Abstract
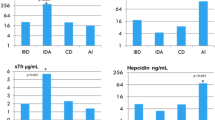
Ulcerative colitis (UC) is often associated with anemia. Hepcidin, the central regulator of iron homeostasis, is known to be induced by inflammation and suppressed by anemia. It is not clear how hepcidin is affected in those with UC, when both inflammation and anemia may co-exist.Such knowledge may hold implications for treatment. Hematological and iron-related parameters, C-reactive protein (CRP), growth differentiation factor 15 (GDF-15) and erythroferrone (ERFE) (erythroid regulators of hepcidin) levels were estimated in blood from those with UC and in control subjects. Values for hematological and iron-related parameters showed evidence of iron-deficiency and resultant anemia, in patients with UC. The presence of UC was significantly associated with inflammation. Serum levels of ERFE, but not of GDF-15, were significantly higher in patients with UC than in control patients, while hepcidin levels were significantly lower. Serum hepcidin concentrations in patients with UC correlated positively with serum iron, ferritin and GDF-15, and negatively with serum ERFE. The iron status and serum hepcidin levels in UC patients with co-existent anemia were significantly lower and serum ERFE values significantly higher than in those with UC without anemia. The effect of anemia on hepcidin predominated over that of inflammation in patients with UC, resulting in suppressed hepcidin levels. This effect is possibly mediated through erythroferrone. We suggest that a serum hepcidin-guided approach may be useful to guide use of oral iron supplements to treat co-existent iron-deficiency anemia in patients with UC and other chronic inflammatory diseases.


Similar content being viewed by others
Data Availability
The data in this article will be shared on reasonable request to the corresponding author.
Change history
11 August 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10753-023-01887-2
References
Cucino, C., and A. Sonnenberg. 2001. Cause of death in patients with inflammatory bowel disease. Inflammatory Bowel Diseases 7:250–255.
Kulnigg, S., and C. Gasche. 2006. Systematic review: Managing anaemia in Crohn’s disease. Alimentary Pharmacology & Therapeutics 24:1507–1523. https://doi.org/10.1111/j.1365-2036.2006.03146.x.
Gasche, C., M.C.E. Lomer, I. Cavill, and G. Weiss. 2004. Iron, anaemia, and inflammatory bowel diseases. Gut 53: 1190–1197. https://doi.org/10.1136/gut.2003.035758.
Sonia, F., and R. S. Blummberg. 2011. Harrisons Principles of Internal Medicine. 18th ed. Vol. 2. 2 vols. McGraw Hill.
Robert, M., J. Molly. and J. Varghese. 2012. Harper’s illustrated Biochemistry. 29th edition. 1043–9811. Section-VI.,Chapter-50. pp/ 629–650.
Nemeth, E., M. S. Tuttle, J. Powelson, M.B. Vaughn, A. Donovan, D. McVey Ward, T. Ganz and J. Kaplan. 2004. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science (New York, N.Y.) 306: 2090–2093. https://doi.org/10.1126/science.1104742.
Gaël, N., C. Chauvet, L. Viatte, J.L. Danan, X. Bigard, I. Devaux, C. Beaumont, A. Kahn, and S. Vaulont. 2002. The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. The Journal of Clinical Investigation 110: 1037–1044. https://doi.org/10.1172/JCI15686.
Kautz, L. G. Jung, E.V. Valore, S. Rivella, E. Nemeth, and T. Ganz. 2014. Identification of erythroferrone as an erythroid regulator of iron metabolism. Nature Genetics 46:678–684. https://doi.org/10.1038/ng.2996.
Tanno, T., N.V. Bhanu, P.A. Oneal, S.H. Goh, Y. Pamela Staker, T. Lee, J.W. Moroney, et al. 2007. High levels of GDF15 in thalassemia suppress expression of the iron regulatory protein hepcidin. Nature Medicine 13:1096–1101. https://doi.org/10.1038/nm1629.
Tanno, T., P. Porayette, O. Sripichai, S.J. Noh, C. Byrnes, Y. Ajoy Bhupatiraju, T. Lee, et al. 2009. Identification of TWSG1 as a second novel erythroid regulator of hepcidin expression in murine and human cells. Blood 114:181–186. https://doi.org/10.1182/blood-2008-12-195503.
