Abstract
Purpose
To evaluate different intraocular lens (IOL) designs and to determine whether extended depth of focus (EDOF) lenses provide a higher depth of field (DOF) than the rest considering both subjective and objective measurements.
Methods
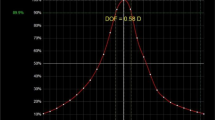
A total of 100 eyes undergoing cataract surgery were divided into six groups depending on the IOL implanted: bifocal designs were Tecnis ZMB and ZLB (Abbott Laboratories, Illinois, USA), trifocal designs were Finevision (PhysIOL, Liège, Belgium) and AT LISA Tri (Carl Zeiss Meditec., Jena, Germany) and EDOF designs were Symfony (Abbott Laboratories, Illinois, USA) and MiniWell (SIFI MedTech, Catania, Italy). Subjective DOF was obtained from defocus curves for the range of vergences which provide a VA over 0.1 LogMAR and 0.2 LogMAR. Aberrometry was measured and Visual Strehl Optical Transference Function (90%) was used to quantify objectively the DOF.
Results
Symfony IOL group showed better subjective and objective DOF compared to the rest of IOL groups, with statistically significant differences (p < 0.001). Comparison between subjective and objective DOF showed that subjective measures were higher for all IOLs, being these differences statistically significant for all groups when compared with objective measures (p < 0.001).
Conclusion
Objective and subjective measures of DOF are not comparable due to differences in methodologies and criterions to define the level of degradation acceptance. Nevertheless, both objective and subjective measures demonstrate a greater DOF for EDOF designs compared to bifocal and trifocal IOLs, being the Symfony IOL the one providing higher levels of subjective and objective DOF.

Similar content being viewed by others
References
Breyer DRH, Kaymak H, Axe T et al (2017) Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia-Pacific J Ophthalmol 6:339–349. https://doi.org/10.22608/APO.2017186
Wang B, Ciuffreda KJ (2006) Depth-of-focus of the human eye: theory and clinical implications. Surv Ophthalmol 51:75–85
Atchison DA, Charman WN, Woods RL (1997) Subjective depth-of-focus of the eye. Optom Vis Sci 74:511–520. https://doi.org/10.1097/00006324-199707000-00019
Leube A, Schilling T, Ohlendorf A et al (2018) Individual neural transfer function affects the prediction of subjective depth of focus. Sci Rep 8:1919. https://doi.org/10.1038/s41598-018-20344-x
Wold JE, Hu A, Chen S, Glasser A (2003) Subjective and objective measurement of human accommodative amplitude. J Cataract Refract Surg 29:1878–1888. https://doi.org/10.1016/S0886-3350(03)00667-9
Gupta N, Wolffsohn JSW, Naroo SA (2008) Optimizing measurement of subjective amplitude of accommodation with defocus curves. J Cataract Refract Surg 34:1329–1338. https://doi.org/10.1016/j.jcrs.2008.04.031
Gupta N, Naroo SA, Wolffsohn JS (2007) Is randomisation necessary for measuring defocus curves in pre-presbyopes? Contact Lens Anterior Eye 30:119–124. https://doi.org/10.1016/j.clae.2007.02.005
Win-Hall DM, Glasser A (2009) Objective accommodation measurements in pseudophakic subjects using an autorefractor and an aberrometer. J Cataract Refract Surg 35:282–290. https://doi.org/10.1016/j.jcrs.2008.10.033
Langenbucher A, Huber S, Nguyen NX et al (2003) Measurement of accommodation after implantation of an accommodating posterior chamber intraocular lens. J Cataract Refract Surg 29:677–685. https://doi.org/10.1016/S0886-3350(02)01893-X
Barišić A, Patel S, Gabric N, Feinbaum CG (2017) The clinical depth of field achievable with trifocal and monofocal intraocular lenses: theoretical considerations and proof of concept clinical results. Graefe’s Arch Clin Exp Ophthalmol 255:367–373. https://doi.org/10.1007/s00417-016-3566-9
Buckhurst PJ, Wolffsohn JS, Naroo SA et al (2012) Multifocal intraocular lens differentiation using defocus curves. Investig Ophthalmol Vis Sci 53:3920–3926. https://doi.org/10.1167/iovs.11-9234
Escandón-García S, Ribeiro FJ, McAlinden C et al (2018) Through-focus vision performance and light disturbances of 3 new intraocular lenses for presbyopia correction. J Ophthalmol. https://doi.org/10.1155/2018/6165493
Ganesh S, Brar S, Pawar A, Relekar KJ (2018) Visual and refractive outcomes following bilateral implantation of extended range of vision intraocular lens with micromonovision. J Ophthalmol 2018:7321794. https://doi.org/10.1155/2018/7321794
Yi F, Iskander DR, Collins MJ (2010) Estimation of the depth of focus from wavefront measurements. J Vis 10:1–9. https://doi.org/10.1167/10.4.3
Tahir HJ, Tong JL, Geissler S et al (2010) Effects of accommodation training on accommodation and depth of focus in an eye implanted with a crystalens intraocular lens. J Refract Surg 26:772–779. https://doi.org/10.3928/1081597X-20100921-02
