Abstract
Purpose
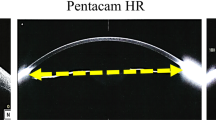
To investigate the reliability of using anterior segment optical coherence tomography (AS-OCT) to measure the lower lid margin thickness (LLMT) from the posterior lash line to the Marx’s line by comparing with a vernier micrometer.
Methods
This was a prospective, single-center, diagnostic test study. Sixty volunteers aged between 20 and 79 without ocular diseases were recruited. A vernier micrometer and AS-OCT were, respectively, used to measure the same lid margin thickness at the central lower lid.
Results
The mean age of volunteers was 39.1 ± 13.7 years. The LLMT in 60 subjects (25 males and 35 females) measured by a vernier micrometer and AS-OCT was 1.03 ± 0.25 mm and 0.82 ± 0.21 mm, respectively. There was a significant difference between two measurements (P < 0.001). In addition, intraclass correlation coefficient (ICC) was engaged to evaluate the reliability and agreement of two measurements (ICC = 0.83). Bland–Altman plots demonstrated that 57 of 60 spots were within 95% limits of agreement. No adverse events were detected in all subjects after the measurements.
Conclusion
Although the LLMT measured by AS-OCT was less than that measured by a vernier micrometer, AS-OCT providing quantitative measurements and imaging data was also seemed to be a reliable method with a good agreement. It could be a substitute for a vernier micrometer in clinical practice in the future.




Similar content being viewed by others
References
Nelson JD, Shimazaki J, Benitez-del-Castillo JM et al (2011) The international workshop on meibomian gland dysfunction:report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci 52:1930–1937
Foulks GN, Bron AJ (2003) Meibomian gland dysfunction: a clinical scheme for description, diagnosis, classification, and grading. Ocul Surf 1:107–126
Bron AJ, Benjamin L, Snibson GR (1991) Meibomian gland disease. Classification and grading of lid changes. Eye 5:395–411
Tomlinson A, Bron AJ, Korb DR et al (2011) The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Vis Sci 52:2006–2049
Asia Dry Eye Association China Branch, Ocular Surface and Tear Disease Group of Ophthalmology Specialized Committee of the Cross-Strait Medical Exchange Association (2017) Chinese expert consensus on the diagnosis and treatment of meibomian gland dysfunction. Zhonghua Yan Ke Za Zhi 53:657–661 (inChinese)
Shimazaki J, Sakata M, Tsubota K (1995) Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch Ophthalmol 113:1266–1270
Goto E, Monden Y, Takano Y et al (2002) Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. Br J Ophthalmol 86:1403–1407
Nichols KK (2011) The international workshop on meibomian gland dysfunction: introduction. Invest Ophthalmol Vis Sci 52:1917–1921
Lin PY, Tsai SY, Cheng CY et al (2003) Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 110:1096–1101
Lekhanont K, Rojanaporn D, Chuck RS et al (2006) Prevalence of dry eye in Bangkok, Thailand. Cornea 25:1162–1167
Jie Y, Xu L, Wu YY et al (2009) Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye 23:688–693
Den S, Shimizu K, Ikeda T et al (2006) Association between meibomian gland changes and aging, sex, or tear function. Cornea 25:651–655
Arita R, Itoh K, Inoue K et al (2008) Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 115:911–915
Gupta PK, Stevens MN, Kashyap N et al (2018)Prevalence of meibomian gland atrophy in a pediatric population. Cornea 37:426–430
Wang X, Lu X, Yang J et al (2016) Evaluation of dry eye and meibomian gland dysfunction in teenagers with myopia through noninvasive keratograph. J Ophthalmol 2016:6761206
Mizoguchi T, Arita R, Fukuoka S et al (2017) Morphology and function of meibomian glands and other tear film parameters in junior high school students. Cornea 36:922–926
Hykin PG, Bron AJ (1992) Age-related morphological changes in lid margin and meibomian gland anatomy. Cornea 11:334–342
He L (1982) Measurement of the thickness of the normal lid margin in Chinese. Zhonghua Yan Ke Za Zhi 18:178 (in Chinese)
Pult H, Korb DR, Murphy PJ et al (2015) A new model of central lid margin apposition and tear film mixing in spontaneous blinking. Cont Lens Anterior Eye 38:173–180
Huang D, Swanson EA, Lin CP et al (1991) Optical coherence tomography. Science 254:1178–1181
Ang M, Baskaran M, Werkmeister RM et al (2018) Anterior segment optical coherence tomography. Prog Retin Eye Res 66:132–156
Park DI, Shin HM, Lee SY et al (2013) Tear production and drainage after botulinum toxin A injection in patients with essential blepharospasm. Acta Ophthalmol 91:e108–112
Grosvenor T (1978) Etiology of astigmatism. Am J Optom Physiol Opt 55:214–218
Anstice J (1971) Astigmatism-its components and their changes with age. Am J Optom Arch Am Acad Optom 48:1001–1006.
