Abstract
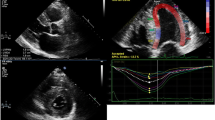
Cardiac involvement in amyloidosis is characterized by the extracellular deposition of misfolded proteins in the heart with the pathognomonic histological property of green birefringence when viewed under cross-polarized light after staining with Congo red. Although considered a rare disease, recent data suggest that cardiac amyloidosis is underappreciated as a cause of common cardiac diseases or syndromes. The prognosis for transthyretin (TTR) amyloidosis (ATTR) amyloidosis is better than that for amyloid light-chain amyloidosis; however, it is not as good as for other etiologies heart failure. Although there is no proven therapy for patients with ATTR cardiomyopathy (ATTR-CM), tafamidis meglumine, a TTR stabilizer, a study in 2018 found it was associated with reductions in all-cause mortality and cardiovascular-related hospitalizations, as well as with a reduction in the decline in functional capacity and quality of life compared with a placebo for patients with ATTR-CM. As a result of these findings, tafamidis meglumine is currently the only drug approved for patients with both wild-type and variant ATTR-CM, and should be considered for patients whose survival can be reasonably expected. In addition, recent advances in cardiac imaging, diagnostic strategies, and therapies have improved so that interest has been growing in the diagnosis of ATTR-CM by means of non-invasive imaging modalities as a potential means for better management of patients with ATTR-CM. This article reviews the efficacy of non-invasive imaging, especially echocardiography, cardiac magnetic imaging, and 99mTc-pyrophosphate scintigraphy for diagnosis of cardiac amyloidosis.









Similar content being viewed by others
References
Benson MD, Buxbaum JN, Eisenberg DS, Merlini G, Saraiva MJM, Sekijima Y, Sipe JD, Westermark P (2018) Amyloid nomenclature 2018: recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid 25(4):215–219. https://doi.org/10.1080/13506129.2018.1549825
Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C (2017) Addressing common questions encountered in the diagnosis and management of cardiac amyloidosis. Circulation 135(14):1357–1377. https://doi.org/10.1161/CIRCULATIONAHA.116.024438
Wechalekar AD, Gillmore JD, Hawkins PN (2016) Systemic amyloidosis. Lancet 387(10038):2641–2654. https://doi.org/10.1016/S0140-6736(15)01274-X
Garcia-Pavia P, Rapezzi C, Adler Y, Arad M, Basso C, Brucato A, Burazor I, Caforio ALP, Damy T, Eriksson U, Fontana M, Gillmore JD, Gonzalez-Lopez E, Grogan M, Heymans S, Imazio M, Kindermann I, Kristen AV, Maurer MS, Merlini G, Pantazis A, Pankuweit S, Rigopoulos AG, Linhart A (2021) Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur Heart J 42(16):1554–1568. https://doi.org/10.1093/eurheartj/ehab072
Ruberg FL, Grogan M, Hanna M, Kelly JW, Maurer MS (2019) Transthyretin amyloid cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol 73(22):2872–2891. https://doi.org/10.1016/j.jacc.2019.04.003
Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, Colby C, Laumann K, Zeldenrust SR, Leung N, Dingli D, Greipp PR, Lust JA, Russell SJ, Kyle RA, Rajkumar SV, Gertz MA (2012) Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 30(9):989–995. https://doi.org/10.1200/JCO.2011.38.5724
Kyle RA, Spittell PC, Gertz MA, Li CY, Edwards WD, Olson LJ, Thibodeau SN (1996) The premortem recognition of systemic senile amyloidosis with cardiac involvement. Am J Med 101(4):395–400. https://doi.org/10.1016/S0002-9343(96)00229-X
Ng B, Connors LH, Davidoff R, Skinner M, Falk RH (2005) Senile systemic amyloidosis presenting with heart failure: a comparison with light chain-associated amyloidosis. Arch Intern Med 165(12):1425–1429. https://doi.org/10.1001/archinte.165.12.1425
Connors LH, Sam F, Skinner M, Salinaro F, Sun F, Ruberg FL, Berk JL, Seldin DC (2016) Heart failure resulting from age-related cardiac amyloid disease associated with wild-type transthyretin: a prospective, observational cohort study. Circulation 133(3):282–290. https://doi.org/10.1161/CIRCULATIONAHA.115.018852
Grogan M, Scott CG, Kyle RA, Zeldenrust SR, Gertz MA, Lin G, Klarich KW, Miller WL, Maleszewski JJ, Dispenzieri A (2016) Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 68(10):1014–1020. https://doi.org/10.1016/j.jacc.2016.06.033
Yamashita T, Ando Y, Okamoto S, Misumi Y, Hirahara T, Ueda M, Obayashi K, Nakamura M, Jono H, Shono M, Asonuma K, Inomata Y, Uchino M (2012) Long-term survival after liver transplantation in patients with familial amyloid polyneuropathy. Neurology 78(9):637–643. https://doi.org/10.1212/WNL.0b013e318248df18
Koike H, Tanaka F, Hashimoto R, Tomita M, Kawagashira Y, Iijima M, Fujitake J, Kawanami T, Kato T, Yamamoto M, Sobue G (2012) Natural history of transthyretin Val30Met familial amyloid polyneuropathy: analysis of late-onset cases from non-endemic areas. J Neurol Neurosurg Psychiatry 83(2):152–158. https://doi.org/10.1136/jnnp-2011-301299
Wechalekar AD, Gillmore JD, Bird J, Cavenagh J, Hawkins S, Kazmi M, Lachmann HJ, Hawkins PN, Pratt G, Committee B (2015) Guidelines on the management of AL amyloidosis. Br J Haematol 168(2):186–206. https://doi.org/10.1111/bjh.13155
Klein AL, Hatle LK, Taliercio CP, Taylor CL, Kyle RA, Bailey KR, Seward JB, Tajik AJ (1990) Serial Doppler echocardiographic follow-up of left ventricular diastolic function in cardiac amyloidosis. J Am Coll Cardiol 16(5):1135–1141. https://doi.org/10.1016/0735-1097(90)90545-z
Swanton RH, Brooksby IA, Davies MJ, Coltart DJ, Jenkins BS, Webb-Peploe MM (1977) Systolic and diastolic ventricular function in cardiac amyloidosis. Studies in six cases diagnosed with endomyocardial biopsy. Am J Cardiol 39(5) 658-664. https://doi.org/10.1016/s0002-9149(77)80125-2
Dubrey S, Pollak A, Skinner M, Falk RH (1995) Atrial thrombi occurring during sinus rhythm in cardiac amyloidosis: evidence for atrial electromechanical dissociation. Br Heart J 74(5):541–544. https://doi.org/10.1136/hrt.74.5.541
Feng D, Syed IS, Martinez M, Oh JK, Jaffe AS, Grogan M, Edwards WD, Gertz MA, Klarich KW (2009) Intracardiac thrombosis and anticoagulation therapy in cardiac amyloidosis. Circulation 119(18):2490–2497. https://doi.org/10.1161/CIRCULATIONAHA.108.785014
