Abstract
Purpose
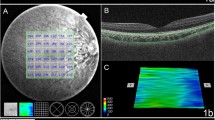
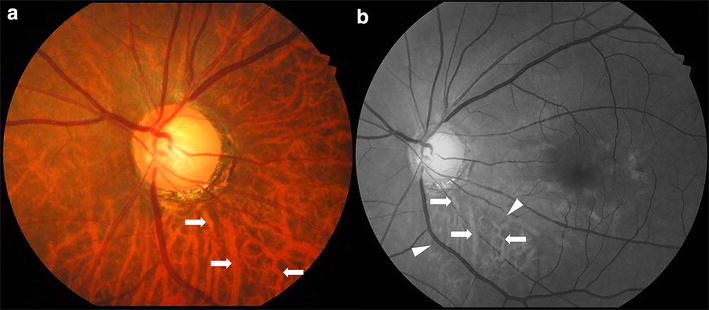
A role of the choroid has been suggested in the pathophysiology of angle closure. We assessed the choroidal thickness (CT) in Caucasian patients with primary angle closure (PAC) and in a subgroup of patients with plateau iris using swept-source optical coherence tomography (SS-OCT) compared to normal eyes.
Methods
This prospective cohort study in a hospital-based population in a tertiary center compared consecutive patients with PAC to healthy controls. A subgroup analysis of patients with plateau iris was also performed. Choroidal thickness was measured by SS-OCT in the subfoveal area (SFCT) and at 1- and 3-mm eccentricity superiorly, inferiorly, nasally and temporally from the fovea.
Results
Compared to the 25 eyes of 13 control patients [7 women, mean (SD) age, 56.6 (15.7) years], the 45 eyes of 25 patients with PAC [15 women, mean (SD) age, 55.7 (10.7) years] had a significantly increased SFCT. SFCT was 355.36 μm (SD 85.97) in PAC eyes versus 286.08 μm (SD 98.09) in control eyes (p = 0.009). The CT was also significantly increased compared to control eyes in other macular areas (p < 0.05), except at 3 mm temporal to the fovea. In the plateau iris subgroup, a not significant (except 3 mm nasal to the fovea) trend toward an increased CT was observed in all studied macular areas compared to control eyes.
Conclusion
In eyes of Caucasian patients with PAC, the CT is increased compared to controls. Increased CT could contribute to the pathophysiology of PAC with a possible choroidal expansion and dysfunction of choroidal ganglion cells.

Similar content being viewed by others
References
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90:262–267. https://doi.org/10.1136/bjo.2005.081224
Cheng J-W, Zong Y, Zeng Y-Y, Wei R-L (2014) The prevalence of primary angle closure glaucoma in adult Asians: a systematic review and meta-analysis. PLoS ONE 9:e103222. https://doi.org/10.1371/journal.pone.0103222
Day AC, Baio G, Gazzard G et al (2012) The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. Br J Ophthalmol 96:1162–1167. https://doi.org/10.1136/bjophthalmol-2011-301189
Kumar G, Bali SJ, Panda A et al (2012) Prevalence of plateau iris configuration in primary angle closure glaucoma using ultrasound biomicroscopy in the Indian population. Indian J Ophthalmol 60:175–178. https://doi.org/10.4103/0301-4738.95865
Mansoori T, Sarvepally VK, Balakrishna N (2016) Plateau iris in primary angle closure glaucoma: an ultrasound biomicroscopy study. J Glaucoma 25:e82–86. https://doi.org/10.1097/IJG.0000000000000263
Mizoguchi T, Ozaki M, Wakiyama H, Ogino N (2015) Plateau iris in Japanese patients with primary angle closure and primary angle closure glaucoma. Clin Ophthalmol Auckl NZ 9:1159–1163. https://doi.org/10.2147/OPTH.S80724
Leeungurasatien T, Radhakrishnan S, Porco T et al (2012) Plateau iris in Whites versus Asians. Eye Sci 27:13–18. https://doi.org/10.3969/j.issn.1000-4432.2012.01.003
George R, Paul PG, Baskaran M et al (2003) Ocular biometry in occludable angles and angle closure glaucoma: a population based survey. Br J Ophthalmol 87:399–402
Chen Y-Y, Chen Y-Y, Sheu S-J, Chou P (2013) The biometric study in different stages of primary angle-closure glaucoma. Eye 27:1070–1076. https://doi.org/10.1038/eye.2013.127
Congdon NG, Youlin Q, Quigley H et al (1997) Biometry and primary angle-closure glaucoma among Chinese, white, and black populations. Ophthalmology 104:1489–1495
Quigley HA, Friedman DS, Congdon NG (2003) Possible mechanisms of primary angle-closure and malignant glaucoma. J Glaucoma 12:167–180
Copete S, Flores-Moreno I, Montero JA et al (2014) Direct comparison of spectral-domain and swept-source OCT in the measurement of choroidal thickness in normal eyes. Br J Ophthalmol 98:334–338. https://doi.org/10.1136/bjophthalmol-2013-303904
