Abstract
Purposes
This research aimed to investigate effects and risk factors on non-contact tonometer (NCT) readings in healthy myopic subjects by employing cross-sectional study design.
Methods
Totally, sixty otherwise healthy myopic volunteers (mean 28.4 years old) with 90% female were recruited in ophthalmic clinic. The routine ophthalmic tests, refractive evaluation, examination central corneal thickness (CCT), depth of anterior chamber, axial length, corneal curvature, white-to-white and NCT were assessed at baseline. The linear-mixed model was utilized to evaluate correlation between the readings and ocular biometric parameters.
Results
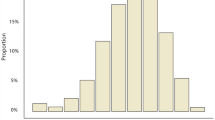
For population in this study, mean spherical equivalents were − 4.85 ± 1.79 diopters in right eyes and − 4.63 ± 1.95 diopters in left eyes. Meanwhile, 28.3% of the eyes had a refractive error exceeding − 6.0 diopters. The mean NCT reading was 15.02 ± 3.02 mmHg in left eyes and 15.33 ± 2.96 mmHg in right eyes. Among the factors analyzed, CCT was the most significant parameter associated with NCT readings. After adjusting for the other factors, per one standard deviation increase of central corneal thickness (36.11 μm) was associated a 1.14 (95% confidence interval 0.53–1.77) mmHg elevated NCT reading. The average central corneal curvature, age and spherical equivalence were also significantly and independently associated with NCT readings.
Conclusions
Central corneal thickness, age, corneal curvature and degree of myopia were independently associated with NCT measured intraocular pressure. Central corneal thickness is one of the most influential factors.
Similar content being viewed by others
References
McMonnies CW (2016) Intraocular pressure and glaucoma: Is physical exercise beneficial or a risk? J Optom 9:139–147
Ornek N, Ornek K, Ogurel T et al (2018) Cystoid macular edema following selective laser trabeculoplasty in a patient with ocular hypertension. Int Ophthalmol 39:1891–1893
Schiefer U, Meisner C, Ziemssen F (2011) 24-Hour intraocular pressure phasing remains an important tool in glaucoma diagnostics. Br J Ophthalmol 95:594
Bang SP, Lee CE, Kim YC (2017) Comparison of intraocular pressure as measured by three different non-contact tonometers and goldmann applanation tonometer for non-glaucomatous subjects. BMC Ophthalmol 17:199
Eksioglu U, Oktem C, Sungur G et al (2018) Outcomes of ahmed glaucoma valve implantation for steroid-induced elevated intraocular pressure in patients with retinitis pigmentosa. Int Ophthalmol 38:1833–1838
Kawai M, Kawai N, Nakabayashi S et al (2017) Comparison of intraocular pressure variability in glaucoma measured by multiple clinicians with those by one clinician. Int Ophthalmol 37:95–101
Gautam N, Kaur S, Kaushik S et al (2016) Postural and diurnal fluctuations in intraocular pressure across the spectrum of glaucoma. Br J Ophthalmol 100:537–541
Myint J, Edgar DF, Kotecha A et al (2011) A national survey of diagnostic tests reported by UK community optometrists for the detection of chronic open angle glaucoma. Ophthalmic Physiol Opt 31:353–359
Ogbuehi KC, Almubrad TM (2008) Accuracy and reliability of the Keeler Pulsair EasyEye non-contact tonometer. Optom Vis Sci 85:61–66
Tsai AS, Aung T, Yip W et al (2016) Relationship of intraocular pressure with central aortic systolic pressure. Curr Eye Res 41:377–382
Rimayanti U, Kiuchi Y, Uemura S et al (2014) Ocular surface displacement with and without contact lenses during non-contact tonometry. PLoS ONE 9:e96066
Jasinskas V, Vaiciuliene R, Varoniukaite A et al (2019) Novel microsurgical management of uveitis–glaucoma–hyphema syndrome. Int Ophthalmol 39:1607–1612
Bilak S, Simsek A, Capkin M et al (2015) Biometric and intraocular pressure change after cataract surgery. Optom Vis Sci 92:464–470
