Abstract
Purpose
To evaluate the cellular and molecular retinal injuries induced by various intraocular pressure (IOP) settings in a mouse model of acute ocular hypertension (AOH), and to advise using a more moderate target IOP during phacoemulsification (phaco) surgery.
Methods
A mouse model of AOH that mimics a transient IOP elevation during phacoemulsification cataract surgery was established. Six groups with various settings of target IOP were included. Retinal tissues were assessed with terminal deoxynucleotidyl transferase-mediated 2′-deoxyuridine 5′-triphosphate nick end-labeling (TUNEL) staining for neuron loss, immunofluorescence with Iba1 for microglia activation, and quantitative real-time polymerase chain reaction analysis with tight junction proteins (claudin-3 and claudin-5) or classic inflammation markers (IL-1β and eNOS) for impairment of the blood–retinal barrier (BRB) and inflammatory injury.
Results
Compared with those in the 45-mmHg IOP group, significantly increased number of neurons loss and increased microglia activation were observed in 90-mmHg IOP group. In addition, the expression of claudin-3 and claudin-5 was significantly decreased, while the expression of IL1-β and eNOS was up-regulated, indicating impairment of the BRB and inflammatory injury in the retina. Furthermore, these findings of neuron loss, microglia activation, and inflammation in the 90-mmHg groups were exacerbated when an IOP-induced retinal injury was established 5 days earlier, while those in the 45-mmHg groups remained almost unchanged.
Conclusions
In conclusion, these results showed that a relatively commonly used high IOP setting (90 mmHg) could induce significantly more serious retinal injury. An IOP setting around 45 mmHg is relatively safe and might be recommended in phaco surgery, especially in patients with advanced glaucoma, previous acute angle closure crisis, or other diseases with fragile retina and optic nerve.





Similar content being viewed by others
Availability of data, material, and code
All of the data, material, and code in this article are available.
References
Kelman CD (1967) Phaco-emulsification and aspiration. A new technique of cataract removal. A preliminary report. Am J Ophthalmol 64(1):23–35
Khokhar S, Aron N, Sen S, Pillay G, Agarwal E (2017) Effect of balanced phacoemulsification tip on the outcomes of torsional phacoemulsification using an active-fluidics system. J Cataract Refract Surg 43(1):22–28. https://doi.org/10.1016/j.jcrs.2016.11.034
Schriefl SM, Stifter E, Menapace R (2014) Impact of low versus high fluidic settings on the efficacy and safety of phacoemulsification. Acta Ophthalmol 92(6):e454–e457. https://doi.org/10.1111/aos.12200
Ting DSJ, Rees J, Ng JY, Allen D, Steel DHW (2017) Effect of high-vacuum setting on phacoemulsification efficiency. J Cataract Refract Surg 43(9):1135–1139. https://doi.org/10.1016/j.jcrs.2017.09.001
Quigley HA, McKinnon SJ, Zack DJ, Pease ME, Kerrigan-Baumrind LA, Kerrigan DF, Mitchell RS (2000) Retrograde axonal transport of BDNF in retinal ganglion cells is blocked by acute IOP elevation in rats. Invest Ophthalmol Vis Sci 41(11):3460–3466
Findl O, Strenn K, Wolzt M, Menapace R, Vass C, Eichler HG, Schmetterer L (1997) Effects of changes in intraocular pressure on human ocular haemodynamics. Curr Eye Res 16(10):1024–1029. https://doi.org/10.1076/ceyr.16.10.1024.9024
Khng C, Packer M, Fine IH, Hoffman RS, Moreira FB (2006) Intraocular pressure during phacoemulsification. J Cataract Refract Surg 32(2):301–308. https://doi.org/10.1016/j.jcrs.2005.08.062
Zhao Y, Li X, Tao A, Wang J, Lu F (2009) Intraocular pressure and calculated diastolic ocular perfusion pressure during three simulated steps of phacoemulsification in vivo. Invest Ophthalmol Vis Sci 50(6):2927–2931. https://doi.org/10.1167/iovs.08-2996
Zhao D, He Z, Vingrys AJ, Bui BV, Nguyen CT (2015) The effect of intraocular and intracranial pressure on retinal structure and function in rats. Physiol Rep 3(8):e12507. https://doi.org/10.14814/phy2.12507
