Abstract
Objectives
As the main cause of osteoporosis, abnormal activity of osteoclasts could disrupt the balance between bone resorption and formation. Moreover, up-regulation of nuclear factor-kappa ligand (RANKL) expression by chronic inflammation-mediated inflammatory factors might contribute to the differentiation of osteoclast precursor cells. Therefore, an anti-inflammatory agent named yangonin was presented for inhibiting osteoclast and relieving inflammatory osteoporosis through down-regulating inflammatory factors.
Methods
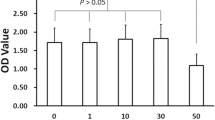
We established a model of macrophage inflammation and then verified the anti-inflammatory effect of yangonin. The inhibitory effect of yangonin on osteoclasts was detected by tartrate-resistant acid phosphatase (TRAP) staining, Western blotting and quantitative real-time PCR (qRT-PCR). Finally, micro-CT, TRAP and hematoxylin–eosin (HE) staining were used to show the effect of yangonin on inflammatory osteoporosis in vivo.
Results
Our results suggested that yangonin was able to reduce the secretion of inflammatory factors, down-regulate osteoclast-related genes such as TRAP, RANKL, cathepsin K (CTSK) and nuclear factor-activated T-cell 1 (NFATc1). Furthermore, it was demonstrated that yangonin could suppress the function of inflammatory cytokines in osteoclast differentiation and reporting, wherein NF-κB, AKT and downstream c-Fos/NFATc1 signaling pathways were involved. In an in vivo study, we implied that yangonin has a relieving effect on inflammatory osteoporosis.
Conclusion
Our research shows that yangonin down-regulates inflammatory factors and inhibits the bone-breaking effect of inflammation through NF-κB, AKT and downstream c-Fos/NFATc1 signaling pathways to achieve the purpose of treating inflammatory osteoporosis.







Similar content being viewed by others
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Abbreviations
- RANKL:
-
Receptor activator of nuclear factor-kappa ligand
- LPS:
-
Lipopolysaccharide
- CM:
-
Conditional medium
- HE:
-
Hematoxylin–eosin
- TRAP:
-
Tartrate-resistant acid phosphatase
- CTSK:
-
Cathepsin K
- NFATc1:
-
Nuclear factor-activated T-cell 1
- M-CSF:
-
Macrophage colony stimulation factor
- TRAF6:
-
Tumor necrosis factor receptor-associated factor 6
- TNF-α:
-
Tumor necrosis factor-α
- BMDM:
-
Bone marrow-derived macrophages/monocytes
- RIPA:
-
Radio-immunoprecipitation assay buffer
- PMSF:
-
Phenylmethanesulfonyl fluoride
References
Alizada A, Khyzha N, Wang L, Antounians L, Chen X, Khor M et al (2021) Conserved regulatory logic at accessible and inaccessible chromatin during the acute inflammatory response in mammals. Nat Commun 12(1):567
Asagiri M, Takayanagi H (2007) The molecular understanding of osteoclast differentiation. Bone 40(2):251–264
Black DM, Rosen CJ (2016) Clinical practice. Postmenop Osteop. N Engl J Med 374(3):254–262
Botto S, Streblow DN, De Filippis V, White L, Kreklywich CN, Smith PP et al (2011) IL-6 in human cytomegalovirus secretome promotes angiogenesis and survival of endothelial cells through the stimulation of survivin. Blood 117(1):352–361
Cao JJ, Gregoire BR, Shen C-L (2017) A high-fat diet decreases bone mass in growing mice with systemic chronic inflammation induced by low-dose. Slow-release lipopolysaccharide pellets. J Nutr 147(10):1909–1916
Dinarello CA (2019) The IL-1 family of cytokines and receptors in rheumatic diseases. Nat Rev Rheumatol 15(10):612–632
Dong R, Yang X, Wang C, Liu K, Liu Z, Ma X et al (2019) Yangonin protects against non-alcoholic fatty liver disease through farnesoid X receptor. Phytomedicine 53:134–142
Folmer F, Blasius R, Morceau F, Tabudravu J, Dicato M, Jaspars M et al (2006) Inhibition of TNFalpha-induced activation of nuclear factor kappaB by kava (Piper methysticum) derivatives. Biochem Pharmacol 71(8):1206–1218
Hirano T (2010) Interleukin 6 in autoimmune and inflammatory diseases: a personal memoir. Proc Jpn Acad Ser B Phys Biol Sci 86(7):717–730
Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Boyle WJ, Riggs BL (2000) The roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorption. J Bone Miner Res 15(1).