Basseri, R.J. E. Nemeth, M.E. Vassilaki, B. Basseri, P. Enayati, O. Shaye, L.A. Bourikas, T. Ganz, and K.A. Papadakis. 2013. Hepcidin is a key mediator of anemia of inflammation in Crohn’s disease. Journal of Crohn’s & Colitis 7:e286-291. https://doi.org/10.1016/j.crohns.2012.10.013.
Oustamanolakis, P., I.E. Koutroubakis, I. Messaritakis, N. Malliaraki, A. Sfiridaki, and Elias A. Kouroumalis. 2011. Serum hepcidin and prohepcidin concentrations in inflammatory bowel disease. European Journal of Gastroenterology & Hepatology 23:262–268. https://doi.org/10.1097/MEG.0b013e328343b885.
Semrin, G., D.S. Fishman, A. Bousvaros, A. Zholudev, A.C. Saunders, C. E. Correia, E. Nemeth, R.J. Grand, and D. A. Weinstein. 2006. Impaired intestinal iron absorption in Crohn’s disease correlates with disease activity and markers of inflammation. Inflammatory Bowel Diseases 12:1101–1106. https://doi.org/10.1097/01.mib.0000235097.86360.04.
Arnold, J., A. Sangwaiya, B. Bhatkal, F. Geoghegan, and M. Busbridge. 2009. Hepcidin and inflammatory bowel disease: Dual role in host defence and iron homoeostasis. European Journal of Gastroenterology & Hepatology 21:425–429. https://doi.org/10.1097/MEG.0b013e32830e2885.
Sukumaran, A., J. James, H. P. Janardhan, A. Amaladas, L. M. Suresh, D.D.V Jeyeseelan, B.S. Ramakrishna, and M. Jacob. 2014. Expression of iron-related proteins in the duodenum is up-regulated in patients with chronic inflammatory disorders. The British Journal of Nutrition 111:1059–1068. https://doi.org/10.1017/S0007114513003334.
Magro, F., P. Gionchetti, R. Eliakim, S. Ardizzone, A. Armuzzi, M. Barreiro-de Acosta, J. Burisch, et al. 2017. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. Journal of Crohn’s and Colitis 11. Oxford Academic: 649–670. https://doi.org/10.1093/ecco-jcc/jjx008.
Higgins, T, J.H. Eckfeldt, J.C. Barton, and B.T. Doumas. 2012. Chapter 32 - Hemoglobin, Iron and Bilirubin. In Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 5th ed. Elsevier Saunders.
Dignass, A.U., C. Gasche, D. Bettenworth, G. Birgegård, S. Danese, J.P. Gisbert, F. Gomollon, et al. 2015. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. Journal of Crohn’s & Colitis 9:211–222. https://doi.org/10.1093/ecco-jcc/jju009.
Jimenez, K.M., and C. Gasche. 2019. Management of Iron Deficiency Anaemia in Inflammatory Bowel Disease. Acta Haematologica 142:30–36. https://doi.org/10.1159/000496728.
Schroeder, K.W., W.J. Tremaine, and D.M. Ilstrup. 1987. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A Randomized Study. https://doi.org/10.1056/NEJM198712243172603.
Mohammed Vashist, N., M. Samaan, M.H. Mosli, C.E. Parker, J.K. MacDonald, S.A. Nelson, G.Y. Zou, B.G. Feagan, R. Khanna, and V. Jairath. 2018. Endoscopic scoring indices for evaluation of disease activity in ulcerative colitis. Cochrane Database of Systematic Reviews: John Wiley & Sons, Ltd. https://doi.org/10.1002/14651858.CD011450.pub2.
Silverberg, M.S., J. Satsangi, T. Ahmad, I.D R. Arnott, C.N. Bernstein, S.R. Brant, R. Caprilli, et al. 2005. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Canadian Journal of Gastroenterology = Journal Canadien De Gastroenterologie 19 Suppl A:5A-36A. https://doi.org/10.1155/2005/269076.
Choi, C.H., W.M., You S. Kim, E.S. Kim, B.-I. Lee, Y. Jung, Y.S. Yoon, et al. 2017. Second Korean guidelines for the management of ulcerative colitis. Intestinal Research 15:7–37. https://doi.org/10.5217/ir.2017.15.1.7.