Siqueira-Filho AG, Cunha CL, Tajik AJ, Seward JB, Schattenberg TT, Giuliani ER (1981) M-mode and two-dimensional echocardiographic features in cardiac amyloidosis. Circulation 63(1):188–196. https://doi.org/10.1161/01.cir.63.1.188
Selvanayagam JB, Hawkins PN, Paul B, Myerson SG, Neubauer S (2007) Evaluation and management of the cardiac amyloidosis. J Am Coll Cardiol 50(22):2101–2110. https://doi.org/10.1016/j.jacc.2007.08.028
Koyama J, Ray-Sequin PA, Davidoff R, Falk RH (2002) Usefulness of pulsed tissue Doppler imaging for evaluating systolic and diastolic left ventricular function in patients with AL (primary) amyloidosis. Am J Cardiol 89(9):1067–1071. https://doi.org/10.1016/s0002-9149(02)02277-4
Palka P, Lange A, Donnelly JE, Scalia G, Burstow DJ, Nihoyannopoulos P (2002) Doppler tissue echocardiographic features of cardiac amyloidosis. J Am Soc Echocardiogr 15(11):1353–1360. https://doi.org/10.1067/mje.2002.125285
Koyama J, Davidoff R, Falk RH (2004) Longitudinal myocardial velocity gradient derived from pulsed Doppler tissue imaging in AL amyloidosis: a sensitive indicator of systolic and diastolic dysfunction. J Am Soc Echocardiogr 17(1):36–44. https://doi.org/10.1016/j.echo.2003.09.014
Perugini E, Rapezzi C, Reggiani LB, Poole-Wilson P, Branzi A, Henein MY (2005) Comparison of ventricular long-axis function in patients with cardiac amyloidosis versus idiopathic restrictive cardiomyopathy. Am J Cardiol 95(1):146–149. https://doi.org/10.1016/j.amjcard.2004.08.084
Tanaka H (2019) Utility of strain imaging in conjunction with heart failure stage classification for heart failure patient management. J Echocardiogr 17(1):17–24. https://doi.org/10.1007/s12574-018-0408-2
Tanaka H (2021) Efficacy of echocardiography for differential diagnosis of left ventricular hypertrophy: special focus on speckle-tracking longitudinal strain. J Echocardiogr 19(2):71–79. https://doi.org/10.1007/s12574-020-00508-3
Gorcsan J 3rd, Tanaka H (2011) Echocardiographic assessment of myocardial strain. J Am Coll Cardiol 58(14):1401–1413. https://doi.org/10.1016/j.jacc.2011.06.038
Biering-Sorensen T, Biering-Sorensen SR, Olsen FJ, Sengelov M, Jorgensen PG, Mogelvang R, Shah AM, Jensen JS (2017) Global longitudinal strain by echocardiography predicts long-term risk of cardiovascular morbidity and mortality in a low-risk general population: the Copenhagen City Heart Study. Circ Cardiovasc Imaging 10(3). https://doi.org/10.1161/CIRCIMAGING.116.005521
Stanton T, Leano R, Marwick TH (2009) Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoring. Circ Cardiovasc Imaging 2(5):356–364. https://doi.org/10.1161/CIRCIMAGING.109.862334
Phelan D, Collier P, Thavendiranathan P, Popovic ZB, Hanna M, Plana JC, Marwick TH, Thomas JD (2012) Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 98(19):1442–1448. https://doi.org/10.1136/heartjnl-2012-302353
Liu D, Hu K, Niemann M, Herrmann S, Cikes M, Stork S, Beer M, Gaudron PD, Morbach C, Knop S, Geissinger E, Ertl G, Bijnens B, Weidemann F (2013) Impact of regional left ventricular function on outcome for patients with AL amyloidosis. PLoS One 8(3):e56923. https://doi.org/10.1371/journal.pone.0056923
