Abstract
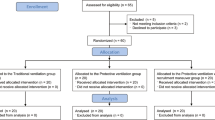
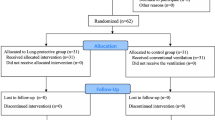
Laparoscopic surgery is performed by carbon dioxide (CO2) insufflation, but this may induce stress responses. The aim of this study is to compare the level of inflammatory mediators in patients receiving low tidal volume (VT) versus traditional VT during gynecological laparoscopic surgery. Forty American Society of Anesthesiologists (ASA) physical status 1 and 2 subjects older than 18 years old undergoing laparoscopic gynecological surgery were included. Systemic inflammatory response was assessed with serum IL-6, TNF-alpha, IL-8, and IL-1β in patients receiving intraoperative low VT and traditional VT during laparoscopic surgery [within the first 5 min after endotracheal intubation (T1), 60 min after the initiation of mechanical ventilation (T2), and in the postanesthesia care unit 30 min after tracheal extubation (T3)]. Additionally, inflammatory response was assessed with bronchoalveolar lavage (BAL) at T1 and T3 periods. An increase in the serum levels of IL-6, TNF-alpha, IL-8, and IL-1β was observed in both groups during the time periods of T1, T2, and T3. No significant differences were found in the serum and BAL levels of inflammatory mediators during time periods between groups. The results of the present study suggested that the lung-protective ventilation and traditional strategies are not different in terms of lung injury and inflammatory response during conventional laparoscopic gynecological surgery.


Similar content being viewed by others
References
Aran, T., M.A. Unsal, S. Güven, C. Kart, E.C. Cetin, and A. Alver. 2012. Carbon dioxide pneumoperitoneum induces systemic oxidative stress: a clinical study. Eur J Obstet Gynecol Reprod Biol 161: 80–83.
Han, C., Z. Ding, J. Fan, J. Sun, and Y. Qian. 2012. Comparison of the stress response in patients undergoing gynecological laparoscopic surgery using carbon dioxide pneumoperitoneum or abdominal wall-lifting methods. J Laparoendosc Adv Surg Tech A 22: 330–335.
Brower, R.G., P.N. Lanken, N. MacIntyre, M.A. Matthay, A. Morris, M. Ancukiewicz, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network, et al. 2004. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 351: 327–336.
Wolthuis, E.K., G. Choi, M.C. Dessing, P. Bresser, R. Lutter, M. Dzoljic, et al. 2008. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology 108: 46–54.
Wrigge, H., U. Uhlig, J. Zinserling, E. Behrends-Callsen, G. Ottersbach, M. Fischer, et al. 2004. The effects of different ventilatory settings on pulmonary and systemic inflammatory responses during major surgery. Anesth Analg 98: 775–81.
Koner, O., S. Celebi, H. Balci, G. Cetin, K. Karaoglu, and N. Cakar. 2004. Effects of protective and conventional mechanical ventilation on pulmonary function and systemic cytokine release after cardiopulmonary bypass. Intensive Care Med 30: 620–626.
Memtsoudis, S.G., A.M. Bombardieri, Y. Ma, and F.P. Girardi. 2012. The effect of low versus high tidal volume ventilation on inflammatory markers in healthy individuals undergoing posterior spine fusion in the prone position: a randomized controlled trial. J Clin Anesth 24: 263–269.
Weingarten, T.N., F.X. Whalen, D.O. Warner, O. Gajic, G.J. Schears, M.R. Snyder, et al. 2010. Comparison of two ventilatory strategies in elderly patients undergoing major abdominal surgery. Br J Anaesth 104: 16–22.
Faul, F., E. Erdfelder, A. Buchner, and A.G. Lang. 2009. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41: 1149–1160.
Sahin, D.A., B. Haliloglu, F.K. Sahin, G. Akbulut, H. Fidan, G. Koken, et al. 2007. Stepwise rising CO2 insufflation as an ischemic preconditioning method. J Laparoendosc Adv Surg Tech A 17: 723–729.
Duggan, M., and P. Kavanagh. 2007. Atelectasis in the perioperative patient. Curr Opin Anaesthesiol 20: 37–42.
Pelosi, P., and P.R. Rocco. 2007. Airway closure: the silent killer of peripheral airways. Crit Care 11: 114–115.
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network. N Engl J Med 2000;342:1301–8.
Hickling, K.G., and S.J. Henderson. 1990. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med 16: 372–377.
Amato, M.B., C.S. Barbas, D.M. Medeiros, R.B. Magaldi, G.P. Schettino, G. Lorenzi-Filho, et al. 1998. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338: 347–354.
Ranieri, V.M., P.M. Suter, C. Tortorella, R. De Tullio, J.M. Dayer, A. Brienza, et al. 1999. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 282: 54–61.
Stüber, F., H. Wrigge, S. Schroeder, S. Wetegrove, J. Zinserling, A. Hoeft, et al. 2002. Kinetic and reversibility of mechanical ventilation-associated pulmonary and systemic inflammatory response in patients with acute lung injury. Intensive Care Med 28: 834–841.
Kilpatrick, B., and P. Slinger. 2010. Lung protective strategies in anaesthesia. Br J Anaesth 105: 108–16.
Hong, C.M., D.Z. Xu, Q. Lu, Y. Cheng, V. Pisarenko, D. Doucet, et al. 2010. Low tidal volume and high positive end-expiratory pressure mechanical ventilation results in increased inflammation and ventilator-associated lung injury in normal lungs. Anesth Analg 110: 1652–1660.
Schultz, M.J., J.J. Haitsma, A.S. Slutsky, and O. Gajic. 2007. What tidal volumes should be used in patients without acute lung injury? Anesthesiology 106: 1226–1231.
Galley, H.F., M.A. DiMatteo, and N.R. Webster. 2000. Immunomodulation by anaesthetic, sedative and analgesic agents: does it matter? Intensive Care Med 26: 267–274.
Wolthuis, E.K., G. Choi, M.C. Dessing, P. Bresser, R. Lutter, M. Dzoljic, et al. 2008. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology 108: 46–54.
Dunn, I., and J. Pugin. 1999. Mechanical ventilation of various human lung cells in vitro: identification of the macrophage as the main producer of inflammatory mediators. Chest 116: 95–97.
Dos Santos, C.C., B. Han, C.F. Andrade, X. Bai, S. Uhlig, R. Hubmayr, et al. 2004. DNA microarray analysis of gene expression in alveolar epithelial cells in response to TNF-, LPS and cyclic stretch. Physiol Genomics 19: 331.
Conflict of Interest
We declare that this study was financially supported by the Scientific Research Projects Committee, Rectorate of Afyon Kocatepe University, Afyonkarahisar, Turkey.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kokulu, S., Günay, E., Baki, E.D. et al. Impact of a Lung-Protective Ventilatory Strategy on Systemic and Pulmonary Inflammatory Responses During Laparoscopic Surgery: Is It Really Helpful?. Inflammation 38, 361–367 (2015). https://doi.org/10.1007/s10753-014-0039-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-0039-3