Baldwin WR, Mills D (1981) A longitudinal study of corneal astigmatism and total astigmatism. Am J Optom Physiol Opt 58:206–211
Collins MJ, Buehren T, Trevor T et al (2006) Factors influencing lid pressure on the cornea. Eye Contact Lens 32:168–173
Shaw AJ, Collins MJ, Davis BA et al (2008) Corneal refractive changes due to short-term eyelid pressure in downward gaze. J Cataract Refract Surg 34:1546–1553
Shaw AJ, Collins MJ, Davis BA et al (2009) Eyelid pressure: inferences from corneal topographic changes. Cornea 28:181–188
Yamaguchi M, Shiraishi A (2018) Relationship Between Eyelid Pressure and Ocular Surface Disorders in Patients With Healthy and Dry Eyes. Invest Ophthalmol Vis Sci 59:DES56-DES63.
Murube J (2005) Characteristics and etiology of conjunctivochalasis: historical perspective. Ocul Surf 3:7–14
Marmalidou A, Kheirkhah A, Dana R (2018) Conjunctivochalasis: a systematic review. Surv Ophthalmol 63:554–564
Yamamoto Y, Shiraishi A, Sakane Y et al (2016) Involvement of eyelid pressure in lid-wiper epitheliopathy. Curr Eye Res 41:171–178
Namiguchi K, Mizoue S, Ohta K et al (2018) Effect of botulinum toxin A treatment on eyelid pressure in eyes with blepharospasm. Curr Eye Res 43:896–901
Young G, Hunt C, Covey M (2002) Clinical evaluation of factors influencing toric soft contact lens fit. Optom Vis Sc 79:11–19
Holden BA, Stephenson A, Stretton S et al (2001) Superior epithelial arcuate lesions with soft contact lens wear. Optom Vis Sci 78:9–12
Cher I (2003) Blink-related microtrauma: when the ocular surface harms itself. Clin Experiment Ophthalmol 31:183–190
Kim J, Lee SM, Choi YJ et al (2018) Estimation of eyelid pressure using a Blepharo-Tensiometer in patients with functional nasolacrimal duct obstruction. J Ophthalmol 2018:8792102
Wang DH, Liu XQ, Hao XJ et al (2018) Effect of the meibomian gland squeezer for treatment of meibomian gland dysfunction. Cornea 37:1270–1278
Norn M (1985) Meibomian orifices and Marx’s line: studied by triple vital staining. Acta Ophthalmol 63:698–700
Donald C, Hamilton L, Doughty MJ (2003) A quantitative assessment of the location and width of Marx's line along the marginal zone of the human eyelid. Optom Vis Sci 80:564–572
Shaw AJ, Collins MJ, Davis BA et al (2010) Eyelid pressure and contact with the ocular surface. Invest Ophthalmol Vis Sci 51:1911–1917
Knop E, Knop N, Zhivov A et al (2011) The lid wiper and muco-cutaneous junction anatomy of the human eyelid margins: an in vivo confocal and histological study. J Anat 218:449–461
Knop N, Korb DR, Blackie CA et al (2012) The lid wiper contains goblet cells and goblet cell crypts for ocular surface lubrication during the blink. Cornea 31:668–679
Doughty MJ (2013) Morphological features of cells along Marx's line of the marginal conjunctiva of the human eyelid. Clin Exp Optom 96:76–84
Acknowledgements
This work was supported by the National Natural Science Foundation of China (grant number: 81574028). We would like to acknowledge Xiao Wang and Cecilia Zhang for their help in language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Da-Hu Wang conceived and designed the study, with input from Jie Yao and Xin-Quan Liu. Da-Hu Wang and Jie Yao analyzed the data and wrote the initial manuscript draft. Xin-Quan Liu actively reviewed and revised the manuscript, and approved the final submitted manuscript. The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 41337 kb)
Rights and permissions
About this article
Cite this article
Wang, DH., Yao, J. & Liu, XQ. Comparison of two measurements for the lower lid margin thickness: vernier micrometer and anterior segment optical coherence tomography. Int Ophthalmol 40, 3223–3232 (2020). https://doi.org/10.1007/s10792-020-01505-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01505-2