Abstract
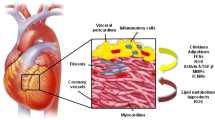
Heart failure is a growing health problem resulting in the decreased life expectancy of patients and severely increased the healthcare burden. Penetrating research on the pathogenesis and regulation mechanism of heart failure is important for treatment of heart failure. Epicardial adipose tissue (EAT) has been demonstrated as not only a dynamic organ with biological functions but also an inert lipid store with regulating systemic metabolism. EAT mediates physiological and pathophysiological processes of heart failure by regulating adipogenesis, cardiac remodeling, insulin resistance, cardiac output, and renin angiotensin aldosterone system (RAAS). Moreover, EAT secretes a wide range of adipokines, adrenomedullin, adiponectin, and miRNAs through paracrine, endocrine, and vasocrine pathways, which involve in various extracellular and intracellular mechanism of cardiac-related cells in the progress of cardiovascular disease especially in heart failure. Nevertheless, mechanisms and roles of EAT on heart failure are barely summarized. Understanding the regulating mechanisms of EAT on heart failure may give rise to novel therapeutic targets and will open up innovative strategies to myocardial injury as well as in heart failure.

Similar content being viewed by others
Abbreviations
- EAT:
-
Epicardial adipose tissue
- RAAS:
-
Renin angiotensin aldosterone system
- WAT:
-
White adipose tissue
- BAT:
-
Brown adipose tissue
- FFA:
-
Free fatty acid
- LV:
-
Left ventricle
- BMI:
-
Body mass index
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure patients with reduced ejection fraction
- ROS:
-
Reactive oxygen species
- AM:
-
Adrenomedullin
- cAMP:
-
Cyclic adenosine monophosphate
- NO:
-
Nitric oxide
- miRNAs:
-
MicroRNAs
References
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602
Rech M, Barandiarán Aizpurua A, van Empel V, van Bilsen M, Schroen B (2018) Pathophysiological understanding of HFpEF: microRNAs as part of the puzzle. Cardiovasc Res 114(6):782–793
Yamamoto E, Hirata Y, Tokitsu T, Kusaka H, Tabata N, Tsujita K, Yamamuro M, Kaikita K, Watanabe H, Hokimoto S, Maruyama T, Ogawa H (2016) The clinical significance of plasma neopterin in heart failure with preserved left ventricular ejection fraction. ESC Heart Fail 3(1):53–59
Gonzalez N et al (2017) Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc Diabetol 16(1):44
Murdolo G, Angeli F, Reboldi G, di Giacomo L, Aita A, Bartolini C, Vedecchia P (2015) Left ventricular hypertrophy and obesity: only a matter of fat? High Blood Press Cardiovasc Prev 22(1):29–41
Karmazyn M, Purdham DM, Rajapurohitam V, Zeidan A (2008) Signalling mechanisms underlying the metabolic and other effects of adipokines on the heart. Cardiovasc Res 79(2):279–286
Bjorndal B et al (2011) Different adipose depots: their role in the development of metabolic syndrome and mitochondrial response to hypolipidemic agents. J Obes 2011:490650
Patel VB, Shah S, Verma S, Oudit GY (2017) Epicardial adipose tissue as a metabolic transducer: role in heart failure and coronary artery disease. Heart Fail Rev 22(6):889–902
Sethi JK, Vidal-Puig AJ (2007) Thematic review series: adipocyte biology. Adipose tissue function and plasticity orchestrate nutritional adaptation. J Lipid Res 48(6):1253–1262
Iozzo P (2011) Myocardial, perivascular, and epicardial fat. Diabetes Care 34(Suppl 2):S371–S379
