Abstract
Purpose
The objective of this study was to investigate the efficacy and safety of phaco-endocycloplasty in an exclusive cohort of primary angle closure disease/glaucoma.
Methods
The study was interventional and non-comparative, carried out at a tertiary level eye care Institute. All adult patients (> 18 years) with angle closure disease, who had controlled or uncontrolled intra-ocular pressure (IOP) and had visually significant cataract, requiring surgery, and had undergone phaco-endocycloplasty, performed for 180°–210° simultaneously with cataract surgery, were included.
Main outcome measures
Primary outcome measure includes IOP, and secondary outcome measures include best corrected logMAR visual acuity (BCVA), anti-glaucoma medication (AGM) and complications.
Results
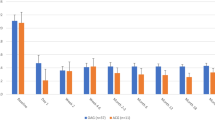
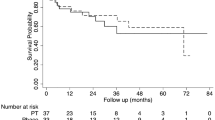
Thirty-two eyes of 28 patients were included. Median follow-up was 15 months (range 3–42 months, Q1 7.5, Q3 18, IQR 10.5). Median IOP pre-procedure (20.5 mmHg, range 11–46, Q1 16.75, Q3 31, IQR 14.25) decreased significantly post-procedure at last follow-up (IOP 16 mmHg, range 10–20, Q1 12, Q3 17.5, IQR 5.5) (p < 0.001). There was significant decrease in use of AGM (median 3 pre-procedure, range 1–5, Q1 2, Q3 3.25, IQR 1.25) at last follow-up (median 0) (p < 0.001) post-procedure. Median logMAR BCVA improved from 0.4 (Q1 0.3, Q3 0.625, IQR 0.325) to 0.05 (Q1 0, Q3 0.3, IQR 0.3) at last follow-up (p < 0.001). None of the patients had serious sight-threatening complications.
Conclusions
This study indicates that phaco-endocycloplasty can effectively control IOP, significantly reducing need for AGM, without compromising safety, in angle closure glaucoma. When combined surgery is indicated, this conjunctiva-sparing procedure may be employed in the management of coexisting cataract and glaucoma prior to bleb-forming surgery.




Similar content being viewed by others
References
George R, Ve RS, Vijaya L (2010) Glaucoma in India: estimated burden of disease. J Glaucoma 19(6):391–397
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90(3):262–267
Ang LP, Ang LP (2008) Current understanding of the treatment and outcome of acute primary angle-closure glaucoma: an Asian perspective. Ann Acad Med Singap 37(3):210–215
Wong EY, Chew PT, Chee CK, Wong JS (1997) Diode laser contact transscleral cyclophotocoagulation for refractory glaucoma in Asian patients. Am J Ophthalmol 124(6):797–804
Foster PJ (2002) The epidemiology of primary angle closure and associated glaucomatous optic neuropathy. Semin Ophthalmol 17(2):50–58
Thomas R, Parikh R, Muliyil J, Kumar RS (2003) Five-year risk of progression of primary angle closure to primary angle closure glaucoma: a population-based study. Acta Ophthalmol Scand 81(5):480–485
Nolan WP, Foster PJ, Devereux JG, Uranchimeg D, Johnson GJ, Baasanhu J (2000) YAG laser iridotomy treatment for primary angle closure in east Asian eyes. Br J Ophthalmol 84(11):1255–1259
Lim MC, Lim LS, Gazzard G, Husain R, Chan YH, Seah SK et al (2006) Lens opacity, thickness, and position in subjects with acute primary angle closure. J Glaucoma 15(3):260–263
Kim YK, Yoo BW, Kim HC, Aung T, Park KH (2014) Relative lens vault in subjects with angle closure. BMC Ophthalmol 14:93
Nongpiur ME, He M, Amerasinghe N, Friedman DS, Tay WT, Baskaran M et al (2011) Lens vault, thickness, and position in Chinese subjects with angle closure. Ophthalmology 118(3):474–479
Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS et al (2016) Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet 388(10052):1389–1397
Hayashi K, Hayashi H, Nakao F, Hayashi F (2000) Changes in anterior chamber angle width and depth after intraocular lens implantation in eyes with glaucoma. Ophthalmology 107(4):698–703
