Abstract
Background
To report emulsified particles and related complications after removal of silicone oil (SO) by spectral domain-optical coherence tomography (SD-OCT) and fluorescein angiography (FA).
Methods
A prospective, single-center investigation was performed using SD-OCT, FA and flare cell photometry measurements to evaluate in a cohort of eyes with emulsified silicone particles after removal of long-term SO tamponade.
Results
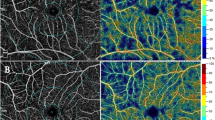
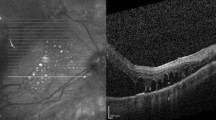
Nineteen eyes of the 19 patients with emulsified silicone particles detected in ophthalmoscopic exam were included in the study: 13 (68%) were male, and 6 (31.6%) were female, and their mean age was 52.75 ± 16.06 years. Preoperative diagnoses were rhegmatogenous retinal detachment in all eyes. The mean duration of the silicone oil’s presence in the eye was found as 12.63 ± 4.87 (7–26) months. SD-OCT examination postoperatively showed small, round and hyper-reflective structures compatible with emulsified silicone particles on preretinal surface in 7 (36.8%) eyes, intraretinally in 6 (31.6%) eyes and in the vitreous in 12 (63%) eyes. FA imaging demonstrated pearl-like hyper-fluorescence at early and late phases on the large blood vessels in 9 (47.4%) eyes. Late phase hyper-fluorescence due to leakage on the macula was observed in 17 (89.5%) eyes. Diffuse peripheral leakage and hyper-fluorescence was detected in 11 (57.9%) eyes. Flare levels were higher in eyes with emulsified SO compared to unaffected fellow eyes (p < 0.05).
Conclusions
Emulsified silicone particles that remain in the eye may lead to retinal complications and inflammation in addition to their known complications such as keratopathy and glaucoma. The particles that lead to inflammation and presence of inflammation may be examined by imaging methods such as SD-OCT and FA. Removing the SO before emulsification would be suitable for avoiding such complications.



Similar content being viewed by others
References
Vaziri K, Schwartz SG, Kishor KS, Flynn HW Jr (2016) Tamponade in the surgical management of retinal detachment. Clin Ophthalmol (Auckland, NZ) 10:471–476. https://doi.org/10.2147/opth.s98529
Feng X, Li C, Zheng Q, Qian XG, Shao W, Li Y, Li W, Yin L, Wang Y, Gao Q (2017) Risk of silicone oil as vitreous tamponade in pars plana vitrectomy: a systematic review and meta-analysis. Retina (Philadelphia, Pa) 37(11):1989–2000. https://doi.org/10.1097/iae.0000000000001553
Miller JB, Papakostas TD, Vavvas DG (2014) Complications of emulsified silicone oil after retinal detachment repair. Semin Ophthalmol 29(5–6):312–318. https://doi.org/10.3109/08820538.2014.962181
Eckle D, Kampik A, Hintschich C, Haritoglou C, Tonn JC, Uhl E, Lienemann A (2005) Visual field defect in association with chiasmal migration of intraocular silicone oil. Br J Ophthalmol 89(7):918–920. https://doi.org/10.1136/bjo.2004.062893
Grzybowski A, Pieczynski J, Ascaso FJ (2014) Neuronal complications of intravitreal silicone oil: an updated review. Acta Ophthalmol 92(3):201–204. https://doi.org/10.1111/aos.12212
Watad A, Quaresma M, Brown S, Cohen Tervaert JW, Rodriguez-Pint I, Cervera R, Perricone C, Shoenfeld Y (2017) Autoimmune/inflammatory syndrome induced by adjuvants (Shoenfeld's syndrome): an update. Lupus 26(7):675–681. https://doi.org/10.1177/0961203316686406
Shaikh S, Egbert PR, Goldblum RS, Wieland MR (2000) Granulomatous local cell reaction to intravitreal silicone. Arch Ophthalmol (Chicago, Ill: 1960) 118(8):1133–1134
Wickham L, Asaria RH, Alexander R, Luthert P, Charteris DG (2007) Immunopathology of intraocular silicone oil: enucleated eyes. Br J Ophthalmol 91(2):253–257. https://doi.org/10.1136/bjo.2006.103564
Chung J, Spaide R (2003) Intraretinal silicone oil vacuoles after macular hole surgery with internal limiting membrane peeling. Am J Ophthalmol 136(4):766–767