Piano MR, Phillips SA (2014) Alcoholic cardiomyopathy: pathophysiologic insights. Cardiovasc Toxicol 14(4):291–308
Srikanthan K, Shapiro JI, Sodhi K (2016) The role of Na/K-ATPase signaling in oxidative stress related to obesity and cardiovascular disease. Molecules 21(9):1–13
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH, American Heart Association, Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism (2006) Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity Committee of the Council on nutrition, physical activity, and metabolism. Circulation 113(6):898–918
Kenchaiah S, Evans JC, Levy D, Wilson PWF, Benjamin EJ, Larson MG, Kannel WB, Vasan RS (2002) Obesity and the risk of heart failure. N Engl J Med 347(5):305–313
Lauer MS, Anderson KM, Kannel WB, Levy D (1991) The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA 266(2):231–236
Alpert MA, Lambert CR, Terry BE, Cohen MV, Mukerji V, Massey CV, Hashimi MW, Panayiotou H (1995) Influence of left ventricular mass on left ventricular diastolic filling in normotensive morbid obesity. Am Heart J 130(5):1068–1073
Dua S, Bhuker M, Sharma P, Dhall M, Kapoor S (2014) Body mass index relates to blood pressure among adults. N Am J Med Sci 6(2):89–95
Wong C, Marwick TH (2007) Obesity cardiomyopathy: pathogenesis and pathophysiology. Nat Clin Pract Cardiovasc Med 4(8):436–443
Lumeng CN, Bodzin JL, Saltiel AR (2007) Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest 117(1):175–184
Chrysant SG, Chrysant GS (2019) Obesity-related heart failure with preserved ejection fraction: new treatment strategies. Hosp Pract (1995) 47(2):67–72
Boudina S, Sena S, Theobald H, Sheng X, Wright JJ, Hu XX, Aziz S, Johnson JI, Bugger H, Zaha VG, Abel ED (2007) Mitochondrial energetics in the heart in obesity-related diabetes: direct evidence for increased uncoupled respiration and activation of uncoupling proteins. Diabetes 56(10):2457–2466
Patel VB, Mori J, McLean B, Basu R, Das SK, Ramprasath T, Parajuli N, Penninger JM, Grant MB, Lopaschuk GD, Oudit GY (2016) ACE2 deficiency worsens epicardial adipose tissue inflammation and cardiac dysfunction in response to diet-induced obesity. Diabetes 65(1):85–95
Boudina S, Han YH, Pei S, Tidwell TJ, Henrie B, Tuinei J, Olsen C, Sena S, Abel ED (2012) UCP3 regulates cardiac efficiency and mitochondrial coupling in high fat-fed mice but not in leptin-deficient mice. Diabetes 61(12):3260–3269
Drosatos K, Schulze PC (2013) Cardiac lipotoxicity: molecular pathways and therapeutic implications. Curr Heart Fail Rep 10(2):109–121
Aroor AR, Mandavia CH, Sowers JR (2012) Insulin resistance and heart failure: molecular mechanisms. Heart Fail Clin 8(4):609–617
Zhang L, Jaswal JS, Ussher JR, Sankaralingam S, Wagg C, Zaugg M, Lopaschuk GD (2013) Cardiac insulin-resistance and decreased mitochondrial energy production precede the development of systolic heart failure after pressure-overload hypertrophy. Circ Heart Fail 6(5):1039–1048
de Ferranti S, Mozaffarian D (2008) The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem 54(6):945–955
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444(7121):860–867
Talman AH, Psaltis PJ, Cameron JD, Meredith IT, Seneviratne SK, Wong DT (2014) Epicardial adipose tissue: far more than a fat depot. Cardiovasc Diagn Ther 4(6):416–429
Iacobellis G, Corradi D, Sharma AM (2005) Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med 2(10):536–543