Tranos P, Bhar G, Little B (2004) Postoperative intraocular pressure spikes: the need to treat. Eye (Lond) 18(7):673–679. https://doi.org/10.1038/sj.eye.6701319
Zhu Y, Ohlemiller KK, McMahan BK, Gidday JM (2002) Mouse models of retinal ischemic tolerance. Invest Ophthalmol Vis Sci 43(6):1903–1911
Kong YX, Crowston JG, Vingrys AJ, Trounce IA, Bui VB (2009) Functional changes in the retina during and after acute intraocular pressure elevation in mice. Invest Ophthalmol Vis Sci 50(12):5732–5740. https://doi.org/10.1167/iovs.09-3814
Xu N, Tang XH, Pan W, Xie ZM, Zhang GF, Ji MH, Yang JJ, Zhou MT, Zhou ZQ (2017) Spared nerve injury increases the expression of microglia M1 markers in the prefrontal cortex of rats and provokes depression-like behaviors. Front Neurosci 11:209. https://doi.org/10.3389/fnins.2017.00209
Erickson KK, Sundstrom JM, Antonetti DA (2007) Vascular permeability in ocular disease and the role of tight junctions. Angiogenesis 10(2):103–117. https://doi.org/10.1007/s10456-007-9067-z
Başoğlu MS, Eren E, Aslan H, Kolatan HE, Özbay C, İnan S, Karaca F, Öztürkcan S, Katılmış H (2012) Increased expression of VEGF, iNOS, IL-1β, and IL-17 in a rabbit model of gastric content-induced middle ear inflammation. Int J Pediatr Otorhinolaryngol 76(1):64–69. https://doi.org/10.1016/j.ijporl.2011.10.001
Nejad M, Injev VP, Miller KM (2012) Laboratory analysis of phacoemulsifier compliance and capacity. J Cataract Refract Surg 38(11):2019–2028. https://doi.org/10.1016/j.jcrs.2012.05.046
Sharif-Kashani P, Fanney D, Injev V (2014) Comparison of occlusion break responses and vacuum rise times of phacoemulsification systems. BMC Ophthalmol 14:96. https://doi.org/10.1186/1471-2415-14-96
Thorne A, Dyk DW, Fanney D, Miller KM (2018) Phacoemulsifier occlusion break surge volume reduction. J Cataract Refract Surg 44(12):1491–1496. https://doi.org/10.1016/j.jcrs.2018.01.032
Minami M, Oku H, Okuno T, Fukuhara M, Ikeda T (2007) High infusion pressure in conjunction with vitreous surgery alters the morphology and function of the retina of rabbits. Acta Ophthalmol Scand 85(6):633–639. https://doi.org/10.1111/j.1600-0420.2007.00919.x
Streit WJ, Conde JR, Fendrick SE, Flanary BE, Mariani CL (2005) Role of microglia in the central nervous system's immune response. Neurol Res 27(7):685–691. https://doi.org/10.1179/016164105x49463
Ramirez AI, de Hoz R, Salobrar-Garcia E, Salazar JJ, Rojas B, Ajoy D, López-Cuenca I, Rojas P, Triviño A, Ramírez JM (2017) The role of microglia in retinal neurodegeneration: Alzheimer's disease, Parkinson, and glaucoma. Front Aging Neurosci 9:214. https://doi.org/10.3389/fnagi.2017.00214
Chen H, Cho KS, Vu THK, Shen CH, Kaur M, Chen G, Mathew R, McHam ML, Fazelat A, Lashkari K, Au NPB, Tse JKY, Li Y, Yu H, Yang L, Stein-Streilein J, Ma CHE, Woolf CJ, Whary MT, Jager MJ, Fox JG, Chen J, Chen DF (2018) Commensal microflora-induced T cell responses mediate progressive neurodegeneration in glaucoma. Nat Commun 9(1):3209. https://doi.org/10.1038/s41467-018-05681-9
Trible JR, Anderson DR (1997) Factors associated with intraocular pressure-induced acute visual field depression. Arch Ophthalmol 115(12):1523–1527. https://doi.org/10.1001/archopht.1997.01100160693005
Bui BV, Edmunds B, Cioffi GA, Fortune B (2005) The gradient of retinal functional changes during acute intraocular pressure elevation. Invest Ophthalmol Vis Sci 46(1):202–213. https://doi.org/10.1167/iovs.04-0421
Pfeiffer F, Schafer J, Lyck R, Makrides V, Brunner S, Schaeren-Wiemers N, Deutsch U, Engelhardt B (2011) Claudin-1 induced sealing of blood-brain barrier tight junctions ameliorates chronic experimental autoimmune encephalomyelitis. Acta Neuropathol 122(5):601–614. https://doi.org/10.1007/s00401-011-0883-2
Murakami T, Frey T, Lin C, Antonetti DA (2012) Protein kinase cβ phosphorylates occludin regulating tight junction trafficking in vascular endothelial growth factor-induced permeability in vivo. Diabetes 61(6):1573–1583. https://doi.org/10.2337/db11-1367
Gardner TW, Antonetti DA, Barber AJ, LaNoue KF, Levison SW (2002) Diabetic retinopathy: more than meets the eye. Surv Ophthalmol 47(Suppl 2):S253–262. https://doi.org/10.1016/s0039-6257(02)00387-9