Wang Y, Ched D, Yang W et al (2019) Primary acute angle-closure glaucoma: three-dimensional reconstruction imaging of optic nerve heard structure in based on optical coherence tomography (OCT). Med Sci Monit 25:3647–3654
Shim SH, Sung KR, Kim JM et al (2017) The prevalence of open-angle glaucoma by age in myopia: the Korea national health and nutrition examination survey. Curr Eye Res 42:65–71
Dhingra N, Manoharan R, Gill S et al (2017) Peripapillary schisis in open-angle glaucoma. Eye (London) 31:499–502
Dong YH, Liu HB, Wang ZH et al (2017) Prevalence of myopia and increase trend in children and adolescents aged 7–18 years in Han ethnic group in China, 2005–2014. Zhonghua Liu Xing Bing Xue Za Zhi 38:583–587
Yuan YZ, Feng CL, Li BY et al (2014) The relationship between visual field global indices and retinal nerve fiber layer thickness in healthy myopes. J Ophthalmol 2014:431901
Littell RC, Henry PR, Ammerman CB (1998) Statistical analysis of repeated measures data using SAS procedures. J Anim Sci 76:1216–1231
Wang D, Singh K, Weinreb R et al (2011) Central corneal thickness and related factors in an elderly American Chinese population. Clin Exp Ophthalmol 39:412–420
Saenz-Frances F, Sanz-Pozo C, Borrego-Sanz L et al (2017) Dependence of dynamic contour and goldmann applanation tonometries on peripheral corneal. Int J Ophthalmol 10:1521–1527
Lee M, Ahn J (2016) Effects of central corneal stromal thickness and epithelial thickness on intraocular pressure using Goldmann applanation and non-contact tonometers. PLoS ONE 11:e0151868
Zhang H, Xu L, Chen C et al (2008) Central corneal thickness in adult Chinese. Association with ocular and general parameters. The Beijing Eye Study. Graefes Arch Clin Exp Ophthalmol 246:587–592
Zhang Y, Zhao JL, Bian AL et al (2009) Effects of central corneal thickness and corneal curvature on measurement of intraocular pressure with Goldmann applanation tonometer and non-contact tonometer. Zhonghua Yan Ke Za Zhi 45:713–718
Mansoori T, Balakrishna N (2018) Effect of central corneal thickness on intraocular pressure and comparison of Topcon CT-80 non-contact tonometry with Goldmann applanation tonometry. Clin Exp Optom 101:206–212
Han X, Niu Y, Guo X et al (2016) Age-related changes of intraocular pressure in elderly people in Southern China: Lingtou Eye Cohort Study. PLoS ONE 11:e1051766
Celebi ARC, Kilavuzoglu AE, Altiparmak UE et al (2018) Age-related change in corneal biomechanical parameters in a healthy caucasian population. Ophthalmic Epidemiol 25:55–62
Jordao ML, Lupinacci AP, Ferreira EL et al (2009) Influence of age, central corneal thickness, and quality score on dynamic contour tonometry. Eye (London) 23:1364–1369
Mark HH, Mark TL (2003) Corneal astigmatism in applanation tonometry. Eye (London) 17:617–618
Acknowledgements
This study was granted by the Science and Technology Commission of Shanghai Municipality (Grant No. 11DZ1921206) and Fudan Youth Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no competing financial or commercial interests in this manuscript.
Ethical approval
This research has been approved by the Ethic Committee of Zhongshan Hospital, Fudan University (Shanghai, China). Meanwhile, this study was performed based on the guidance of Declaration of Helsinki. All of subjects have approved this study and provided the written informed consents. This research was taken place from October 2010 to December 2010 in Zhongshan Hospital, Fudan University.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yazhen Ma and Yanping Ma contributed equally to this study.
Rights and permissions
About this article
Cite this article
Ma, Y., Ma, Y., Feng, C. et al. Ocular biometric parameters are associated with non-contact tonometry measured intraocular pressure in non-pathologic myopic patients. Int Ophthalmol 40, 431–437 (2020). https://doi.org/10.1007/s10792-019-01203-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01203-8