Truelove, S.C., and L.J. Witts. 1955. Cortisone in ulcerative colitis; final report on a therapeutic trial. British Medical Journal 2:1041–1048. https://doi.org/10.1136/bmj.2.4947.1041.
Nemeth, Elizabeta, S. Rivera, V. Gabayan, C. Keller, S. Taudorf, B.K. Pedersen, and T. Ganz. 2004. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. The Journal of Clinical Investigation 113:1271–1276. https://doi.org/10.1172/JCI20945.
Theurl, I., E. Aigner, M. Theurl, M. Nairz, M. Seifert, A. Schroll, T. Sonnweber, et al. 2009. Regulation of iron homeostasis in anemia of chronic disease and iron deficiency anemia: Diagnostic and therapeutic implications. Blood. 113:5277–5286. https://doi.org/10.1182/blood-2008-12-195651.
Finch, C. 1994. Regulators of Iron Balance in Humans Vol 84, NO 6:6.
Pak, Mihwa, M.A. Lopez, V. Gabayan, T. Ganz, and S. Rivera. 2006. Suppression of hepcidin during anemia requires erythropoietic activity. Blood 108:3730–3735. https://doi.org/10.1182/blood-2006-06-028787.
Arezes, J., N. Foy, K. McHugh, A. Sawant, D. Quinkert, V. Terraube, A. Brinth, et al. 2018. Erythroferrone inhibits the induction of hepcidin by BMP6. Blood 132:1473–1477. https://doi.org/10.1182/blood-2018-06-857995.
Canali, S., K.B. Zumbrennen-Bullough, A.B. Core, C-Y. Wang, M. Nairz, R. Bouley, F.K. Swirski, and J.L. Babitt. 2017. Endothelial cells produce bone morphogenetic protein 6 required for iron homeostasis in mice. Blood 129:405–414. https://doi.org/10.1182/blood-2016-06-721571.
Hentze, M., W., M.U. Muckenthaler, B. Galy, and C. Camaschella. 2010. Two to tango: Regulation of Mammalian iron metabolism. Cell 142:24–38. https://doi.org/10.1016/j.cell.2010.06.028.
Koch, P.S., V. Olsavszky, F. Ulbrich, C. Sticht, A. Demory, T. Leibing, T. Henzler, et al. 2017. Angiocrine Bmp2 signaling in murine liver controls normal iron homeostasis. Blood 129:415–419. https://doi.org/10.1182/blood-2016-07-729822.
Zhao, N., C.P. Nizzi, S.A. Anderson, J.W., A. Ueno, H. Tsukamoto, R.S. Eisenstein, C.A. Enns, and A.-S. Zhang. 2015. Low intracellular iron increases the stability of matriptase-2. The Journal of Biological Chemistry 290:4432–4446. https://doi.org/10.1074/jbc.M114.611913.
Schmidt, P. J., P.T. Toran, A.M. Giannetti, P.J. Bjorkman, and N.C. Andrews. 2008. The transferrin receptor modulates Hfe-dependent regulation of hepcidin expression. Cell Metabolism 7:205–214. https://doi.org/10.1016/j.cmet.2007.11.016.
Jiang, F., W.-J. Yu, X.-H. Wang, Y.-T.g Tang, L. Guo, and X.-Y. Jiao. 2014. Regulation of hepcidin through GDF-15 in cancer-related anemia. Clinica Chimica Acta; International Journal of Clinical Chemistry 428:14–19. https://doi.org/10.1016/j.cca.2013.10.015.
Mirciov, C., S. G., Sarah J. Wilkins, Linda A. Dunn, Gregory J. Anderson, and D.M. Frazer. 2017. Characterization of Putative Erythroid Regulators of Hepcidin in Mouse Models of Anemia. PloS One 12:e0171054. https://doi.org/10.1371/journal.pone.0171054.
Dignass, A., K. Farrag, and J. Stein. 2018. Limitations of Serum Ferritin in Diagnosing Iron Deficiency in Inflammatory Conditions. International Journal of Chronic Diseases 2018:9394060. https://doi.org/10.1155/2018/9394060.
Gasche, C, A.B., Ragnar Befrits, C. Beglinger, A. Dignass, K.E. Fernando Gomollon, et al. 2007. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflammatory Bowel Diseases 13:1545–1553. https://doi.org/10.1002/ibd.20285.