Kankaanpaa M et al (2006) Myocardial triglyceride content and epicardial fat mass in human obesity: relationship to left ventricular function and serum free fatty acid levels. J Clin Endocrinol Metab 91(11):4689–4695
Corradi D, Maestri R, Callegari S, Pastori P, Goldoni M, Luong TV, Bordi C (2004) The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts. Cardiovasc Pathol 13(6):313–316
Company JM et al (2010) Epicardial fat gene expression after aerobic exercise training in pigs with coronary atherosclerosis: relationship to visceral and subcutaneous fat. J Appl Physiol (1985) 109(6):1904–1912
Matloch Z, Kotulak T, Haluzik M (2016) The role of epicardial adipose tissue in heart disease. Physiol Res 65(1):23–32
Pang C, Gao Z, Yin J, Zhang J, Jia W, Ye J (2008) Macrophage infiltration into adipose tissue may promote angiogenesis for adipose tissue remodeling in obesity. Am J Physiol Endocrinol Metab 295(2):E313–E322
Henrichot E, Juge-Aubry CE, Pernin À, Pache JC, Velebit V, Dayer JM, Meda P, Chizzolini C, Meier CA (2005) Production of chemokines by perivascular adipose tissue: a role in the pathogenesis of atherosclerosis? Arterioscler Thromb Vasc Biol 25(12):2594–2599
Katz AM, Lorell BH (2000) Regulation of cardiac contraction and relaxation. Circulation 102(20 Suppl 4):IV69–IV74
Zeller J, Krüger C, Lamounier-Zepter V, Sag S, Strack C, Mohr M, Loew T, Schmitz G, Maier L, Fischer M, Baessler A (2019) The adipo-fibrokine activin A is associated with metabolic abnormalities and left ventricular diastolic dysfunction in obese patients. ESC Heart Fail 6(2):362–370
Burgeiro A, Fuhrmann A, Cherian S, Espinoza D, Jarak I, Carvalho RA, Loureiro M, Patrício M, Antunes M, Carvalho E (2016) Glucose uptake and lipid metabolism are impaired in epicardial adipose tissue from heart failure patients with or without diabetes. Am J Physiol Endocrinol Metab 310(7):E550–E564
Ritchie RH (2009) Evidence for a causal role of oxidative stress in the myocardial complications of insulin resistance. Heart Lung Circ 18(1):11–18
Fosshaug LE, Dahl CP, Risnes I, Bohov P, Berge RK, Nymo S, Geiran O, Yndestad A, Gullestad L, Aukrust P, Vinge LE, Øie E (2015) Altered levels of fatty acids and inflammatory and metabolic mediators in epicardial adipose tissue in patients with systolic heart failure. J Card Fail 21(11):916–923
Neel JV (1999) Diabetes mellitus: a "thrifty" genotype rendered detrimental by "progress"? 1962. Bull World Health Organ 77(8):694–703 discussion 692-3
Reingold JS, McGavock JM, Kaka S, Tillery T, Victor RG, Szczepaniak LS (2005) Determination of triglyceride in the human myocardium by magnetic resonance spectroscopy: reproducibility and sensitivity of the method. Am J Physiol Endocrinol Metab 289(5):E935–E939
Karastergiou K, Evans I, Ogston N, Miheisi N, Nair D, Kaski JC, Jahangiri M, Mohamed-Ali V (2010) Epicardial adipokines in obesity and coronary artery disease induce atherogenic changes in monocytes and endothelial cells. Arterioscler Thromb Vasc Biol 30(7):1340–1346
Sacks HS, Fain JN (2011) Human epicardial fat: what is new and what is missing? Clin Exp Pharmacol Physiol 38(12):879–887
de Feyter PJ (2011) Epicardial adipose tissue: an emerging role for the development of coronary atherosclerosis. Clin Cardiol 34(3):143–144
Iacobellis G, Bianco AC (2011) Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab 22(11):450–457
Iacobellis G (2015) Local and systemic effects of the multifaceted epicardial adipose tissue depot. Nat Rev Endocrinol 11(6):363–371