Tan CS, Cheong KX, Lim LW, Sadda SR (2016) Comparison of macular choroidal thicknesses from swept source and spectral domain optical coherence tomography. Br J Ophthalmol 100:995–999. https://doi.org/10.1136/bjophthalmol-2015-307541
Hirata M, Tsujikawa A, Matsumoto A et al (2011) Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 52:4971–4978. https://doi.org/10.1167/iovs.11-7729
Zhou M, Wang W, Huang W et al (2014) Is increased choroidal thickness association with primary angle closure? Acta Ophthalmol (Copenh) 92:e514–520. https://doi.org/10.1111/aos.12403
Li Z, Wang W, Zhou M et al (2015) Enhanced depth imaging-optical coherence tomography of the choroid in moderate and severe primary angle-closure glaucoma. Acta Ophthalmol (Copenh) 93:e349–355. https://doi.org/10.1111/aos.12616
Arora KS, Jefferys JL, Maul EA, Quigley HA (2012) The choroid is thicker in angle closure than in open angle and control eyes. Invest Ophthalmol Vis Sci 53:7813–7818. https://doi.org/10.1167/iovs.12-10483
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ (2002) The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 86:238–242
Foster PJ, Aung T, Nolan WP et al (2004) Defining “occludable” angles in population surveys: drainage angle width, peripheral anterior synechiae, and glaucomatous optic neuropathy in east Asian people. Br J Ophthalmol 88:486–490
Kim YY, Jung HR (1997) Clarifying the nomenclature for primary angle-closure glaucoma. Surv Ophthalmol 42:125–136
Kumar RS, Tantisevi V, Wong MH et al (2009) Plateau iris in Asian subjects with primary angle closure glaucoma. Arch Ophthalmol Chic Ill 1960 127:1269–1272. https://doi.org/10.1001/archophthalmol.2009.241
Congdon N, Wang F, Tielsch JM (1992) Issues in the epidemiology and population-based screening of primary angle-closure glaucoma. Surv Ophthalmol 36:411–423
Day AC, Baio G, Gazzard G et al (2012) The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. Br J Ophthalmol 96:1162–1167. https://doi.org/10.1136/bjophthalmol-2011-301189
Shen L, Melles RB, Metlapally R et al (2016) The association of refractive error with glaucoma in a multiethnic population. Ophthalmology 123:92–101. https://doi.org/10.1016/j.ophtha.2015.07.002
Lowe RF (1970) Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol 54:161–169
Huang W, Wang W, Gao X et al (2013) Choroidal thickness in the subtypes of angle closure: an EDI-OCT study. Invest Ophthalmol Vis Sci 54:7849–7853. https://doi.org/10.1167/iovs.13-13158
Chen X, Hui X, Guo X (2014) Choroidal thickness of macular and peripapillary area in malignant glaucoma. Chin J Ocluar Fundus Dis 30:578–582
Quigley HA, Friedman DS, Congdon NG (2003) Possible mechanisms of primary angle-closure and malignant glaucoma. J Glaucoma 12:167–180
May CA, Fuchs AV, Scheib M, Lütjen-Drecoll E (2002) Characterization of nitrergic neurons in the porcine and human ciliary nerves. Invest Ophthalmol Vis Sci 43:581–586
May CA, Hayreh SS, Furuyoshi N et al (1997) Choroidal ganglion cell plexus and retinal vasculature in monkeys with laser-induced glaucoma. Ophthalmol J Int Ophtalmol Int J Ophthalmol Z Augenheilkd 211:161–171
May CA, Lütjen-Drecoll E (2004) Choroidal ganglion cell changes in human glaucomatous eyes. J Glaucoma 13:389–395
Funding
None. AVOPH (association for vision of the Department of Ophthalmology, Avicenne Hospital, Bobigny, France) paid for translation edition fees and will pay in case of publication fees.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Signed by patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, DT., Giocanti-Aurégan, A., Benhatchi, N. et al. Increased choroidal thickness in primary angle closure measured by swept-source optical coherence tomography in Caucasian population. Int Ophthalmol 40, 195–203 (2020). https://doi.org/10.1007/s10792-019-01171-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01171-z