Kniesel U, Wolburg H (2000) Tight junctions of the blood-brain barrier. Cell Mol Neurobiol 20(1):57–76. https://doi.org/10.1023/a:1006995910836
Antonetti DA, Klein R, Gardner TW (2012) Diabetic retinopathy. N Engl J Med 366(13):1227–1239. https://doi.org/10.1056/NEJMra1005073
Azuara-Blanco A, Harris A, Cantor LB, Abreu MM, Weinland M (1998) Effects of short term increase of intraocular pressure on optic disc cupping. Br J Ophthalmol 82(8):880–883. https://doi.org/10.1136/bjo.82.8.880
Moorhead LC, Armeniades CD (1986) Variations in intraocular pressure during closed-system surgical procedures. Arch Ophthalmol 104(2):269–272. https://doi.org/10.1001/archopht.1986.01050140127034
Armeniades CD, Moorhead LC (1992) Hydrodynamic analysis of intraocular pressure changes during anterior chamber procedures. J Cataract Refract Surg 18(5):444–448. https://doi.org/10.1016/s0886-3350(13)80096-x
Moorhead LC, Gardner TW, Lambert HM, O'Malley RE, Willis AW, Meharg LS, Moorhead WD (2005) Dynamic intraocular pressure measurements during vitrectomy. Arch Ophthalmol 123(11):1514–1523. https://doi.org/10.1001/archopht.123.11.1514
Vasavada AR, Praveen MR, Vasavada VA, Vasavada VA, Raj SM, Asnani PK, Garg VS (2010) Impact of high and low aspiration parameters on postoperative outcomes of phacoemulsification: randomized clinical trial. J Cataract Refract Surg 36(4):588–593. https://doi.org/10.1016/j.jcrs.2009.11.009
Vasavada V, Raj SM, Praveen MR, Vasavada AR, Henderson BA, Asnani PK (2014) Real-time dynamic intraocular pressure fluctuations during microcoaxial phacoemulsification using different aspiration flow rates and their impact on early postoperative outcomes: a randomized clinical trial. J Refract Surg 30(8):534–540. https://doi.org/10.3928/1081597x-20140711-06
Vasavada V, Srivastava S, Vasavada V, Vasavada S, Vasavada AR, Sudhalkar A, Bilgic A (2019) Impact of fluidic parameters during phacoemulsification on the anterior vitreous face behavior: experimental study. Indian J Ophthalmol 67(10):1634–1637. https://doi.org/10.4103/ijo.IJO_465_19
Miami Study Group (1979) Cystoid macular edema in aphakic and pseudophakic eyes. Am J Ophthalmol 88(1):45–48. https://doi.org/10.1016/0002-9394(79)90751-7
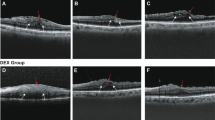
Perente I, Utine CA, Ozturker C, Cakir M, Kaya V, Eren H, Kapran Z, Yilmaz OF (2007) Evaluation of macular changes after uncomplicated phacoemulsification surgery by optical coherence tomography. Curr Eye Res 32(3):241–247. https://doi.org/10.1080/02713680601160610
Sari ES, Ermis SS, Yazici A, Koytak A, Sahin G, Kilic A (2014) The effect of intracameral anesthesia on macular thickness and ganglion cell-inner plexiform layer thickness after uneventful phacoemulsification surgery: prospective and randomized controlled trial. Graefes Arch Clin Exp Ophthalmol 252(3):433–439. https://doi.org/10.1007/s00417-013-2557-3
Walkden A, Porter LF, Morarji J, Kelly SP, Sioras E (2017) Pseudophakic cystoid macular edema and spectral-domain optical coherence tomography-detectable central macular thickness changes with perioperative prostaglandin analogs. J Cataract Refract Surg 43(8):1027–1030. https://doi.org/10.1016/j.jcrs.2017.05.029
Song WM, Colonna M (2018) The identity and function of microglia in neurodegeneration. Nat Immunol 19(10):1048–1058. https://doi.org/10.1038/s41590-018-0212-1
Trost A, Motloch K, Bruckner D, Schroedl F, Bogner B, Kaser-Eichberger A, Runge C, Strohmaier C, Klein B, Aigner L, Reitsamer HA (2015) Time-dependent retinal ganglion cell loss, microglial activation and blood-retina-barrier tightness in an acute model of ocular hypertension. Exp Eye Res 136:59–71. https://doi.org/10.1016/j.exer.2015.05.010
Chen M, Luo C, Zhao J, Devarajan G, Xu H (2019) Immune regulation in the aging retina. Prog Retin Eye Res 69:159–172. https://doi.org/10.1016/j.preteyeres.2018.10.003
Rathnasamy G, Foulds WS, Ling EA, Kaur C (2019) Retinal microglia—a key player in healthy and diseased retina. Prog Neurobiol 173:18–40. https://doi.org/10.1016/j.pneurobio.2018.05.006