Mazurek T, Zhang LF, Zalewski A, Mannion JD, Diehl JT, Arafat H, Sarov-Blat L, O’Brien S, Keiper EA, Johnson AG, Martin J, Goldstein BJ, Shi Y (2003) Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 108(20):2460–2466
Cherian S, Lopaschuk GD, Carvalho E (2012) Cellular cross-talk between epicardial adipose tissue and myocardium in relation to the pathogenesis of cardiovascular disease. Am J Physiol Endocrinol Metab 303(8):E937–E949
Drevon CA (2005) Fatty acids and expression of adipokines. Biochim Biophys Acta 1740(2):287–292
Shibasaki I, Nishikimi T, Mochizuki Y, Yamada Y, Yoshitatsu M, Inoue Y, Kuwata T, Ogawa H, Tsuchiya G, Ishimitsu T, Fukuda H (2010) Greater expression of inflammatory cytokines, adrenomedullin, and natriuretic peptide receptor-C in epicardial adipose tissue in coronary artery disease. Regul Pept 165(2–3):210–217
Peacock WF (2014) Novel biomarkers in acute heart failure: MR-pro-adrenomedullin. Clin Chem Lab Med 52(10):1433–1435
Kitamura K, Sakata J, Kangawa K, Kojima M, Matsuo H, Eto T (1993) Cloning and characterization of cDNA encoding a precursor for human adrenomedullin. Biochem Biophys Res Commun 194(2):720–725
Voors AA, Kremer D, Geven C, ter Maaten JM, Struck J, Bergmann A, Pickkers P, Metra M, Mebazaa A, Düngen HD, Butler J (2019) Adrenomedullin in heart failure: pathophysiology and therapeutic application. Eur J Heart Fail 21(2):163–171
Silaghi A, Achard V, Paulmyer-Lacroix O, Scridon T, Tassistro V, Duncea I, Clément K, Dutour A, Grino M (2007) Expression of adrenomedullin in human epicardial adipose tissue: role of coronary status. Am J Physiol Endocrinol Metab 293(5):E1443–E1450
Yuan M, Wang Q, Li C, Tao L, Zhang H, Wang H, Zhang Y, Ren J (2015) Adrenomedullin in vascular endothelial injury and combination therapy: time for a new paradigm. Curr Vasc Pharmacol 13(4):459–466
Benigni A, Cassis P, Remuzzi G (2010) Angiotensin II revisited: new roles in inflammation, immunology and aging. EMBO Mol Med 2(7):247–257
Ribatti D, Nico B, Spinazzi R, Vacca A, Nussdorfer GG (2005) The role of adrenomedullin in angiogenesis. Peptides 26(9):1670–1675
Nagy JA, Benjamin L, Zeng H, Dvorak AM, Dvorak HF (2008) Vascular permeability, vascular hyperpermeability and angiogenesis. Angiogenesis 11(2):109–119
Rohrbach S, Troidl C, Hamm C, Schulz R (2015) Ischemia and reperfusion related myocardial inflammation: a network of cells and mediators targeting the cardiomyocyte. IUBMB Life 67(2):110–119
Hamid SA, Baxter GF (2005) Adrenomedullin: regulator of systemic and cardiac homeostasis in acute myocardial infarction. Pharmacol Ther 105(2):95–112
Li LL, Peng C, Zhang M, Liu Y, Li H, Chen H, Sun Y, Zhu C, Zhang Y (2018) Mesenchymal stem cells overexpressing adrenomedullin improve heart function through antifibrotic action in rats experiencing heart failure. Mol Med Rep 17(1):1437–1444
Zhang Y, Xu Y, Ma J, Pang X, Dong M (2017) Adrenomedullin promotes angiogenesis in epithelial ovarian cancer through upregulating hypoxia-inducible factor-1alpha and vascular endothelial growth factor. Sci Rep 7:40524
Eleuteri E, Mezzani A, di Stefano A, Vallese D, Gnemmi I, Delle Donne L, Taddeo A, Della Bella S, Giannuzzi P (2013) Aerobic training and angiogenesis activation in patients with stable chronic heart failure: a preliminary report. Biomarkers 18(5):418–424
Chen H, Montagnani M, Funahashi T, Shimomura I, Quon MJ (2003) Adiponectin stimulates production of nitric oxide in vascular endothelial cells. J Biol Chem 278(45):45021–45026