Ishida N, Hayashi K, Hoshijima M, Ogawa T, Koga S, Miyatake Y et al (2002) Large scale gene expression analysis of osteoclastogenesis in vitro and elucidation of NFAT2 as a key regulator. J Biol Chem 277(43):41147–41156
Kim S-H, Kim K-J, Kang HJ, Son Y-J, Choi S-W, Lee M-J (2018) The dual role of oat bran water extract in bone homeostasis through the regulation of osteoclastogenesis and osteoblast differentiation. Molecules 23(12).
Kim J-M, Lin C, Stavre Z, Greenblatt MB, Shim J-H (2020) Osteoblast-Osteoclast Communication and Bone Homeostasis. Cells 9(9).
Kong Y, Gao X, Wang C, Ning C, Liu K, Liu Z et al (2018) Protective effects of yangonin from an edible botanical Kava against lithocholic acid-induced cholestasis and hepatotoxicity. Eur J Pharmacol 824:64–71
Lee SE, Woo KM, Kim SY, Kim HM, Kwack K, Lee ZH et al (2002) The phosphatidylinositol 3-kinase, p38, and extracellular signal-regulated kinase pathways are involved in osteoclast differentiation. Bone 30(1):71–77
Li Y, Li Z, Hou H, Zhuang Y, Sun L (2018) Metal chelating, inhibitory DNA damage, and anti-inflammatory activities of phenolics from rambutan (Nephelium lappaceum) Peel and the Quantifications of Geraniin and Corilagin. Molecules 23(9):2263
Li Z, Zhu X, Xu R, Wang Y, Hu R, Xu W (2019) Deacylcynaropicrin Inhibits RANKL-Induced Osteoclastogenesis by Inhibiting NF-κB and MAPK and Promoting M2 Polarization of Macrophages. Front Pharmacol 10:599
Liu Y, Wang Z, Ma C, Wei Z, Chen K, Wang C et al (2020) Dracorhodin perchlorate inhibits osteoclastogenesis through repressing RANKL-stimulated NFATc1 activity. J Cell Mol Med 24(6):3303–3313
Medzhitov R (2008) Origin and physiological roles of inflammation. Nature 454(7203):428–435
Michalski MN, McCauley LK (2017) Macrophages and skeletal health. Pharmacol Ther 174:43–54
Minoshima M, Kikuta J, Omori Y, Seno S, Suehara R, Maeda H et al (2019) Multicolor imaging with fluorescent probes revealed the dynamics and function of osteoclast proton pumps. ACS Cent Sci 5(6):1059–1066
Napimoga MH, Dantas Formiga WD, Abdalla HB, Trindade-da-Silva CA, Venturin CM, Martinez EF et al (2020) Secreted osteoclastogenic factor of activated T cells (SOFAT) is associated with rheumatoid arthritis and joint pain: initial evidences of a new pathway. Front Immunol 11:1442
Nickoloff BJ, Ben-Neriah Y, Pikarsky E (2005) Inflammation and cancer: is the link as simple as we think? J Invest Dermatol. https://doi.org/10.1111/j.0022-202X.2005.23724.x
Park K-R, Kim E-C, Hong JT, Yun H-M (2018) Dysregulation of 5-hydroxytryptamine 6 receptor accelerates maturation of bone-resorbing osteoclasts and induces bone loss. Theranostics 8(11):3087–3098
Qu X, Tang Y, Hua S (2018) Immunological approaches towards cancer and inflammation: a cross talk. Front Immunol 9:563
Rivers-Auty J, Daniels MJD, Colliver I, Robertson DL, Brough D (2018) Redefining the ancestral origins of the interleukin-1 superfamily. Nat Commun 9(1):1156
Saylor PJ, Lee RJ, Smith MR (2011) Emerging therapies to prevent skeletal morbidity in men with prostate cancer. J Clin Oncol 29(27):3705–3714
Sinder BP, Pettit AR, McCauley LK (2015) Macrophages: their emerging roles in bone. J Bone Miner Res 30(12):2140–2149
Smith BJ, Lerner MR, Bu SY, Lucas EA, Hanas JS, Lightfoot SA et al (2006) Systemic bone loss and induction of coronary vessel disease in a rat model of chronic inflammation. Bone 38(3):378–386
Sun X, Wang Y, Zhang M, Wang Q (2019) Intraarticular injection of dexamethasone promotes bone erosion in collagen-induced arthritis in mice through up-regulation of RANKL expression. Inflammopharmacology 27(3):503–509
