Abstract
Background
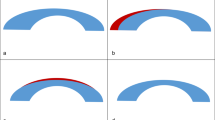
Attention is usually given to inferior steepening on corneal topography in the evaluation of a patient’s suitability for LASIK surgery. The aim of this study is to investigate long-term refractive results with superior steepening.
Methods
Patients who underwent LASIK surgery between 2015 and 2019 in our refractive surgery department were retrospectively reviewed. The patients with a ≥ 1.0 D superior–inferior (S–I) quadrant difference in the tangential map, using a Scheimpflug camera with a Placido disc topographer (Sirius), were included in the study. Preoperative and postoperative best-corrected and uncorrected visual acuity (Snellen), cylindrical refraction values, and spherical equivalent (SE) values were compared. Adverse events were recorded.
Results
Fifty eyes of 28 patients participated in the study. The mean age of the patients was 27.5 ± 8.0 (19–59). Sixteen patients were female (57.1%), and 12 (42.8%) patients were male. The average follow-up time was 29.8 ± 11.1 months (12–61). Average central corneal thickness was 549.4 ± 26.0 (498–602) μm. Average minimal corneal thickness was 549.1 ± 26.9 (497–598) μm. Preoperative S–I quadrant difference (D) was 1.87 ± 0.7 (1.0–3.99). Posterior elevation (Kvb) was 11.2 ± 1.9 (9–17) μm. The preoperative SE value was − 1.7 ± 2.1 (− 6.25–3.25) and improved to − 0.3 ± 0.44 D (− 1.25–0.75) (p < 0.001). Preoperative cylindrical refraction values were − 2.04 ± 1.7 (− 6.25–0), and postoperative values were − 0.47 ± 0.4 (− 2–0) D (p < 0.001). Uncorrected visual acuity was median 1.0 (0.4–1.0) with 38 eyes (76%) having 20/20 postoperative uncorrected visual acuity. No sight threatening complications or ectasia findings were observed during the 2 years postoperative follow-up time.
Conclusions
Abnormal corneal topographies with (S–I) asymmetry result in predictable results after LASIK.






Similar content being viewed by others
References
Taneri S, Weisberg M, Azar DT (2011) Surface ablation techniques. J Cataract Refract Surg 37:392–408
Sutton GL, Kim P (2010) Laser in situ keratomileusis in 2010—a review. Clin Exp Ophthalmol 38:192–210
Holland SP, Srivannaboon S, Reinstein DZ (2000) Avoiding serious corneal complications of laser assisted in situ keratomileusis and photorefractive keratectomy. Ophthalmol 107:640–652
Mannis MJ, Segal WA, Darlington JK (2001) Making sense of refractive surgery in 2001: why, when, for whom, and by whom? Mayo Clin Proc 76:823–829
Mannis MJ, Zadnik K, Johnson CA (1984) The effect of penetrating keratoplasty on contrast sensitivity in keratoconus. Arch Ophthalmol 102:1513–1516
Wang Y, Rabinowitz YS, Rotter JI, Yang H (2000) Genetic epidemiological study of keratoconus: evidence for major gene determination. Am J Med Genet 28:403–409
Holladay JT, Dudeja DR, Chang J (1999) Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg 25:663–669
Rabinowitz YS, Rasheed K (1999) KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg 25:1327–1335
Schor P, Beer SM, da Silva O et al (2003) A clinical follow-up of PRK and LASIK in eyes with preoperative abnormal corneal topographies. Br J Ophthalmol 87:682–685
Gortzak R, Rosen S, Weitzman S et al (2002) Videokeratography findings in children with vernal keratoconjunctivitis versus those of healthy children. Ophthalmol 109:2018–2023C
Markomanolakis MM, Kymionis GD, Aslanides IM et al (2005) Induced videokeratography alterations in patients with excessive meibomian secretions. Cornea 24:16–19
Kymionis GD, Kankariya VP, Grentzelos MA et al (2012) Outcomes of refractive surgery in patients with topographic superior corneal steepening. J Refract Surg 28:462–467
Seiler T, Koufala K, Richter G (1998) Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg 14:312–317
Randleman JB, Russell B, Ward MA et al (2003) Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmol 110:267–275
Rabinowitz YS (1998) Keratoconus. Surv Ophthalmol 42:297–319
Rabinowitz YS, Yang H, Brickman Y et al (1996) Videokeratography database of normal human corneas. Br J Ophthalmol 80:610–616
Varssano D, Kaiserman I, Hazarbassanov R (2004) Topographic patterns in refractive surgery candidates. Cornea 23:602–607
Ruiz-Montenegro J, Mafra CH, Wilson SE et al (1993) Corneal topographic alterations in normal contact lens wearers. Ophthalmol 100:128–134
Kim T, Khosla-Gupta B, Debacker C (2000) Blepharoptosis-induced superior keratoconus. Am J Ophthalmol 130:232–234
Prisant O, Legeais JM, Renard G (1997) Superior keratoconus. Cornea 16:693–694
Alessio G, Boscia F, La Tegola MG et al (2001) Topography-driven excimer laser for the retreatment of decentralized myopic photorefractive keratectomy. Ophthalmol 108:1695–1703
Pop M, Payette Y (2000) Photorefractive keratectomy versus laser in situ keratomileusis: a control-matched study. Ophthalmol 107:251–257
McDonald MB, Deitz MR, Frantz JM et al (1999) Photorefractive keratectomy for low-to-moderate myopia and astigmatism with a small-beam tracker-directed excimer laser. Ophthalmology 106:1481–1488 Discussion 1488–1489
Agarwal S, Thornell E, Hodge C et al (2018) Visual outcomes and higher order aberrations following LASIK on eyes with low myopia and astigmatism. Open Ophthalmol J 12:84–93
Jain AK, Malhotra C, Pasari A et al (2016) Outcomes of topography-guided versus wavefront-optimized laser in situ keratomileusis for myopia in virgin eyes. J Cataract Refract Surg 42:1302–1311
Sridhar MS, Mahesh S, Bansal K et al (2004) Superior pellucid marginal corneal degeneration. Eye 18:393–399
Spadea L, Cantera E, Cortes M, Conocchia NE, Stewart CW (2012) Corneal ectasia after myopic laser in situ keratomileusis: a long-term study. Clin Ophthalmol 6:1801–1813
Pasquali T, Krueger R (2012) Topography-guided laser refractive surgery. Curr Opin Ophthalmol 23(4):264–268. https://doi.org/10.1097/ICU.0b013e328354adf0
Acknowledgements
This study was presented as a poster at the American Society of Cataract and Refractive Surgery (ASCRS) 2018, Washington Meeting.
Funding
No funding was provided for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Okmeydanı Training and Research Hospital Ethic Committee and was carried out in accordance with the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kepez Yildiz, B., Kemer Atik, B., Yildirim, Y. et al. Laser in situ keratomileusis (LASİK) in patients with superior steepening on corneal topography: Is it safe and predictable?. Int Ophthalmol 40, 2353–2359 (2020). https://doi.org/10.1007/s10792-020-01420-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01420-6