Yang CH, Hung PT (1997) Intraocular lens position and anterior chamber angle changes after cataract extraction in eyes with primary angle-closure glaucoma. J Cataract Refract Surg 23(7):1109–1113
Tran HV, Liebmann JM, Ritch R (2003) Iridociliary apposition in plateau iris syndrome persists after cataract extraction. Am J Ophthalmol 135(1):40–43
Francis BA, Pouw A, Jenkins D, Babic K, Vakili G, Tan J et al (2016) Endoscopic cycloplasty (ECPL) and lens extraction in the treatment of severe plateau iris syndrome. J Glaucoma 25(3):e128–e133
Pathak-Ray VA, Ahmed IIK (2016) Phaco-endocycloplasty: a novel technique for management of ring iridociliary cyst presenting as acute angle closure. Oman J Ophthalmol 9(1):63–65
Cairns JE (1968) Trabeculectomy: preliminary report of a new method. Am J Ophthalmol 66(4):673–679
Pathak-Ray V (2016) Advances in glaucoma surgery: paradigm shift in management. Oman J Ophthalmol 9(1):1
Siriwardena D, Kotecha A, Minassian D, Dart JK, Khaw PT (2000) Anterior chamber flare after trabeculectomy and after phacoemulsification. Br J Ophthalmol 84(9):1056–1057
Jampel HD, Quigley HA, Kerrigan-Baumrind LA, Melia BM, Friedman D, Barron Y et al (2001) Risk factors for late-onset infection following glaucoma filtration surgery. Arch Ophthalmol 119(7):1001–1008
DeBry PW, Perkins TW, Heatley G, Kaufman P, Brumback LC (2002) Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol 120(3):297–300
Landers J, Martin K, Sarkies N, Bourne R, Watson P (2012) A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology 119(4):694–702
Kahook MY, Lathrop KL, Noecker RJ (2007) One-site versus two-site endoscopic cyclophotocoagulation. J Glaucoma 16(6):527–530
Carter BC, Plager DA, Neely DE, Sprunger DT, Sondhi N, Roberts GJ (2007) Endoscopic diode laser cyclophotocoagulation in the management of aphakic and pseudophakic glaucoma in children. J AAPOS 11(1):34–40
Neely DE, Plager DA (2001) Endocyclophotocoagulation for management of difficult pediatric glaucomas. J AAPOS 5(4):221–229
Barkana Y, Morad Y, Ben-nun J (2002) Endoscopic photocoagulation of the ciliary body after repeated failure of trans-scleral diode-laser cyclophotocoagulation. Am J Ophthalmol 133(3):405–407
Wang JC, Campos-Moller X, Shah M, Sheybani A, Ahmed II (2016) Effect of endocyclophotocoagulation on refractive outcomes in angle-closure eyes after phacoemulsification and posterior chamber intraocular lens implantation. J Cataract Refract Surg 42(1):132–137
Bloom PA, Tsai JC, Sharma K, Miller MH, Rice NS, Hitchings RA et al (1997) “Cyclodiode”: Trans-scleral diode laser cyclophotocoagulation in the treatment of advanced refractory glaucoma. Ophthalmology 104(9):1508–1519 (discussion 19–20)
Alaghband P, Rodrigues IA, Goyal S (2018) Phacoemulsification with intraocular implantation of lens, endocyclophotocoagulation, and endoscopic-goniosynechialysis (PIECES): a combined technique for the management of extensive synechial primary angle closure glaucoma. J Curr Glaucoma Pract 12(1):45–49
Acknowledgement
Author thanks IIK Ahmed, MD, University of Toronto, Department of Glaucoma, Credit Valley Eye Care, 3200 Erin Mills Parkway, Mississauga, Ontario, Canada L5L 1W8.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None relevant (Novartis, Allergan).
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1: Video that demonstrates technique of phaco-endocycloplasty and ECPL in pseudoexfoliation (MOV 48,142 kb)
Rights and permissions
About this article
Cite this article
Pathak-Ray, V. Intermediate results of phaco-endocycloplasty in an exclusive cohort of angle closure glaucoma: potential for change. Int Ophthalmol 39, 2257–2265 (2019). https://doi.org/10.1007/s10792-018-01062-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-01062-9