Pérez-Merino P, Birkenfeld J, Dorronsoro C et al (2014) Aberrometry in patients implanted with accommodative intraocular lenses. Am J Ophthalmol 157:1077–1089. https://doi.org/10.1016/j.ajo.2014.02.013
Marsack JD, Thibos LN, Applegate RA (2004) Metrics of optical quality derived from wave aberrations predict visual performance. J Vis 4:8. https://doi.org/10.1167/4.4.8
Molebna O, Molebny S, Robert Iskander D, et al (2014) Objective DoF measurement based on through-focus augmented VSOTF. Conference: 7th European coinciding with the 1st World Meeting in Visual and Physiological Optics, At Wroclaw, Poland
Marcos S, Moreno E, Navarro R (1999) The depth-of-field of the human eye from objective and subjective measurements. Vis Res 39:2039–2049. https://doi.org/10.1016/S0042-6989(98)00317-4
Castillo Gómez A, Verdejo del Rey A, Palomino Bautista C et al (2012) Principles and clinical applications of ray-tracing aberrometry. Emmetropia 999:96–110
Atchison DA, Fisher SW, Pedersen CA, Ridall PG (2005) Noticeable, troublesome and objectionable limits of blur. Vis Res 45:1967–1974. https://doi.org/10.1016/j.visres.2005.01.022
Woods RL, Colvin CR, Vera-Diaz FA, Peli E (2010) A relationship between tolerance of blur and personality. Investig Ophthalmol Vis Sci 51:6077–6082. https://doi.org/10.1167/iovs.09-5013
Kamlesh Dadeya S, Kaushik S (2001) Contrast sensitivity and depth of focus with aspheric multifocal versus conventional monofocal intraocular lens. Can J Ophthalmol 36:197–201. https://doi.org/10.1016/S0008-4182(01)80040-5
Post CT (1992) Comparison of depth of focus and low-contrast acuities for monofocal versus multifocal intraocular lens patients at 1 year. Ophthalmology 99:1658–1664. https://doi.org/10.1016/S0161-6420(92)31735-X
Langenbucher A, Seitz B, Huber S et al (2003) Theoretical and measured pseudophakic accommodation after implantation of a new accommodative posterior chamber intraocular lens. Arch Ophthalmol 121:1722–1727. https://doi.org/10.1001/archopht.121.12.1722
Domínguez-Vicent A, Esteve-Taboada JJ, Del Águila-Carrasco AJ et al (2016) In vitro optical quality comparison between the Mini WELL ready progressive multifocal and the TECNIS Symfony. Graefe’s Arch Clin Exp Ophthalmol 254:1387–1397. https://doi.org/10.1007/s00417-015-3240-7
Chang M, Kang S-Y, Kim HM (2012) Which keratometer is most reliable for correcting astigmatism with toric intraocular lenses? Korean J Ophthalmol 26:10. https://doi.org/10.3341/kjo.2012.26.1.10
Knorz MC, Claessens D, Schaefer RC et al (1993) Evaluation of contrast acuity and defocus curve in bifocal and monofocal intraocular lenses. J Cataract Refract Surg 19:513–523. https://doi.org/10.1016/S0886-3350(13)80616-5
Sergienko NM, Kondratenko YN, Tutchenko NN (2008) Depth of focus in pseudophakic eyes. Graefe’s Arch Clin Exp Ophthalmol 246:1623–1627. https://doi.org/10.1007/s00417-008-0923-3
Marsack JD, Thibos LN, Applegate RA (2004) Metrics of optical quality derived from wave aberrations predict visual performance. J Vis 4:322–328. https://doi.org/10.1167/4.4.8
Win-Hall DM, Glasser A (2008) Objective accommodation measurements in prepresbyopic eyes using an autorefractor and an aberrometer. J Cataract Refract Surg 34:774–784. https://doi.org/10.1016/j.jcrs.2007.12.033
Marcos S, Navarro R, Ferro M (1995) Through focus image quality of eyes implanted with monofocal and multifocal intraocular lenses. Opt Eng 34:772–779. https://doi.org/10.1117/12.191818
Wolffsohn JS, Naroo SA, Motwani NK et al (2006) Subjective and objective performance of the Lenstec KH-3500 “accommodative” intraocular lens. Br J Ophthalmol 90:693–696. https://doi.org/10.1136/bjo.2006.090951
Ciuffreda KJ, Wang B, Vasudevan B (2007) Conceptual model of human blur perception. Vis Res 47:1245–1252. https://doi.org/10.1016/j.visres.2006.12.001
Funding
The author David P Piñero has been supported by the Ministry of Economy, Industry and Competitiveness of Spain within the program Ramón y Cajal, RYC-2016-20471. The rest of the authors have not received funding for performing this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (CEIm-FJD) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclosure
The authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Palomino-Bautista, C., Sánchez-Jean, R., Carmona-González, D. et al. Subjective and objective depth of field measures in pseudophakic eyes: comparison between extended depth of focus, trifocal and bifocal intraocular lenses. Int Ophthalmol 40, 351–359 (2020). https://doi.org/10.1007/s10792-019-01186-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01186-6