Abstract
Purpose
To report the outcomes of secondary Descemet Membrane Endothelial Keratoplasty (DMEK) performed for failed primary DMEK.
Methods
The medical records of all patients undergoing secondary DMEK due to failure of primary DMEK were reviewed. Reasons for failure were sought and best-corrected visual acuity (BCVA), endothelial cell density (ECD) and complications of secondary DMEK were evaluated.
Results
A total of 10 cases undergoing secondary DMEK following failed primary DMEK were identified. Presumed reasons for failure included donor ECD ≤ 2300 cells/mm2 (n = 4), difficulty during graft preparation (n = 2), graft detachment (n = 2), acute angle closure due to retroiridal air dislocation (n = 1), inverse graft positioning (n = 1) and phacoemulsification (n = 1). Eyes with low visual potential were not excluded from the study group. We should note that one patient (case no7) had both low ECD and graft detachment as reasons for failure and as a result he is counted twice.
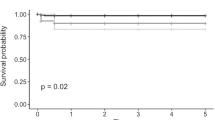
Median BCVA (decimal fraction) increased from 0.1 (range, 0.01; 0.3) to 0.5 (0.05; 1.0) at one month and remained stable thereafter. A BCVA of 0.5 or higher was achieved in 7 cases at the final follow-up. Mean ECD fell from 2628 ± 284 cells/mm2 to 1391 ± 252cells/mm2 at 6 months (47% reduction) and 959 ± 225cells/mm2 at 24 months (64% reduction) (P ≤ 0.028). Complications included the incomplete removal of the primary graft and mild iris bleeding, decompensation of a preexisting primary open-angle glaucoma and retroiridal air dislocation.
Conclusions
Apart from low donor ECD, surgical challenges, i.e., difficulty with graft preparation, inverse graft positioning, and retroiridal air dislocation, were main reasons for failure of primary DMEK. Secondary DMEK showed a good safety profile and reasonable visual outcomes.

Similar content being viewed by others
Data availability
All data and materials of our research are available for evaluation.
Abbreviations
- DMEK:
-
Descemet membrane endothelial keratoplasty
- BCVA:
-
Best-corrected visual acuity
- CF:
-
Counting fingers
- DSAEK:
-
Descemet stripping endothelial keratoplasty
- ECD:
-
Endothelial cell density
- CCT:
-
Central corneal thickness
- ECL:
-
Endothelial cell loss
References
Lovaglio B, Trindade C, Coutinho G (2019) Descemetmembrane endothelial keratoplasty (DMEK): an update on safety, efficacy and patientselection. ClinOphthalmol 13:1549–1557. https://doi.org/10.2147/OPTH.S178473
Anshu A, Price MO, Price FW Jr (2012) Risk of corneal transplant rejection significantly reduced with Descemet’s membrane endothelial keratoplasty. Ophthalmology 119(3):536–540. https://doi.org/10.1016/j.ophtha.2011.09.019
Deng SX, Lee WB, Hammersmith KM et al (2018) Descemet membrane endothelial keratoplasty: safety and outcomes: a report by the american academy of ophthalmology. Ophthalmology 125(2):295–310. https://doi.org/10.1016/j.ophtha.2017.08.
Dirisamer M, Ham L, Dapena I et al (2011) Efficacy of descemet membrane endothelial keratoplasty: clinical outcome of 200 consecutive cases after a learning curve of 25 cases. Arch Ophthalmol 129:1435–1443
Guerra FP, Anshu A, Price MO et al (2011) Descemet’s membrane endothelial keratoplasty: prospective study of 1-year visual outcomes, graft survival, and endothelial cell loss. Ophthalmology 118:2368–2373
Peraza-Nieves J, Baydoun L, DapenaI I et al (2017) Two-year clinical outcome of 500 consecutive cases undergoing descemet membrane endothelial keratoplasty. Cornea 36(6):655–660.
Price D, Kelley M, Price F Jr et al (2018) Five-year graft survival ofdescemet membrane endothelial keratoplasty (ek) versus descemet stripping ek and theeffectofdonor sex matching. Ophthalmology 125(10):1508–1514. https://doi.org/10.1016/j.ophtha.2018.03.050
Baydoun L, van Dijk K, Dapena I et al (2015) Repeat descemet membrane endothelial keratoplasty after complicated primary descemet membrane endothelial keratoplasty. Ophthalmology 122(1):8–16. https://doi.org/10.1016/j.ophtha.2014.07.024
Yoeruek E, Bartz-Schmidt KU (2013) Secondary Descemet membrane endothelial keratoplasty after failed primary Descemet membrane endothelial keratoplasty: clinical results. Cornea 32(11):1414–1417. https://doi.org/10.1097/ICO.0b013e31828321c1
Price MO, Feng MT, McKee Y et al (2015) Repeat descemet membrane endothelial keratoplasty: secondary grafts with early intervention are comparable with fellow-eye primary grafts. Ophthalmology 122(8):1639–1644. https://doi.org/10.1016/j.ophtha.2015.04.037
Dirisamer M, van Dijk K, Dapena I et al (2012) Prevention and management of graft detachment in descemet membrane endothelial keratoplasty. Arch Ophthalmol. 130(3):280–291. https://doi.org/10.1001/archophthalmol.2011.343
Dapena I, Moutsouris K, Droutsas K et al (2011) Standardized “no-touch” technique for Descemet membrane endothelial keratoplasty. Arch Ophthalmol 129(1):88–94. https://doi.org/10.1001/archophthalmol.2010.334
Lie J, Birbal R, Ham L et al (2008) Donor tissue preparation for Descemet membrane endothelial keratoplasty. Cataract Refract Surg 34(9):1578–83. https://doi.org/10.1016/j.jcrs.2008.05.036
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
KD designed and conducted the study. All authors analyzed the results and prepared the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Droutsas, K., Alexopoulos, P., Giachos, I. et al. Secondary DMEK following failed primary DMEK. Int Ophthalmol 41, 3287–3293 (2021). https://doi.org/10.1007/s10792-021-01890-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01890-2