Liu D, Hu K, Niemann M, Herrmann S, Cikes M, Stork S, Gaudron PD, Knop S, Ertl G, Bijnens B, Weidemann F (2013) Effect of combined systolic and diastolic functional parameter assessment for differentiation of cardiac amyloidosis from other causes of concentric left ventricular hypertrophy. Circ Cardiovasc Imaging 6(6):1066–1072. https://doi.org/10.1161/CIRCIMAGING.113.000683
Tuzovic M, Yang EH, Baas AS, Depasquale EC, Deng MC, Cruz D, Vorobiof G (2017) Cardiac Amyloidosis: Diagnosis and Treatment Strategies. Curr Oncol Rep 19(7):46. https://doi.org/10.1007/s11912-017-0607-4
Barros-Gomes S, Williams B, Nhola LF, Grogan M, Maalouf JF, Dispenzieri A, Pellikka PA, Villarraga HR (2017) Prognosis of light chain amyloidosis with preserved LVEF: added value of 2D speckle-tracking echocardiography to the current prognostic staging system. JACC Cardiovasc Imaging 10(4):398–407. https://doi.org/10.1016/j.jcmg.2016.04.008
Dungu JN, Valencia O, Pinney JH, Gibbs SD, Rowczenio D, Gilbertson JA, Lachmann HJ, Wechalekar A, Gillmore JD, Whelan CJ, Hawkins PN, Anderson LJ (2014) CMR-based differentiation of AL and ATTR cardiac amyloidosis. JACC Cardiovasc Imaging 7(2):133–142. https://doi.org/10.1016/j.jcmg.2013.08.015
Fattori R, Rocchi G, Celletti F, Bertaccini P, Rapezzi C, Gavelli G (1998) Contribution of magnetic resonance imaging in the differential diagnosis of cardiac amyloidosis and symmetric hypertrophic cardiomyopathy. Am Heart J 136(5):824–830. https://doi.org/10.1016/s0002-8703(98)70127-9
Martinez-Naharro A, Treibel TA, Abdel-Gadir A, Bulluck H, Zumbo G, Knight DS, Kotecha T, Francis R, Hutt DF, Rezk T, Rosmini S, Quarta CC, Whelan CJ, Kellman P, Gillmore JD, Moon JC, Hawkins PN, Fontana M (2017) Magnetic resonance in transthyretin cardiac amyloidosis. J Am Coll Cardiol 70(4):466–477. https://doi.org/10.1016/j.jacc.2017.05.053
Maceira AM, Prasad SK, Hawkins PN, Roughton M, Pennell DJ (2008) Cardiovascular magnetic resonance and prognosis in cardiac amyloidosis. J Cardiovasc Magn Reson 10(54). https://doi.org/10.1186/1532-429X-10-54
Syed IS, Glockner JF, Feng D, Araoz PA, Martinez MW, Edwards WD, Gertz MA, Dispenzieri A, Oh JK, Bellavia D, Tajik AJ, Grogan M (2010) Role of cardiac magnetic resonance imaging in the detection of cardiac amyloidosis. JACC Cardiovasc Imaging 3(2):155–164. https://doi.org/10.1016/j.jcmg.2009.09.023
Wan K, Sun J, Yang D, Liu H, Wang J, Cheng W, Zhang Q, Zeng Z, Zhang T, Greiser A, Jolly MP, Han Y, Chen Y (2018) Left ventricular myocardial deformation on cine MR images: relationship to severity of disease and prognosis in light-chain amyloidosis. Radiology 288(1):73–80. https://doi.org/10.1148/radiol.2018172435
Fontana M, Pica S, Reant P, Abdel-Gadir A, Treibel TA, Banypersad SM, Maestrini V, Barcella W, Rosmini S, Bulluck H, Sayed RH, Patel K, Mamhood S, Bucciarelli-Ducci C, Whelan CJ, Herrey AS, Lachmann HJ, Wechalekar AD, Manisty CH, Schelbert EB, Kellman P, Gillmore JD, Hawkins PN, Moon JC (2015) Prognostic value of late gadolinium enhancement cardiovascular magnetic resonance in cardiac amyloidosis. Circulation 132(16):1570–1579. https://doi.org/10.1161/CIRCULATIONAHA.115.016567