Errera MH, Liyanage SE, Elgohary M, Day AC, Wickham L, Patel PJ, Sahel JA, Paques M, Ezra E, Sullivan PM (2013) Using spectral-domain optical coherence tomography imaging to identify the presence of retinal silicone oil emulsification after silicone oil tamponade. Retina (Philadelphia, Pa) 33(8):1567–1573. https://doi.org/10.1097/IAE.0b013e318287d9ea
Januschowski K, Irigoyen C, Pastor JC, Srivastava GK, Romano MR, Heimann H, Stalmans P, Van Keer K, Boden K, Szurman P, Spitzer MS (2018) Retinal toxicity of medical devices used during vitreoretinal surgery: a critical overview. Ophthalmologica 240:236–243. https://doi.org/10.1159/000488504
Romano MR, Xu X, Li KK (2014) Vitreous substitutes: from tamponade effect to intraocular inflammation. BioMed Res Int 2014:159832. https://doi.org/10.1155/2014/159832
Russo A, Morescalchi F, Donati S, Gambicorti E, Azzolini C, Costagliola C, Semeraro F (2018) Heavy and standard silicone oil: intraocular inflammation. Int Ophthalmol 38(2):855–867. https://doi.org/10.1007/s10792-017-0489-3
Semeraro F, Russo A, Morescalchi F, Gambicorti E, Vezzoli S, Parmeggiani F, Romano MR, Costagliola C (2019) Comparative assessment of intraocular inflammation following standard or heavy silicone oil tamponade: a prospective study. Acta Ophthalmol 97(1):e97–e102. https://doi.org/10.1111/aos.13830
Asaria RH, Kon CH, Bunce C, Sethi CS, Limb GA, Khaw PT, Aylward GW, Charteris DG (2004) Silicone oil concentrates fibrogenic growth factors in the retro-oil fluid. Br J Ophthalmol 88(11):1439–1442. https://doi.org/10.1136/bjo.2003.040402
Wickham LJ, Asaria RH, Alexander R, Luthert P, Charteris DG (2007) Immunopathology of intraocular silicone oil: retina and epiretinal membranes. Br J Ophthalmol 91(2):258–262. https://doi.org/10.1136/bjo.2006.103549
Das T, Vedantham V (2004) Intravitreal sodium fluorescein enhances visualization of clear vitreous during vitreous surgery for macular hole: a safety and efficacy study. Clin Exp Ophthalmol 32(1):55–57
Kociok N, Gavranic C, Kirchhof B, Joussen AM (2005) Influence on membrane-mediated cell activation by vesicles of silicone oil or perfluorohexyloctane. Graefe's Arch Clin Exp Ophthalmol 243(4):345–358. https://doi.org/10.1007/s00417-004-1039-z
Odrobina D, Laudanska-Olszewska I (2014) Analysis of the time and location of the silicone oil emulsification by spectral-domain optical coherence tomography after silicone oil tamponade. BioMed Res Int 2014:372045. https://doi.org/10.1155/2014/372045
Liu W, Gao M, Liang X (2018) Management of subfoveal perfluorocarbon liquid: a review. Ophthalmologica 240(1):1–7. https://doi.org/10.1159/000488118
Uji A, Murakami T, Nishijima K, Akagi T, Horii T, Arakawa N, Muraoka Y, Ellabban AA, Yoshimura N (2012) Association between hyperreflective foci in the outer retina, status of photoreceptor layer, and visual acuity in diabetic macular edema. Am J Ophthalmol 153(4):710–717. https://doi.org/10.1016/j.ajo.2011.08.041
Chan YK, Cheung N, Chan WS, Wong D (2015) Quantifying silicone oil emulsification in patients: are we only seeing the tip of the iceberg? Graefe's Arch Clin Exp Ophthalmol 253(10):1671–1675. https://doi.org/10.1007/s00417-014-2866-1
Lo DM, Flaxel CJ, Fawzi AA (2017) Macular effects of silicone oil tamponade: optical coherence tomography findings during and after silicone oil removal. Curr Eye Res 42(1):98–103. https://doi.org/10.3109/02713683.2016.1146776
Gonvers M, Hornung JP, de Courten C (1986) The effect of liquid silicone on the rabbit retina: histologic and ultrastructural study. Arch Ophthalmol 104(7):1057–1062
Funding
This study was not funded by any company.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from the parents of each subject in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cebeci, Z., Sadik, M.T., Ogurel, M.B. et al. Evaluation of emulsified silicone oil with spectral domain-optical coherence tomography and fluorescein angiography. Int Ophthalmol 40, 2267–2274 (2020). https://doi.org/10.1007/s10792-020-01409-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01409-1