Ouchi N, Kihara S, Arita Y, Maeda K, Kuriyama H, Okamoto Y, Hotta K, Nishida M, Takahashi M, Nakamura T, Yamashita S, Funahashi T, Matsuzawa Y (1999) Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein adiponectin. Circulation 100(25):2473–2476
Villarreal-Molina MT, Antuna-Puente B (2012) Adiponectin: anti-inflammatory and cardioprotective effects. Biochimie 94(10):2143–2149
Antonopoulos AS, Margaritis M, Coutinho P, Digby J, Patel R, Psarros C, Ntusi N, Karamitsos TD, Lee R, de Silva R, Petrou M, Sayeed R, Demosthenous M, Bakogiannis C, Wordsworth PB, Tousoulis D, Neubauer S, Channon KM, Antoniades C (2014) Reciprocal effects of systemic inflammation and brain natriuretic peptide on adiponectin biosynthesis in adipose tissue of patients with ischemic heart disease. Arterioscler Thromb Vasc Biol 34(9):2151–2159
Kistorp C, Faber J, Galatius S, Gustafsson F, Frystyk J, Flyvbjerg A, Hildebrandt P (2005) Plasma adiponectin, body mass index, and mortality in patients with chronic heart failure. Circulation 112(12):1756–1762
Sente T, van Berendoncks AM, Hoymans VY, Vrints CJ (2016) Adiponectin resistance in skeletal muscle: pathophysiological implications in chronic heart failure. J Cachexia Sarcopenia Muscle 7(3):261–274
George J, Patal S, Wexler D, Sharabi Y, Peleg E, Kamari Y, Grossman E, Sheps D, Keren G, Roth A (2006) Circulating adiponectin concentrations in patients with congestive heart failure. Heart 92(10):1420–1424
Rathmann W, Herder C (2007) Adiponectin and cardiovascular mortality: evidence for "reverse epidemiology". Horm Metab Res 39(1):1–2
Yamauchi T, Kadowaki T (2013) Adiponectin receptor as a key player in healthy longevity and obesity-related diseases. Cell Metab 17(2):185–196
Park M, Sweeney G (2013) Direct effects of adipokines on the heart: focus on adiponectin. Heart Fail Rev 18(5):631–644
Shibata R, Sato K, Pimentel DR, Takemura Y, Kihara S, Ohashi K, Funahashi T, Ouchi N, Walsh K (2005) Adiponectin protects against myocardial ischemia-reperfusion injury through AMPK- and COX-2-dependent mechanisms. Nat Med 11(10):1096–1103
Chakraborti CK (2015) Role of adiponectin and some other factors linking type 2 diabetes mellitus and obesity. World J Diabetes 6(15):1296–1308
Shibata R, Ouchi N, Murohara T (2009) Adiponectin and cardiovascular disease. Circ J 73(4):608–614
Yoon MJ, Lee GY, Chung JJ, Ahn YH, Hong SH, Kim JB (2006) Adiponectin increases fatty acid oxidation in skeletal muscle cells by sequential activation of AMP-activated protein kinase, p38 mitogen-activated protein kinase, and peroxisome proliferator-activated receptor alpha. Diabetes 55(9):2562–2570
Agra RM, Fernández-Trasancos Á, Díaz-Rodríguez E, Cordero A, Varela-Román A, Gómez-Otero I, Canoa JNL, Fernández ÁL, Martínez-Cereijo JM, González-Juanatey JR, Eiras S (2018) Nutrients restriction upregulates adiponectin in epicardial or subcutaneous adipose tissue: impact in de novo heart failure patients. Int J Med Sci 15(5):417–424
Delporte ML, Brichard SM, Hermans MP, Beguin C, Lambert M (2003) Hyperadiponectinaemia in anorexia nervosa. Clin Endocrinol 58(1):22–29
Thomou T, Mori MA, Dreyfuss JM, Konishi M, Sakaguchi M, Wolfrum C, Rao TN, Winnay JN, Garcia-Martin R, Grinspoon SK, Gorden P, Kahn CR (2017) Adipose-derived circulating miRNAs regulate gene expression in other tissues. Nature 542(7642):450–455