Rizvi, S., and R.E. Schoen. 2011. Supplementation with oral vs. intravenous iron for anemia with IBD or gastrointestinal bleeding: Is oral iron getting a bad rap? The American Journal of Gastroenterology 106:1872–1879. https://doi.org/10.1038/ajg.2011.232.
Aksan, A., M. Wohlrath, T.H. Iqbal, A. Dignass, and J. Stein. 2020. Inflammation, but Not the Underlying Disease or Its Location, Predicts Oral Iron Absorption Capacity in Patients With Inflammatory Bowel Disease. Journal of Crohn’s & Colitis 14:316–322. https://doi.org/10.1093/ecco-jcc/jjz149.
Rampton, D.S., J.R. Goodhand, N.M. Joshi, A-B. Karim, Y. Koodun, F.M. Barakat, L. Macken, et al. 2017. Oral Iron Treatment Response and Predictors in Anaemic Adolescents and Adults with IBD: A Prospective Controlled Open-Label Trial. Journal of Crohn’s & Colitis 11:706–715. https://doi.org/10.1093/ecco-jcc/jjw208.
Shah, Y., D. Patel, and N. Khan. 2021. Iron deficiency anemia in IBD: An overlooked comorbidity. Expert Review of Gastroenterology & Hepatology 15:771–781. https://doi.org/10.1080/17474124.2021.1900730.
Cercamondi, C.I., N.U. Stoffel, D. Moretti, T. Zoller, D.W. Swinkels, C. Zeder, F. Mhimibra, J. Hella, L. Fenner, and M.B. Zimmermann. 2021. Iron homeostasis during anemia of inflammation: A prospective study of patients with tuberculosis. Blood 138:1293–1303. https://doi.org/10.1182/blood.2020010562.
Minor, E.A. J.T. Kupec, A.J. Nickerson, K. Narayanan, and V.M. Rajendran. 2020. Increased DMT1 and FPN1 expression with enhanced iron absorption in ulcerative colitis human colon. American Journal of Physiology-Cell Physiology 318. American Physiological Society: C263–C271. https://doi.org/10.1152/ajpcell.00128.2019.
Funding
This work was supported by Fluid Research grants from Christian Medical College, Vellore, India (IRB minute numbers 7372 dated 08.12.2010, 8150 dated 09.01.13 and 8823 dated 07.04.2014). Christian Medical College, Vellore, is affiliated to The Tamil Nadu Dr MGR Medical University, Chennai, Tamil Nadu, India.
Author information
Authors and Affiliations
Contributions
Jagadish Ramasamy: recruited participants, collected data, analyzed, and interpreted results, and wrote the manuscript; Chinmai Jagadish and Abitha Sukumaran: recruited participants and collected and analyzed data; AJ Joseph and Ebby George Simon: provided logistical support to recruit participants and collect data; Joe Varghese and Thenmozhi Mani: analyzed and interpreted data; Molly Jacob: conceptualized and designed the study, analyzed data, interpreted results, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study was performed in line with the principles of the Declaration of Helsinki. The study was approved by the Institutional Review Board of Christian Medical College (CMC), Vellore, India (IRB minute numbers 7372 dated 08.12.2010, 8150 dated 09.01.13 and 8823 dated 07.04.2014). Informed consent was obtained from all recruited subjects to participate in the study.
Human and Animal Ethics
This study involves only human participants, and it was performed in line with the principles of the Declaration of Helsinki. The study was approved by the Institutional Review Board of Christian Medical College (CMC), Vellore, India (IRB minute numbers 7372 dated 08.12.2010, 8150 dated 09.01.13 and 8823 dated 07.04.2014). Informed consent was obtained from all recruited subjects to participate in the study.
Consent for Publication
Informed consent was obtained from all recruited subjects for publishing the results of the study.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The article had mistakes with regards to use of the symbols ≤ and ≥.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramasamy, J., Jagadish, C., Sukumaran, A. et al. Low Serum Hepcidin Levels in Patients with Ulcerative Colitis – Implications for Treatment of Co-existent Iron-Deficiency Anemia. Inflammation 46, 2209–2222 (2023). https://doi.org/10.1007/s10753-023-01872-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-023-01872-9