Okunuki Y, Mukai R, Nakao T, Tabor SJ, Butovsky O, Dana R, Ksander BR, Connor KM (2019) Retinal microglia initiate neuroinflammation in ocular autoimmunity. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.1820387116
Klaassen I, Van Noorden CJ, Schlingemann RO (2013) Molecular basis of the inner blood-retinal barrier and its breakdown in diabetic macular edema and other pathological conditions. Prog Retin Eye Res 34:19–48. https://doi.org/10.1016/j.preteyeres.2013.02.001
McCulley TJ, Lam BL, Feuer WJ (2001) Incidence of nonarteritic anterior ischemic optic neuropathy associated with cataract extraction. Ophthalmology 108(7):1275–1278. https://doi.org/10.1016/s0161-6420(01)00631-5
Nguyen LT, Taravella MJ, Pelak VS (2006) Determining whether delayed nonarteritic ischemic optic neuropathy associated with cataract extraction is a true entity. J Cataract Refract Surg 32(12):2105–2109. https://doi.org/10.1016/j.jcrs.2006.08.028
Sharma S, Tun TA, Baskaran M, Atalay E, Thakku SG, Liang Z, Milea D, Strouthidis NG, Aung T, Girard MJ (2018) Effect of acute intraocular pressure elevation on the minimum rim width in normal, ocular hypertensive and glaucoma eyes. Br J Ophthalmol 102(1):131–135. https://doi.org/10.1136/bjophthalmol-2017-310232
Nicoli CM, Dimalanta R, Miller KM (2016) Experimental anterior chamber maintenance in active versus passive phacoemulsification fluidics systems. J Cataract Refract Surg 42(1):157–162. https://doi.org/10.1016/j.jcrs.2015.08.017
Solomon KD, Lorente R, Fanney D, Cionni RJ (2016) Clinical study using a new phacoemulsification system with surgical intraocular pressure control. J Cataract Refract Surg 42(4):542–549. https://doi.org/10.1016/j.jcrs.2016.01.037
Pareja-Esteban J, Teus-Guezala MA, Drake-Casanova P, Dapena-Sevilla I (2009) Retinal nerve fiber layer changes after cataract surgery measured by OCT: a pilot study. Arch Soc Esp Oftalmol 84(6):305–309
Kok PHB, van den Berg TJTP, van Dijk HW, Stehouwer M, van der Meulen IJE, Mourits MP, Verbraak FD (2013) The relationship between the optical density of cataract and its influence on retinal nerve fibre layer thickness measured with spectral domain optical coherence tomography. Acta Ophthalmol 91(5):418–424. https://doi.org/10.1111/j.1755-3768.2012.02514.x
Dada T, Behera G, Agarwal A, Kumar S, Sihota R, Panda A (2010) Effect of cataract surgery on retinal nerve fiber layer thickness parameters using scanning laser polarimetry (GDxVCC). Indian J Ophthalmol 58(5):389–394. https://doi.org/10.4103/0301-4738.67048
Mwanza JC, Bhorade AM, Sekhon N, McSoley JJ, Yoo SH, Feuer WJ, Budenz DL (2011) Effect of cataract and its removal on signal strength and peripapillary retinal nerve fiber layer optical coherence tomography measurements. J Glaucoma 20(1):37–43. https://doi.org/10.1097/IJG.0b013e3181ccb93b
El-Ashry M, Appaswamy S, Deokule S, Pagliarini S (2006) The effect of phacoemulsification cataract surgery on the measurement of retinal nerve fiber layer thickness using optical coherence tomography. Curr Eye Res 31(5):409–413
Funding
These research was support by Guangzhou Science and Technology Plan Project (Grant number: 201803040020, 201903010065; Guangzhou, China), Guangdong Natural Science Foundation (Grant number: 2020A151501168; Guangzhou, China) and Research Funds of the State Key Laboratory of Ophthalmology (Grant numbers: PT1001022).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by ZZ, XY, and NS. The first draft of the manuscript was written by ZZ and XY, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All experiments are performed in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research, and the experimental protocol was approved by the Ethics Committee of Zhongshan Ophthalmology center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhao, Z., Yu, X., Yang, X. et al. Elevated intraocular pressure causes cellular and molecular retinal injuries, advocating a more moderate intraocular pressure setting during phacoemulsification surgery. Int Ophthalmol 40, 3323–3336 (2020). https://doi.org/10.1007/s10792-020-01519-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01519-w