Vegter EL, van der Meer P, de Windt LJ, Pinto YM, Voors AA (2016) MicroRNAs in heart failure: from biomarker to target for therapy. Eur J Heart Fail 18(5):457–468
Iacobellis G, Leonetti F, Singh N, M Sharma A (2007) Relationship of epicardial adipose tissue with atrial dimensions and diastolic function in morbidly obese subjects. Int J Cardiol 115(2):272–273
Tran KV, Majka J, Sanghai S, Sardana M, Lessard D, Milstone Z, Tanriverdi K, Freedman JE, Fitzgibbons TP, McManus D (2019) Micro-RNAs are related to epicardial adipose tissue in participants with atrial fibrillation: data from the MiRhythm study. Front Cardiovasc Med 6:115
Charrier H, Cuvelliez M, Dubois-Deruy E, Mulder P, Richard V, Bauters C, Pinet F (2019) Integrative system biology analyses identify seven microRNAs to predict heart failure. Noncoding RNA 5(1):1–9
Price NL, Fernandez-Hernando C (2016) miRNA regulation of white and brown adipose tissue differentiation and function. Biochim Biophys Acta 1861(12 Pt B):2104–2110
Oclon E et al (2016) Hyperglycemia-induced changes in miRNA expression patterns in epicardial adipose tissue of piglets. J Endocrinol 229(3):259–266
Bar C, Thum T, de Gonzalo-Calvo D (2019) Circulating miRNAs as mediators in cell-to-cell communication. Epigenomics 11(2):111–113
Liang H, Zhang C, Ban T, Liu Y, Mei L, Piao X, Zhao D, Lu Y, Chu W, Yang B (2012) A novel reciprocal loop between microRNA-21 and TGFbetaRIII is involved in cardiac fibrosis. Int J Biochem Cell Biol 44(12):2152–2160
Long B, Gan TY, Zhang RC, Zhang YH (2017) miR-23a regulates cardiomyocyte apoptosis by targeting manganese superoxide dismutase. Mol Cells 40(8):542–549
Yang L, Wang B, Zhou Q, Wang Y, Liu X, Liu Z, Zhan Z (2018) MicroRNA-21 prevents excessive inflammation and cardiac dysfunction after myocardial infarction through targeting KBTBD7. Cell Death Dis 9(7):769
Hilton C, Neville MJ, Karpe F (2013) MicroRNAs in adipose tissue: their role in adipogenesis and obesity. Int J Obes 37(3):325–332
de Gonzalo-Calvo D, Vilades D, Martinez-Camblor P, Vea A, Ferrero-Gregori A, Nasarre L, Bornachea O, Sanchez Vega J, Leta R, Puig N, Benitez S, Sanchez-Quesada JL, Carreras F, Llorente-Cortes, V (2019) Plasma microRNA profiling reveals novel biomarkers of epicardial adipose tissue: a multidetector computed tomography study. J Clin Med 8(6):1–9
Karbiener M, Fischer C, Nowitsch S, Opriessnig P, Papak C, Ailhaud G, Dani C, Amri EZ, Scheideler M (2009) microRNA miR-27b impairs human adipocyte differentiation and targets PPARgamma. Biochem Biophys Res Commun 390(2):247–251
Zhu Y et al (2014) miR-27 inhibits adipocyte differentiation via suppressing CREB expression. Acta Biochim Biophys Sin (Shanghai) 46(7):590–596
Omran A, Elimam D, Webster KA, Shehadeh LA, Yin F (2013) MicroRNAs: a new piece in the paediatric cardiovascular disease puzzle. Cardiol Young 23(5):642–655
Funding
This study was supported by a Joint Fund for Science and Technology Cooperation across the Taiwan Straits from the National Natural Science Foundation and Fujian Province, China (Grant No. U1605226), and a Science and Technology Project from Xiamen Science and Technology Bureau, Fujian Province, China (Grant No. 3502Z20184025).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Song, Y., Song, F., Wu, C. et al. The roles of epicardial adipose tissue in heart failure. Heart Fail Rev 27, 369–377 (2022). https://doi.org/10.1007/s10741-020-09997-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-020-09997-x