Fontana M, Banypersad SM, Treibel TA, Maestrini V, Sado DM, White SK, Pica S, Castelletti S, Piechnik SK, Robson MD, Gilbertson JA, Rowczenio D, Hutt DF, Lachmann HJ, Wechalekar AD, Whelan CJ, Gillmore JD, Hawkins PN, Moon JC (2014) Native T1 mapping in transthyretin amyloidosis. JACC Cardiovasc Imaging 7(2):157–165. https://doi.org/10.1016/j.jcmg.2013.10.008
Karamitsos TD, Piechnik SK, Banypersad SM, Fontana M, Ntusi NB, Ferreira VM, Whelan CJ, Myerson SG, Robson MD, Hawkins PN, Neubauer S, Moon JC (2013) Noncontrast T1 mapping for the diagnosis of cardiac amyloidosis. JACC Cardiovasc Imaging 6(4):488–497. https://doi.org/10.1016/j.jcmg.2012.11.013
Martinez-Naharro A, Kotecha T, Norrington K, Boldrini M, Rezk T, Quarta C, Treibel TA, Whelan CJ, Knight DS, Kellman P, Ruberg FL, Gillmore JD, Moon JC, Hawkins PN, Fontana M (2019) Native T1 and extracellular volume in transthyretin amyloidosis. JACC Cardiovasc Imaging 12(5):810–819. https://doi.org/10.1016/j.jcmg.2018.02.006
Dorbala S, Ando Y, Bokhari S, Dispenzieri A, Falk RH, Ferrari VA, Fontana M, Gheysens O, Gillmore JD, Glaudemans A, Hanna MA, Hazenberg BPC, Kristen AV, Kwong RY, Maurer MS, Merlini G, Miller EJ, Moon JC, Murthy VL, Quarta CC, Rapezzi C, Ruberg FL, Shah SJ, Slart R, Verberne HJ, Bourque JM (2019) ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: Part 1 of 2-evidence base and standardized methods of imaging. J Nucl Cardiol 26(6):2065–2123. https://doi.org/10.1007/s12350-019-01760-6
Gillmore JD, Maurer MS, Falk RH, Merlini G, Damy T, Dispenzieri A, Wechalekar AD, Berk JL, Quarta CC, Grogan M, Lachmann HJ, Bokhari S, Castano A, Dorbala S, Johnson GB, Glaudemans AW, Rezk T, Fontana M, Palladini G, Milani P, Guidalotti PL, Flatman K, Lane T, Vonberg FW, Whelan CJ, Moon JC, Ruberg FL, Miller EJ, Hutt DF, Hazenberg BP, Rapezzi C, Hawkins PN (2016) Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 133(24):2404–2412. https://doi.org/10.1161/CIRCULATIONAHA.116.021612
Castano A, Haq M, Narotsky DL, Goldsmith J, Weinberg RL, Morgenstern R, Pozniakoff T, Ruberg FL, Miller EJ, Berk JL, Dispenzieri A, Grogan M, Johnson G, Bokhari S, Maurer MS (2016) Multicenter study of planar technetium 99m pyrophosphate cardiac imaging: predicting survival for patients with ATTR cardiac amyloidosis. JAMA Cardiol 1(8):880–889. https://doi.org/10.1001/jamacardio.2016.2839
Hahn VS, Yanek LR, Vaishnav J, Ying W, Vaidya D, Lee YZJ, Riley SJ, Subramanya V, Brown EE, Hopkins CD, Ononogbu S, Perzel Mandell K, Halushka MK, Steenbergen C Jr, Rosenberg AZ, Tedford RJ, Judge DP, Shah SJ, Russell SD, Kass DA, Sharma K (2020) Endomyocardial biopsy characterization of heart failure with preserved ejection fraction and prevalence of cardiac amyloidosis. JACC Heart Fail 8(9):712–724. https://doi.org/10.1016/j.jchf.2020.04.007
Gonzalez-Lopez E, Gallego-Delgado M, Guzzo-Merello G, de Haro-Del Moral FJ, Cobo-Marcos M, Robles C, Bornstein B, Salas C, Lara-Pezzi E, Alonso-Pulpon L, Garcia-Pavia P (2015) Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J 36(38):2585–2594. https://doi.org/10.1093/eurheartj/ehv338
