Abstract
Purpose
Multiple sclerosis (MS) patients whose first demyelinating event is optic neuritis have been claimed to display a milder disease course and reduced physical disability. Our aim was to investigate the impact of the clinical features of the first clinical episode on cognitive disability and sleep dysfunction in MS.
Methods
A total of 26 (10 with optic neuritis as the first clinical event) MS patients were recruited. A comprehensive sleep study was performed, and a panel of tests were administered to examine cognitive and motor performance. Serum levels of sleep-related mediators orexin-A and melatonin were measured by enzyme-linked immunosorbent assay. Subjective sleep quality was evaluated by Pittsburgh sleep quality test, and daytime excessive sleepiness was tested by Epworth sleepiness scale.
Results
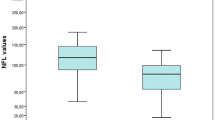
MS patients with the first clinical episode of optic neuritis and patients with at least one optic neuritis attack exhibited increased daytime sleepiness, higher sleep efficiency and NREM duration and lower total wake time. Patients with a history of optic neuritis obtained more favorable scores in neuropsychological tests measuring executive functions and complex attention as compared to those who had never experienced optic neuritis. Melatonin and orexin-A levels were lower in patients with optic neuritis onset. The higher no. of optic neuritis attacks was associated with reduced wake time and higher symbol digit modalities test scores.
Conclusions
Having a history of optic neuritis is associated with improved sleep quality and executive functions but increased daytime sleepiness. Reduction of orexin-A and melatonin levels might be one of the underlying mechanisms.
Similar content being viewed by others
References
Hughes AJ, Parmenter BA, Haselkorn JK, Lovera JF, Bourdette D, Boudreau E, Cameron MH, Turner AP (2017) Sleep and its associations with perceived and objective cognitive impairment in individuals with multiple sclerosis. J Sleep Res 26:428–435
Braley TJ, Kratz AL, Kaplish N, Chervin RD (2016) Sleep and cognitive function in multiple sclerosis. Sleep 39:1525–1533
Palma JA, Urrestarazu E, Iriarte J (2013) Sleep loss as risk factor for neurologic disorders: a review. Sleep Med 14:229–236
Heesen C, Gold SM, Raji A, Wiedemann K, Schulz KH (2002) Cognitive impairment correlates with hypothalamo-pituitary-adrenal axis dysregulation in multiple sclerosis. Psychoneuroendocrinology 27:505–517
Kantorová E, Poláček H, Bittšanský M, Baranovičová E, Hnilicová P, Čierny D, Sivák Š, Nosáľ V, Zeleňák K, Kurča E (2017) Hypothalamic damage in multiple sclerosis correlates with disease activity, disability, depression, and fatigue. Neurol Res 39:323–330
Gencer M, Akbayır E, Şen M, Arsoy E, Yılmaz V, Bulut N, Tüzün E, Türkoğlu R (2019) Serum orexin-A levels are associated with disease progression and motor impairment in multiple sclerosis. Neurol Sci. https://doi.org/10.1007/s10072-019-3708-z
Myhr KM, Riise T, Vedeler C, Nortvedt MW, Grønning R, Midgard R, Nyland HI (2001) Disability and prognosis in multiple sclerosis: demographic and clinical variables important for the ability to walk and awarding of disability pension. Mult Scler J 7:59–65
Sørensen TL, Frederiksen JL, Brønnum-Hansen H, Petersen HC (1999) Optic neuritis as onset manifestation of multiple sclerosis: a nationwide, long-term survey. Neurology 53:473–478
Düzel B, Tamam Y, Çoban A, Tüzün E (2019) Adipokines in multiple sclerosis patients with and without optic neuritis as the first clinical presentation. Immunol Invest 48:190–197
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619
Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J (2003) Restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology: a report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med 4:101–119
Sakkas GK, Giannaki CD, Karatzaferi C, Manconi M (2019) Sleep abnormalities in multiple sclerosis. Curr Treat Options Neurol 21:4
Papuć E, Stelmasiak Z, Grieb P, Paweł G, Rejdak K (2010) CSF hypocretin-1 concentrations correlate with the level of fatigue in multiple sclerosis patients. Neurosci Lett 474:9–12
Kallweit U, Bassetti CLA, Oberholzer M, Fronczek R, Béguin M, Strub M, Lammers GJ (2018) Coexisting narcolepsy (with and without cataplexy) and multiple sclerosis: six new cases and a literature review. J Neurol 265:2071–2078
Oka Y, Kanbayashi T, Mezaki T, Iseki K, Matsubayashi J, Murakami G, Matsui M, Shimizu T, Shibasaki H (2004) Low CSF hypocretin-1/orexin-A associated with hypersomnia secondary to hypothalamic lesion in a case of multiple sclerosis. J Neurol 251:885–886
Hansen S, Muenssinger J, Kronhofmann S, Lautenbacher S, Oschmann P, Keune PM (2017) Cognitive screening in multiple sclerosis: the five-point test as a substitute for the PASAT in measuring executive function. Clin Neuropsychol 31:179–192
Ferreira NV, Cunha PJ, da Costa DI, dos Santos F, Costa FO, Consolim-Colombo F, Irigoyen MC (2015) Association between functional performance and executive cognitive functions in an elderly population including patients with low ankle-brachial index. Clin Interv Aging 10:839–846
Saunamäki T, Jehkonen M (2007) A review of executive functions in obstructive sleep apnea syndrome. Acta Neurol Scand 115:1–11
Chakravarty K, Shukla G, Poornima S, Agarwal P, Gupta A, Mohammed A, Ray S, Pandey RM, Goyal V, Srivastava A, Behari M (2019) Effect of sleep quality on memory, executive function, and language performance in patients with refractory focal epilepsy and controlled epilepsy versus healthy controls—a prospective study. Epilepsy Behav 92:176–183
Kalsbeek A, Fliers E, Romijn JA, La Fleur SE, Wortel J, Bakker O, Endert E, Buijs RM (2001) The suprachiasmatic nucleus generates the diurnal changes in plasma leptin levels. Endocrinology 142:2677–2685
Zhang S, Zeitzer JM, Yoshida Y, Wisor JP, Nishino S, Edgar DM, Mignot E (2004) Lesions of the suprachiasmatic nucleus eliminate the daily rhythm of hypocretin-1 release. Sleep 27:619–627
Hardeland R (2013) Chronobiology of melatonin beyond the feedback to the suprachiasmatic nucleus-consequences to melatonin dysfunction. Int J Mol Sci 14:5817–5841
Hardeland R (2018) Melatonin and inflammation—story of a double-edged blade. J Pineal Res 65:e12525
Funding
This study was supported by Istanbul University Research Projects Fund, Project No. 30783.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Türkoğlu, R., Benbir, G., Özyurt, S. et al. Sleep disturbance and cognitive decline in multiple sclerosis patients with isolated optic neuritis as the first demyelinating event. Int Ophthalmol 40, 151–158 (2020). https://doi.org/10.1007/s10792-019-01157-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01157-x