Talaat RM, Sidek A, Mosalem A, Kholief A (2015) Effect of bisphosphonates treatment on cytokine imbalance between TH17 and Treg in osteoporosis. Inflammopharmacology 23(2–3):119–125
Tanaka T, Narazaki M, Kishimoto T (2014) IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol 6(10):a016295
Wang J, Wu X, Duan Y (2018) Magnesium lithospermate B protects against lipopolysaccharide-induced bone loss by inhibiting RANKL/RANK pathway. Front Pharmacol 9:64
Wang X, Fu T, Wang J, Wang C, Liu K, Wu J et al (2019) Hepatoprotection of yangonin against hepatic fibrosis in mice via farnesoid X receptor activation. Int Immunopharmacol 75:105833
Wei W, Wang X, Yang M, Smith LC, Dechow PC, Sonoda J et al (2010) PGC1beta mediates PPARgamma activation of osteoclastogenesis and rosiglitazone-induced bone loss. Cell Metab 11(6):503–516
Won H, Nandakumar V, Yates P, Sanchez S, Jones L, Huang XF et al (2014) Epigenetic control of dendritic cell development and fate determination of common myeloid progenitor by Mysm1. Blood 124(17):2647–2656
Xiong J, Cawley K, Piemontese M, Fujiwara Y, Zhao H, Goellner JJ et al (2018) Soluble RANKL contributes to osteoclast formation in adult mice but not ovariectomy-induced bone loss. Nat Commun 9(1):2909
Yan H, Shao D, Lao Y-H, Li M, Hu H, Leong KW (2019) Engineering cell membrane-based nanotherapeutics to target inflammation. Adv Sci (Weinh) 6(15):1900605
Yao F, Xue Q, Li K, Cao X, Sun L, Liu Y (2019) Phenolic compounds and ginsenosides in ginseng shoots and their antioxidant and anti-inflammatory capacities in LPS-induced RAW264.7 mouse macrophages. Int J Mol Sci 20(12):2951
Zeng Q, Lu W, Deng Z, Wu J, Guo R, Xu X (2020) Tablysin-15 inhibits osteoclastogenesis and LPS-induced bone loss via attenuating the integrin αβ pathway. Chem Biol Interact 327:109179
Zhou P, Gross S, Liu J-H, Yu B-Y, Feng L-L, Nolta J et al (2010) Flavokawain B, the hepatotoxic constituent from kava root, induces GSH-sensitive oxidative stress through modulation of IKK/NF-kappaB and MAPK signaling pathways. FASEB J 24(12):4722–4732
Zhu N, Hou J (2021) Molecular mechanism of the anti-inflammatory effects of Sophorae Flavescentis Aiton identified by network pharmacology. Sci Rep 11(1):1005
Funding
This study was supported by the Natural Science Foundation of Zhejiang Province (LY20H060006), Experimental Animal Science Project of Zhejiang Province (LGD19H310001). The authors thank Professor Li Wang of Research Center for Integrated Medicine Affiliated Traditional Medicine Hospital of Southwest Medical University for his guidance.
Author information
Authors and Affiliations
Contributions
HC and FL conceived the study. FL and HH contributed to the acquisition and interpretation of data. FL and XW did the data cleaning, statistical analysis and model building with assistance from ZJ, XS, XJ, LC and JS. FL and HH drafted the manuscript. All authors contributed to the critical revision of the manuscript for important intellectual content. All authors critically reviewed the manuscript for important intellectual content and gave final approval for the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
We declare that no conflict of interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lu, F., Wu, X., Hu, H. et al. Yangonin treats inflammatory osteoporosis by inhibiting the secretion of inflammatory factors and RANKL expression. Inflammopharmacol 30, 1445–1458 (2022). https://doi.org/10.1007/s10787-022-00985-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-022-00985-1