Abstract
Purpose
To investigate the changes and evaluate the diagnosis value of circumpapillary vessel density (VD) in cases of acute primary angle closure (APAC).
Design
Case–control study.
Methods
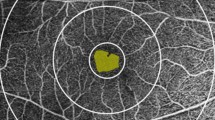
APAC patients with a history of unilateral acute attack were enrolled. The eyes with acute episode constituted the case group while the contralateral eyes without attack consisted of the control group. Ophthalmic examinations including slit-lamp examination, best-corrected visual acuity, intraocular pressure and visual field were carried out. Retinal nerve fiber layer (RNFL), macular ganglion cell complex (GCC) were measured by spectral-domain optical coherence tomography, while VD was assessed by optical coherence tomography angiography.
Results
The whole en face image vessel density (wiVD), circumpapillary vessel density (cpVD) and inside disk VD for both all vessels and capillary were all significantly lower in the APAC eyes compared to the fellow eyes (P < 0.01 for all). In APAC eyes, the wiVD, inside disk VD and cpVD both for all vessels and capillary were all positively correlated with RNFL and GCC thicknesses but negatively correlated with the mean deviation (MD), pattern standard deviation (PSD) and the duration of acute attack (all P < 0.01). From the ROC curve, the cpVDcap, wiVDcap, cpVDall and wiVDall all showed comparable diagnostic ability with RNFL, GCC and MD to differentiate eyes with APAC from the fellow eyes (all P > 0.05). The inside disk VDcap and VDall demonstrated significant lower diagnostic ability than the cpVDcap, wiVDcap, cpVDall and wiVDall (all P < 0.001).
Conclusions
In APAC eyes, circumpapillary VD decreased significantly compared with the fellow unaffected eyes. They were significantly correlated with thicknesses of RNFL and GCC, and visual field MD and PSD in the APAC eyes. The patients with longer duration of acute attack were more likely to have lower cpVD. For APAC, the diagnostic ability of wiVD and cpVD was similar with RNFL, GCC and MD and was higher than inside disk VD.

Similar content being viewed by others
Data availability
The data used to support the findings of this study are included within the article.
References
Sun X, Dai Y, Chen Y et al (2017) Primary angle closure glaucoma: what we know and what we don’t know. Prog Retin Eye Res 57:26–45
Fu L, Fung FK, Lo AC et al (2018) Transcorneal electrical stimulation inhibits retinal microglial activation and enhances retinal ganglion cell survival after acute ocular hypertensive injury. Transl Vis Sci Technol 7:7
Yang H, Reynaud J, Lockwood H et al (2017) The connective tissue phenotype of glaucomatous cupping in the monkey eye - clinical and research implications. Prog Retin Eye Res 59:1–52
Yanagi M, Kawasaki R, Wang JJ, Wong TY, Crowston J, Kiuchi Y (2011) Vascular risk factors in glaucoma: a review. Clin Exp Ophthalmol 39:252–258
Yarmohammadi A, Zangwill LM, Diniz-Filho A et al (2017) Peripapillary and macular vessel density in patients with glaucoma and single-hemifield visual field defect. Ophthalmology 124:709–719
Jia Y, Tan O, Tokayer J et al (2012) Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express 20:4710–4725
Bojikian KD, Chen PP, Wen JC (2019) Optical coherence tomography angiography in glaucoma. Curr Opin Ophthalmol 30:110–116
Liu L, Jia Y, Takusagawa HL et al (2015) Optical coherence tomography angiography of the peripapillary retina in glaucoma. JAMA Ophthalmol 133:1045–1052
Hou H, Moghimi S, Zangwill LM et al (2019) Macula vessel density and thickness in early primary open-angle glaucoma. Am J Ophthalmol 199:120–132
Moghimi S, SafiZadeh M, Xu BY et al (2020) Vessel density and retinal nerve fibre layer thickness following acute primary angle closure. Br J Ophthalmol 104:1103–1108
Zhang S, Wu C, Liu L et al (2017) Optical coherence tomography angiography of the peripapillary retina in primary angle-closure glaucoma. Am J Ophthalmol 182:194–200
Moghimi S, SafiZadeh M, Fard MA et al (2019) Changes in optic nerve head vessel density after acute primary angle closure episode. Invest Ophthalmol Vis Sci 60:552–558
Wang X, Jiang C, Kong X, Yu X, Sun X, Oho AUID (2017) Peripapillary retinal vessel density in eyes with acute primary angle closure: an optical coherence tomography angiography study. Graefes Arch Clin Exp Ophthalmol 255:1013–1018
Zhu X, Zeng W, Wu S et al (2019) Measurement of retinal changes in primary acute angle closure glaucoma under different durations of symptoms. J Ophthalmol 2019:5409837
Takusagawa HL, Liu L, Ma KN et al (2017) Projection-resolved optical coherence tomography angiography of macular retinal circulation in glaucoma. Ophthalmology 124:1589–1599
Bekkers A, Borren N, Ederveen V et al (2020) Microvascular damage assessed by optical coherence tomography angiography for glaucoma diagnosis: a systematic review of the most discriminative regions. Acta Ophthalmol 98:537–558
Rao HL, Pradhan ZS, Weinreb RN et al (2017) Vessel density and structural measurements of optical coherence tomography in primary angle closure and primary angle closure glaucoma. Am J Ophthalmol 177:106–115
Feke GT, Bex PJ, Taylor CP et al (2014) Effect of brimonidine on retinal vascular autoregulation and short-term visual function in normal tension glaucoma. Am J Ophthalmol 158:105-112.e1
Funding
This study was supported by the Wenzhou Municipal Science and Technology Bureau of China (Grant No. Y20190170) and Research Initiation Project of the Affiliated Eye Hospital of Wenzhou Medical University (KYQD202001).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [LN and PL], [YY, WP] and [JX, YKC, TL]. The first draft of the manuscript was written by [LN and LF] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the Clinical Research Ethics Committee of the Affiliated Eye Hospital of Wenzhou Medical University, and followed the tenets of the Declaration of Helsinki in 1964.
Informed consent
Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nie, L., Xu, J., Fu, L. et al. Changes in circumpapillary retinal vessel density after acute primary angle closure episode via OCT angiography. Int Ophthalmol 41, 2389–2397 (2021). https://doi.org/10.1007/s10792-021-01793-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01793-2