Abstract
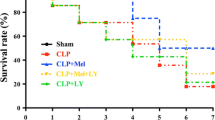
Melatonin improves survival and functional impairment including hemolysis, thrombocytopenia, and hypotension when administered in a prophylactic manner or early after initiation of sepsis or endotoxemia. In the present study, melatonin was given not before first symptoms of systemic inflammation became manifest. Lipopolysaccharide was infused at a rate of 0.5 mg/kg × h to induce systemic inflammation in male Wistar rats. Melatonin (single dose 3 mg/kg × 15 min) was intravenously administered 180 and 270 min after starting of the lipopolysaccharide infusion. Systemic and vital parameters (e.g., systemic blood pressure and breathing rate) as well as blood and plasma parameters (acid-base parameters; electrolytes; parameters of tissue injury such as glucose concentration, lactate concentration, hemolysis, and aminotransferase activities; parameters of thromboelastometry; and platelet count) were determined in regular intervals. Infusion of lipopolysaccharide led to characteristic symptoms of severe systemic inflammation including hypotension, metabolic acidosis and hypoglycemia, electrolyte and hemostatic disturbances, thrombocytopenia, and hemolysis. Melatonin neither decreased mortality nor reduced lipopolysaccharide-dependent changes to vital, blood, and plasma parameters. Even though melatonin may have a beneficial effect in early stages of systemic inflammation, it can hardly be an option in therapy of manifest sepsis or endotoxemia in an intensive care unit.



Similar content being viewed by others
References
Hardeland, R., and B. Poeggeler. 2003. Non-vertebrate melatonin. Journal of Pineal Research 34: 233–241.
Tan, D.X., L.C. Manchester, R. Hardeland, S. Lopez-Burillo, J.C. Mayo, R.M. Sainz, and R.J. Reiter. 2003. Melatonin: A hormone, a tissue factor, an autocoid, a paracoid, and an antioxidant vitamin. Journal of Pineal Research 34: 75–78.
Challet, E. 2007. Minireview: Entrainment of the suprachiasmatic clockwork in diurnal and nocturnal mammals. Endocrinology 148: 5648–5655.
Srinivasan, V., S.R. Pandi-Perumal, D.W. Spence, H. Kato, and D.P. Cardinali. 2010. Melatonin in septic shock: Some recent concepts. Journal of Critical Care 25 (4): 656.e651–656.e656.
Carrillo-Vico, A., P.J. Lardone, L. Naji, J.M. Fernandez-Santos, I. Martin-Lacave, J.M. Guerrero, and J.R. Calvo. 2005. Beneficial pleiotropic actions of melatonin in an experimental model of septic shock in mice: Regulation of pro-/anti-inflammatory cytokine network, protection against oxidative damage and anti-apoptotic effects. Journal of Pineal Research 39: 400–408.
Arendt, J. 1999. Jet-lag and shift work: (2) Therapeutic use of melatinon. Journal of Royal Society of Medicine 92: 402–405.
Effenberger-Neidnicht, K., L. Brencher, M. Broecker-Preuss, T. Hamburger, F. Petrat, and H. De Groot. 2014. Immune stimulation by exogenous melatonin during experimental endotoxemia. Inflammation 37: 738–744.
Wu, C.-C., C.-W. Chiao, G. Hsiao, A. Chen, and M.-H. Yen. 2001. Melatonin prevents endotoxin-induced circulatory failure in rats. Journal of Pineal Research 30: 147–156.
Ersoy, O.F., N. Ozkan, Z. Ozsoy, H.A. Kayaoglu, E. Yenidogan, A. Celik, A.F. Ozugurlu, E. Arabaci Cakir, and N. Lortlar. 2016. Effects of melatonin on cytokine release and healing of colonic anastomoses in an experimental sepsis model. Turkish Journal of Trauma & Emergency Surgery 22: 315–321.
Gitto, E., M. Karbownik, R.J. Reiter, D.X. Tan, S. Cuzzocrea, P. Chiurazzi, S. Cordaro, G. Corona, G. Trimachi, and I. Barberi. 2001. Effects of melatonin treatment in septic newborns. Pediatric Research 50: 756–760.
