors and Affiliations
Contributions
SK was responsible for the concept and formulation of the work, data analysis, and manuscript preparation. VSV and AM were responsible for data collection and reviewing the manuscript. SJ and DKM were responsible for histopathological correlation and reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest exist for any author.
Consent for publication
Consent for publication was obtained from the patients.
Consent to participate
Consent to participate was obtained from the patients.
Ethical approval
This study has been approved by the Institute Ethics Committee.
Human and animal rights
This work involved demographic and clinical information of human participants. Research involved demographic and clinical information of human participants. All procedures performed were in accordance with the ethical standards of the institutional ethical standards of the institutional ethics committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent has been obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Précis Of the 32 patients who underwent primary enucleation for retinoblastoma presenting as orbital pseudocellulitis, tumor necrosis was noted in all cases (median, 70%; range, 10–90%) and high risk histopathology features in 23 (72%) cases.
Rights and permissions
About this article
Cite this article
Kaliki, S., Jakati, S., Vempuluru, V.S. et al. Retinoblastoma associated with orbital pseudocellulitis and high-risk retinoblastoma: a study of 32 eyes. Int Ophthalmol 42, 19–26 (2022). https://doi.org/10.1007/s10792-021-01993-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01993-w