Abstract
Purpose
Retinal detachment (RD) is a vision-threatening complication of open globe injuries (OGI). This study sought to assess clinical, radiographic, and intraoperative risk factors for RD after OGI. A secondary goal was to test the retinal detachment after open globe injury (RD-OGI) score.
Methods
Records of patients undergoing OGI repair at a single trauma center over 3 years were reviewed using a retrospective case series design. Eyes that were enucleated or lost to follow up within 30 days of OGI without evidence of RD were excluded. Potential risk factors for RD development were assessed by logistic regression or chi-square tests were appropriate and were entered into a multivariate logistic regression if significant on univariate analysis. Risk of RD for each eye was categorized by its RD-OGI score.
Results
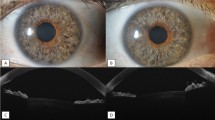
Seventy-three eyes (72 patients) were included. In univariate analysis, afferent pupillary defect, worse visual acuity, posterior injury, vitreous hemorrhage, and posterior segment volume loss (PSVL) on CT were strong predictors of RD. In multivariate analysis, only PSVL on CT (adjusted OR 10.8, P = 0.025) maintained a statistically significant association with RD risk. At 1 year, 5% of low-risk eyes, 20% of moderate-risk eyes, and 67% of high-risk eyes developed RD. These rates were not significantly different from the RD-OGI derivation or validation cohorts (P = 0.90 and P = 0.67, respectively).
Conclusion
PSVL on CT increases the risk of RD after OGI. The RD-OGI Score was a good prognostic tool for assessing RD risk after OGI in this population.



Similar content being viewed by others
Data availability
De-identified patient data were contained in a single spreadsheet, which is available from any author upon reasonable request.
References
Négrel A, Thylefors B (1998) The global impact of eye injuries. Ophthalmic Epidemiol 5:143–169
Pieramici DJ, Sternberg P Jr et al (1997) A system for classifying mechanical injuries of the eye (globe). Am J Ophthalmol 123(6):820–831
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD (2002) The Ocular Trauma Score (OTS). Ophthalmol Clin North Am 15(2):163–vi. https://doi.org/10.1016/s0896-1549(02)00007-x
Kono Kono JO, Maier M, Schmidt T (2001) Clinical predictors of retinal detachment after open globe injury. Klin Monbl Augenheilkd 218:553–556. https://doi.org/10.1055/s-2001-17137
Lin H, Lema GM, Yoganathan P (2016) Prognostic indicators of visual acuity after open globe injury and retinal detachment repair. Retina 36(4):750–757. https://doi.org/10.1097/IAE.0000000000000798
Stryjewski TP, Andreoli CM, Eliott D (2014) Retinal detachment after open globe injury. Ophthalmol 121(1):327–333. https://doi.org/10.1016/j.ophtha.2013.06.045
Brodowska K, Stryjewski TP, Papavasileiou E et al (2017) Validation of the retinal detachment after open globe injury (RD-OGI) score as an effective tool for predicting retinal detachment. Ophthalmol 124(5):674–678. https://doi.org/10.1016/j.ophtha.2004.05.010
Schulze-Bonsel K, Feltgen N, Burau H et al (2006) Visual acuities “hand motion” and “count fingers” can be quantified with the Freiburg visual acuity test. Invest Vis Sci Ophthalmol 47:1236–1240. https://doi.org/10.1167/iovs.05-0981
Cardillo JA, Stout JT, LaBree L et al (1997) Post-traumatic proliferative vitreoretinopathy: the epidemiologic profile, onset, risk factors, and visual outcome. Ophthalmol 104:1166–1173. https://doi.org/10.1016/S0161-6420(97)30167-5
Feng K, Hu Y, Wang C et al (2013) Risk factors, anatomical, and visual outcomes of injured eyes with proliferative vitreoretinopathy: eye injury vitrectomy study. Retina 33(8):1512–1518. https://doi.org/10.1097/IAE.0b013e3182852469
Cleary PE, McInckler DS, Ryan SJ (1980) Ultrastructure of traction retinal detachment in rhesus monkey eyes after a posterior penetrating injury. Am J Ophthalmol 90(6):829–845. https://doi.org/10.1016/S0002-9394(14)75198-0
Cleary PE, Ryan SJ (1979) Histology of wound, vitreous, and retina in experimental posterior penetrating eye injury in the rhesus monkey. Am J Ophthalmol 88(2):221–231. https://doi.org/10.1016/0002-9394(79)90469-0
Hui YN, Goodnight R, Sorgente N et al (1989) Fibrovascular proliferation and retinal detachment after intravitreal injection of activated macrophages in the rabbit eye. Am J Ophthalmol 108(2):176–184. https://doi.org/10.1016/0002-9394(89)90014-7
Entezari M, Rabei HM, Badalabadi MM et al (2006) Visual outcome and ocular survival in open-globe injuries. Injury 37:633–637. https://doi.org/10.1016/j.injury.2006.02.043
Lesniak SP, Bauza A, Son JH et al (2011) Twelve-year review of pediatric traumatic open globe injuries in an urban U.S. population. J Pediatr Ophthalmol Strabismus 49:73–79. https://doi.org/10.3928/01913913-20110712-02
Dunkin JM, Crum AV, Swanger RS, Bokhari SA (2011) Globe trauma. Semin Ultrasound CT MR 32:51–56. https://doi.org/10.1053/j.sult.2010.09.003
Arey ML, Mootha VV, Whittemore AR et al (2007) Computed tomography in the diagnosis of occult open-globe injuries. Ophthalmol 114(8):1448–1452. https://doi.org/10.1016/j.ophtha.2006.10.051
Yuan WH, Hsu HC, Cheng HC et al (2014) CT of globe rupture: analysis and frequency of findings. AJR Am J Roentgenol 202(5):1100–1107. https://doi.org/10.2214/AJR.13.11010
Joseph DP, Pieramici DJ, Beauchamp NJ (2000) Computed tomography in the diagnosis and prognosis of open-globe injuries. Ophthalmol 107(10):1899–1906. https://doi.org/10.1016/S0161-6420(00)00335-3
Bodanapally UK, Addis H, Dreizin D et al (2017) Prognostic predictors of visual outcome in open globe injury: Emphasis on facial CT findings. AJNR Am J Neuroradiol 38(5):1013–1018. https://doi.org/10.3174/ajnr.A5107
Funding
The authors declare no outside sources of funding for this research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and initial data collection were performed by Travis Bales. Analysis was performed by Harpal S. Sandhu, MD. The first draft of the manuscript was written by Travis Bales with substantial contribution and revision by Harpal S. Sandhu, MD. Additional data collection and subsequent manuscript revision was performed by Tyler Ogden. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Research ethics and patient consent
In this retrospective study, care was taken to protect the identities of human subjects. Patient names were substituted with a numerical code. De-identified patient data were contained in a single spreadsheet. The study was approved by the University of Louisville Institutional Review Board (Study ID# 19.0068) and conducted in accordance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act (HIPAA). An informed consent waiver was approved by the IRB in accordance with United States Code of Federal Regulations [45 CFR 46.116 (d)].
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bales, T., Ogden, T. & Sandhu, H.S. Clinical, radiographic, and intraoperative risk factors for retinal detachment after open globe injury. Int Ophthalmol 41, 815–823 (2021). https://doi.org/10.1007/s10792-020-01635-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01635-7