Castano A, Narotsky DL, Hamid N, Khalique OK, Morgenstern R, DeLuca A, Rubin J, Chiuzan C, Nazif T, Vahl T, George I, Kodali S, Leon MB, Hahn R, Bokhari S, Maurer MS (2017) Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur Heart J 38(38):2879–2887. https://doi.org/10.1093/eurheartj/ehx350
Nitsche C, Scully PR, Patel KP, Kammerlander AA, Koschutnik M, Dona C, Wollenweber T, Ahmed N, Thornton GD, Kelion AD, Sabharwal N, Newton JD, Ozkor M, Kennon S, Mullen M, Lloyd G, Fontana M, Hawkins PN, Pugliese F, Menezes LJ, Moon JC, Mascherbauer J, Treibel TA (2021) Prevalence and outcomes of concomitant aortic stenosis and cardiac amyloidosis. J Am Coll Cardiol 77(2):128–139. https://doi.org/10.1016/j.jacc.2020.11.006
Lee SP, Lee ES, Choi H, Im HJ, Koh Y, Lee MH, Kwon JH, Paeng JC, Kim HK, Cheon GJ, Kim YJ, Kim I, Yoon SS, Seo JW, Sohn DW (2015) 11C-Pittsburgh B PET imaging in cardiac amyloidosis. JACC Cardiovasc Imaging 8(1):50–59. https://doi.org/10.1016/j.jcmg.2014.09.018
Park MA, Padera RF, Belanger A, Dubey S, Hwang DH, Veeranna V, Falk RH, Di Carli MF, Dorbala S (2015) 18F-Florbetapir binds specifically to myocardial light chain and transthyretin amyloid deposits: autoradiography study. Circ Cardiovasc Imaging 8(8). https://doi.org/10.1161/CIRCIMAGING.114.002954
Law WP, Wang WY, Moore PT, Mollee PN, Ng AC (2016) Cardiac amyloid imaging with 18F-Florbetaben PET: a pilot study. J Nucl Med 57(11):1733–1739. https://doi.org/10.2967/jnumed.115.169870
Bandula S, White SK, Flett AS, Lawrence D, Pugliese F, Ashworth MT, Punwani S, Taylor SA, Moon JC (2013) Measurement of myocardial extracellular volume fraction by using equilibrium contrast-enhanced CT: validation against histologic findings. Radiology 269(2):396–403. https://doi.org/10.1148/radiol.13130130
Oda S, Emoto T, Nakaura T, Kidoh M, Utsunomiya D, Funama Y, Nagayama Y, Takashio S, Ueda M, Yamashita T, Tsujita K, Ando Y, Yamashita Y (2019) Myocardial late iodine enhancement and extracellular volume quantification with dual-layer spectral detector dual-energy cardiac CT. Radiol Cardiothorac Imaging 1(1):e180003. https://doi.org/10.1148/ryct.2019180003
Scully PR, Patel KP, Saberwal B, Klotz E, Augusto JB, Thornton GD, Hughes RK, Manisty C, Lloyd G, Newton JD, Sabharwal N, Kelion A, Kennon S, Ozkor M, Mullen M, Hartman N, Cavalcante JL, Menezes LJ, Hawkins PN, Treibel TA, Moon JC, Pugliese F (2020) Identifying cardiac amyloid in aortic stenosis: ECV quantification by CT in TAVR Patients. JACC Cardiovasc Imaging 13(10):2177–2189. https://doi.org/10.1016/j.jcmg.2020.05.029
Acknowledgments
I thank Dr. Takayoshi Toba and Yu Izawa in the Kobe University Hospital for the support of CMR, 99mTc-PYP scintigraphy, and cardiac CT.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tanaka, H. Illustrative review of cardiac amyloidosis by multimodality imaging. Heart Fail Rev 28, 113–122 (2023). https://doi.org/10.1007/s10741-022-10245-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-022-10245-7