El Frargy, M., H.M. El-Sharkawy, and G.F. Attia. 2015. Use of melatonin as an adjuvant therapy in neonatal sepsis. Journal of Neonatal-Perinatal Medicine 8: 227–232.
El Frargy, M.S., H.M. El-Sharkawy, and G.F. Attia. 2015. Adjuvant therapy in the treatment of sepsis in premature neonates. Global Journal of Medicine Researches and Studies 2: 1–6.
Effenberger-Neidnicht, K., M. Al Nator, L. Brencher, M. Oude Lansink, and H. De Groot. 2013. Prevention of endotoxin-induced hypotension in rats by the circadian hormone melatonin. Infection 41: S11–S12.
Wu, J.-Y., M.-Y. Tsou, T.-H. Chen, S.-J. Chen, C.-M. Tsao, and C.-C. Wu. 2008. Therapeutic effects of melatonin on peritonitis-induced septic shock with multiple organ dysfunction syndrome in rats. Journal of Pineal Research 45: 106–116.
Crespo, E., M. Macias, G. Escames, M. Martin, F. Vives, J.M. Guerrero, and D. Acuna-Castroviejo. 1999. Melatonin inhibits expression of the inducible NO synthase II in liver and lung and prevents endotoxemia in lipopolysaccharide-induced multiple organ dysfunction syndrome in rats. The FASEB Journal 13: 1537–1546.
An, R., L. Zhao, C. Xi, H. Li, G. Shen, H. Liu, S. Zhang, and L. Sun. 2016. Melatonin attenuates sepsis-induced cardiac dysfunction via a PI3K/Akt-dependent mechanism. Basic Research in Cardiology 111: 8.
Oude Lansink, M., K. Görlinger, M. Hartmann, H. de Groot, and K. Effenberger-Neidnicht. 2016. Melatonin does not affect disseminated intravascular coagulation but diminishes decreases in platelet count during subacute endotoxaemia in rats. Thrombosis Research 139: 38–43.
Zhang, H., D. Liu, X.-B. Wang, X. Chen, Y. Long, W. Chai, X. Zhou, et al. 2013. Melatonin improved rat cardiac mitochondria and survival rate in septic heart injury. Journal of Pineal Research 55: 1–6.
Fink, T., M. Glas, A. Wolf, A. Kleber, E. Reus, M. Wolff, D. Kiefer, et al. 2014. Melatonin receptors mediate improvements of survival in a model of polymicrobial sepsis. Critical Care Medicine 42: e22–e31.
Effenberger-Neidnicht, K., J. Jägers, R. Verhaegh, and H. De Groot. 2014. Glycine reduces small intestinal tissue injury in a rat model of endotoxemia. The Journal of Surgical Research 192: 592–598.
Oude Lansink, M., V. Patyk, H. de Groot, and K. Effenberger-Neidnicht. 2017. Melatonin reduces changes to small intestinal microvasculature during systemic inflammation. The Journal of Surgical Research 211: 114–125.
Hamburger, T., M. Broecker-Preuss, M. Hartmann, F.U. Schade, H. de Groot, and F. Petrat. 2013. Effects of glycine, pyruvate, resveratrol, and nitrite on tissue injury and cytokine response in endotoxemic rats. The Journal of Surgical Research 183: e7–e21.
Galley, H.F., D.A. Lowes, L. Allen, G. Cameron, L.S. Aucott, and N.R. Webster. 2014. Melatonin as a potential therapy for sepsis: a phase I dose escalation study and an ex vivo whole blood model under conditions of sepsis. Journal of Pineal Research 56: 427–438.
Li, C.X., D.D. Liang, G.H. Xie, B.L. Cheng, Q.X. Chen, S.J. Wu, J.L. Wang, W. Cho, and X.M. Fang. 2013. Altered melatonin secretion and circadian gene expression with increased proinflammatory cytokine expression in early-stage sepsis patients. Molecular Medicine Reports 7: 1117–1122.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brencher, L., Oude Lansink, M. & Effenberger-Neidnicht, K. Administration of Exogenous Melatonin After the Onset of Systemic Inflammation Is Hardly Beneficial. Inflammation 40, 1672–1677 (2017). https://doi.org/10.1007/s10753-017-0608-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-017-0608-3